What Desserts Can You Eat With Ulcerative Colitis Recipe Ideas
Just about everybody enjoys a sweet treat now and then, but if youre living with ulcerative colitis, it can be tough to decide what to eat and when. Can you eat dessert at all? If so, which desserts are best?
In this article, youll find some ideas of what to keep in mind when you look at dessert options, along with resources on where to find recipes. Doing your research and learning from others is a great way to have your cake and eat it too.
The Worst Foods For Those With Ulcerative Colitis
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
What Foods Should I Eat If I Have Ulcerative Colitis
Many people with ulcerative colitis can eat a normal diet, but during flare-ups your diet may need to be altered to help reduce your symptoms.
Eating during a flare up
When you are experiencing a flare-up, eating a temporary diet of low-residue or low-fibre foods may reduce the amount and frequency of the stools you pass and allow your colon to heal.
Foods to eat during a flare-up include:
- Low-fiber fruits: bananas, cantaloupe, honeydew melon. Cooked, pureed, canned or peeled fruits. Avoid skins and seeds.
- Lean protein sources: fish, lean cuts of pork, white meat such as chicken, soy, eggs, firm tofu and smooth nut butters
- Refined grains: sourdough, potato or gluten-free bread, white pasta, white rice and oatmeal
- Seedless, skinless vegetables: fully cooked, peeled vegetables such as asparagus tips, cucumbers, potatoes and squash
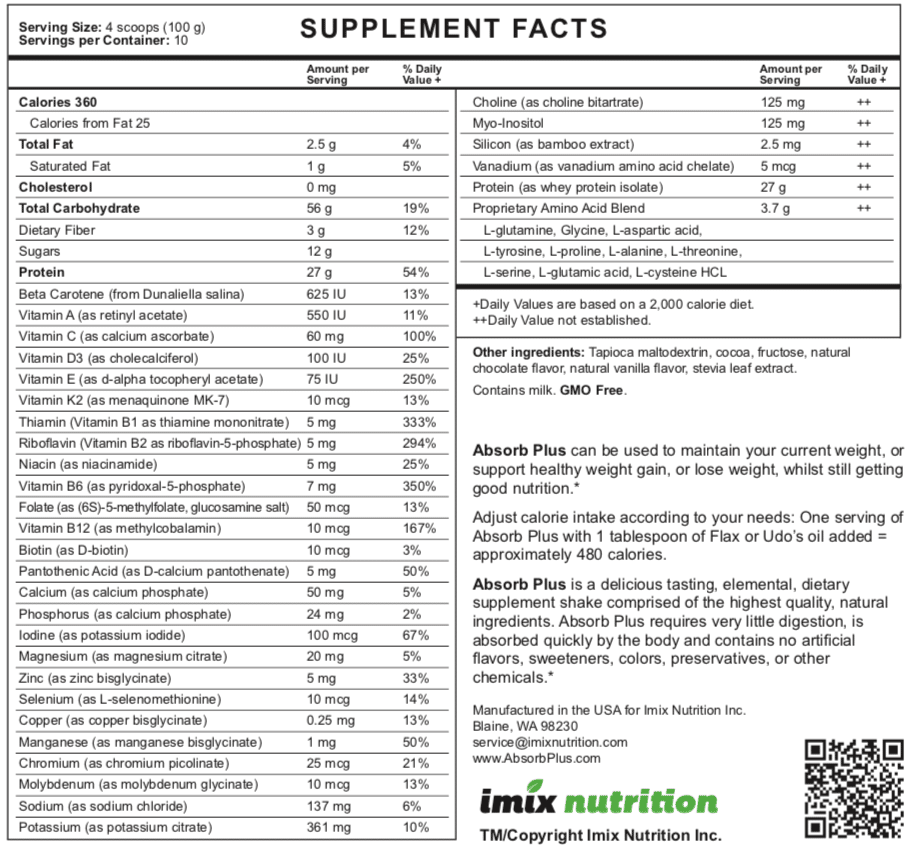
- Oral nutritional supplements or homemade protein shakes
Eating when in remission
When symptoms have lessened or subsided, many people with ulcerative colitis can resume a more normal, well-balanced diet and reintroduce foods slowly.
Slowly reintroduce:
You May Like: Foods To Avoid If You Think You Have An Ulcer
If You Love Eating Chocolate A New Research Will Delight You It Suggests That Consuming Protein Rich Foods Could Spell Relief From People Suffering From Diarrhoea And Other Disorders
In the past, studies have shown that dark chocolate helps in sleeping better, and that indulging in chocolate daily could lead to a better-working brain. Now, a new research shows that consuming protein rich foods such as nuts, eggs, seeds, beans, poultry, yogurt, cheese, and even chocolates, may foster a more tolerant and less inflammatory gut environment. This could mean relief for people living with abdominal pain and diarrhoea of inflammatory bowel disease.
These food items contain an appreciable amounts of tryptophan – an amino acid used in the buildup of proteins – which when fed on mice led to the development of immune cells that foster a tolerant gut, the study said. The findings indicated that a protein rich diet triggers the appearance of immune cells in Lactobacillus reuteri – a bacterium that normally lives in the gut, and together these promote a more tolerant, less inflammatory gut immune system.
We established a link between one bacterial species – Lactobacillus reuteri – that is a normal part of the gut microbiome, and development of a population of cells that promote tolerance, said Marco Colonna, the Robert Rock Belliveau, Professor at the Washington University School of Medicine in St Louis. The more tryptophan the mice had in their diet, the more of these immune cells they had, Belliveau added. For the study, published in the journal Science, the team examined mice that had lived under sterile conditions since birth and was germ-free.
What Causes Ulcerative Colitis

The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitis can run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high-fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
Don’t Miss: Pressure Ulcer Cream Over The Counter
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
Read Also: Bowel Ulcers Signs And Symptoms
Studies Of Cell Culture
Cell culture studies constitute a useful tool to elucidate the molecular mechanisms of action of flavanols including those related to inflammatory processes. It should be mentioned that both free flavanols and their metabolites circulate in blood, and some flavanol metabolites have shown to have a remarkable biological activity , indicating that their synergic effect to that of pure compounds should not be ruled out. Moreover, intracellular and bound phenolic metabolite concentrations can be higher than plasma levels, and can be significantly bioactive even when plasma concentrations are in the nM range . These crucial points should be considered when discussing flavanol doses used in cell culture studies and the potential value of their extrapolation to a whole-organism situation.
How Artificial Sweeteners Can Impact Gut Health
Current research suggests that artificial sweeteners can change your gut microbe composition because certain microbes can break down artificial sweeteners better than others, says Jessie Wong, RDN, LD, a registered dietitian who specializes in gut health and IBS. This allows the microbes that can break them down to flourish while the ones that cant diminish, leading to a change in composition.
For example, an October 2017 article in Moleculepoints out how neotamea no-calorie artificial sweeteneraltered the diversity of bacteria in the gut microbiome in mice by promoting the growth of certain bacteria and declining the growth of others.
Although larger studies are needed to see the long-term effects of artificial sweeteners, like neotame, on the human gut, the fact that they can cause gut dysbiosisan imbalance between the good and bad bacteria in your gutmeans theres potential for them to impact a wide range of things in your body.
Recommended Reading: Compression Therapy For Venous Leg Ulcers
Don’t Miss: How To Get Rid Of Corneal Ulcer
Certain Foods Can Trigger Uc Symptoms In Some People
Has ulcerative colitis made you hesitant to eat for fear of causing painful symptoms? If you know for sure what foods make you feel worse, it’ll be easier to live with the disease. A review published in April 2019 in the journal Current Treatment Options in Gastroenterology noted that people with inflammatory bowel disease who had a diet full of fiber from fruits and vegetables, and low in animal fats, dairy, and processed food, had the fewest flares and best health outcomes. Doctors and nutritionists recommend that people who are diagnosed with ulcerative colitis change their dietary intake to ensure that they are consuming much-needed nutrients without exacerbating symptoms.
Whats the best way to identify what not to eat if you have UC? According to the research review mentioned above, starting an elimination diet for patients with Crohns disease or UC allowed 73 percent of patients to achieve remission in a six-week period. . Elimination diets, where patients remove certain foods from their diet to see if their symptoms abate, are a good way to identify common food triggers.
To get started on one, record all the food you eat during the day in a diary or journal along with any symptoms you experience. You can do this with pen and paper or with phone apps.
What Foods Should I Avoid If I Have Ulcerative Colitis
While no single diet has been proven to treat the intestinal inflammation that causes ulcerative colitis, avoiding some foods may help alleviate symptoms during a flare-up. Trigger foods are not the same for everyone, so it is important to track what you eat and identify your own troublesome foods.
Avoid these foods during an ulcerative colitis flare-up, as they can be potential trigger foods:
- Foods high in insoluble fiber: whole grain foods , fruits with skin and seeds, some raw green vegetables, broccoli, cabbage, brussel sprouts, nuts, seeds, beans, lentils and peas
- Dairy products: milk, cream cheese and soft cheeses
- Non-absorbable sugars: sugar alcohols such as sorbitol and mannitol, which are found in sugar-free foods like gum, candy and ice cream
- High-sugar foods: pastries, candy, chocolate and juices
- High-fat foods: butter, margarine and cream, as well as greasy foods such as pizza and fried foods
- Alcoholic and caffeinated beverages: beer, wine, liquor, soda and coffee. Elimination of alcohol may not be required, but it should be consumed in moderation.
Also Check: What’s The Signs Of An Ulcer
Peanut Butter And Chocolate Chip Muffins
Anyone who is a Reeses Peanut Butter Cup fan will rejoice with this recipeproof that you can have your cake and eat it, too. I like this recipe of peanut butter muffins with dark chocolate chips for UC symptoms, because it includes oat flour, which is a great fiber-rich whole grain that provides gut health benefits by feeding probiotic microbes, and it has lactose-free milk and adds a dose of magnesium to boot, says Scarlata. Semi-sweet chocolate chips dont add much of a nutritional anything, but we wont tell!
Metabolic And Inflammatory Effects Of As Depend On The Diet
The extent to which specific bacteria are selectively modified by AS reflects diet composition, for instance, the presence of dietary saturated fat . In Wistar rats fed either with a high-fat diet or a standard rodent diet supplemented with sucralose, steviol glycoside, or a caloric sweetener , gut microbiota were differentially modified by both the type of sweetener and the fat content of the diet, explaining up to 48.5% of microbiota variation . While steviol glycoside resulted in the lowest number of LPS synthesis genes and produced the highest serum IL-10 compared with other AS, mice fed either with steviol + HFD, sucrose + HFD, or sucralose + HFD had the highest number of LPS synthesis genes. Thus, the effect of an AS depends on the diet composition, and this modulates the effects of AS on inflammation .
The same concept applies to food intake , for which studies have reported AS-induced alterations, either increasing or decreasing caloric intake . This is important, since the effects on colonic microbiota, as reported by studies, may be attributed to changes in food intake, rather than the actual AS tested. Overall, an AS-supplemented diet may modify bacterial functionality with subsequent by-products that directly or indirectly trigger/modify inflammation locally in the gut or systemically in other organs, for example, the liver.
Also Check: How Do I Get Rid Of A Stomach Ulcer
Lets Learn The Preparation Method
Recommended Reading: Snack Ideas For Ulcerative Colitis
The Benefits Of Moderate Consumption For Colitis
The flavonoids contained in cocoa, in fact, are able to stimulate the production and release of nitric oxide, which leads to an increase in cerebral blood flow and blood perfusion of the central and peripheral nervous system, such as to provide oxygen and glucose to neurons, also eliminating toxic metabolites in the brain and sensory organs and stimulating angiogenesis in the hippocampus. A modest consumption of chocolate also helps to regulate the intestine and gives benefits to the cardiovascular system. Polyphenols in chocolate, in fact, exert an anti-inflammatory action on the colon, improving the integrity of the mucosa and suggesting an inhibitory effect on the release of pro-inflammatory cytokines, with reduction of infiltration of neutrophils, and generation of nitric oxide, associated with improving colitis.
Recommended Reading: Pressure Ulcer Interventions And Rationales
Cocoa Flavonoids As Anti
Considerable attention has recently been focused on the identification of dietary compounds with anti-inflammatory bioactivity as an alternative natural source for prevention of inflammation-associated diseases . During the last decade, a growing number of studies have demonstrated that flavanols, a sub-family of the flavonoid family of polyphenols, show the capacity to modulate inflammation, as well as other major metabolic and immunological pathways . The molecular mechanisms underlying their chemo-preventive effects have been associated with their antioxidant capacity, as well as the modulation of signalling cascades and expression of genes involved in the regulation of cell proliferation and apoptosis and the suppression of chronic inflammation . Indeed, the capacity of flavanols to modulate signalling pathways involved in cellular processes such as inflammation, metabolism, proliferation and apoptosis has encouraged research on this type of polyphenols as useful bioactive compounds for nutritional prevention of cardiovascular disease and cancer.
Nitric Oxide Is A Vasodilator And An Anti
The release of nitric oxide observed after the consumption of dark chocolate with good flavonoid content, also results in a vasodilating and anti-inflammatory action, with reduction of atherogenesis. Finally, the increase in this oxide may explain the antihypertensive effects of cocoa, but also the better lipid profile, as it reduces LDL cholesterol and increases HDL cholesterol .
Also Check: How To Know If You Have A Bleeding Ulcer
Ulcerative Colitis: Lets Talk
Colitis, Ulcerative Colitis, and Crohns are often used interchangeably but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Pick A Less Acidic Alternative To Tomatoes
Whether theyre juiced, cooked, or stewed, tomatoes can be notoriously hard on your gut. Not only are tomatoes acidic, which can irritate your intestinal lining, but their seeds can also be hard to digest.
If youre not in the middle of a flare, you may be able to indulge in an occasional helping of tomato sauce perhaps a quarter cup, suggests Craggs-Dino.
Do tomatoes trigger your UC symptoms? Make a sauce or bisque-style soup from pureed cooked squash instead.
Read Also: What Is Acute Ulcerative Colitis
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Metabolism And Bacterial Utilization Of Artificial Sweeteners

The proposed advantage of most non-nutritive AS is that following ingestion they are not metabolized . Some AS are known to be compound molecules that are amenable for degradation by bacteria. Some sweeteners, i.e., sucralose, were originally thought not to be metabolizable. However, mass spectrometry studies showed that the spectral profile of the molecule recovered from feces is structurally different from that which was ingested, indicating that such AS can be metabolized in the gut, possibly by bacteria. In other cases, AS, such as stevia, are broken down into simpler molecules that can be metabolized by the host or bacteria . In such scenario, the AS core molecule, steviol, is absorbed systemically, and then excreted in urine . While AS are known to modulate the gut microbiota, little is known regarding their effect on viruses and fungi in the gut. The section below and provide an overview of absorption-excretion patterns for representative AS and the influence of gut bacteria.
Comparison of main routes of absorption, digestion, metabolism, and excretion of representative AS illustrate the absorption, digestion, metabolism, and excretion for saccharin, acesulfame-potassium, sucralose, and aspartame and steviol glycoside.
Also Check: How Do They Test For Ulcers