Ulcers Caused By Problems With Blood Circulation
The blood supply coming to the skin is needed for the skin to heal after it has become broken or split for any reason. If there is a problem with circulation, the break in the skin does not heal, and may persist, leaving an ulcer. This may be a problem with the veins, the arteries, or the smaller blood vessels. The kinds of ulcers caused by circulation problems are:
- Venous ulcers. These ulcers and their treatment are described in the separate leaflet called Venous Leg Ulcers. They occur when the circulation in your legs is not working very well. Fluid tends to pool in the legs because the veins dont work well enough to pump the blood efficiently back to the heart . This type of ulcer is more common in people with varicose veins that have lead to associated skin problems such as varicose eczema. They are also more common if you are overweight or obese, or not very mobile for any reason. They can also occur when the circulation is damaged by a deep vein thrombosis .
- Arterial ulcers. These are caused by conditions affecting arteries see the separate leaflet called Peripheral Arterial disease.
- Vasculitic ulcers. These are caused by a number of conditions which cause blood vessels to become inflamed. This is called vasculitis.
What Types Of Surgeries Can Help With Diabetic Ulcers
As podiatrists, we consider future foot function along with wound healing. If surgery is right for you, we will recommend a procedure that treats your pain or infection now so you can move more easily and with less pain.
Procedures we might discuss include:
- Debridement to remove dead or infected skin and tissue from the wound, which encourages healing.
- Skin grafts to reconstruct weakened or missing skin, which promotes healing and helps reduce the risk of infection. Skin can be taken from another part of the patients body, such as the thigh, or come from a donor it depends on each individual.
- Vascular surgery, which helps restore proper blood flow to the wound site, promoting healing and healthier skin.
- Shaving or removing bone to correct deformities that put pressure on the surrounding area, such as hammertoes, bone spurs, or bunions.
- Reconstruction of deformities such as flat or high-arched feet, which can cause areas of high pressure.
- Realigning or fusing joints to address biomechanical defects that increase pressure
- Lengthening tendons to release tension and take pressure off an ulcer, allowing it to heal, or prevent a new one from forming.
- Amputation of a toe or the foot if tissue is severely damaged or an infection will not stop spreading. Our limb salvage team exhausts all other options before recommending amputation.
Related reading:3D bunion surgery gets you back on your feet faster
Assess Wound With A Full Exam
The best treatments begin with a comprehensive exam with a full evaluation.
Generally, this will begin with a process called debridement, which involves removing all dead skin from the feet. Many foot ulcers hide under callused skin, so only debridement can expose the real wounds and help your doctor evaluate the extent of your injuries.
If your circulation is especially poor, your doctor may wait to perform debridement until a vascular physician is able to identify the source of poor circulation, such as a major clogging of the blood vessels, and perform the treatment or surgery necessary to boost circulation again.
Whether debridement occurs first or second in this process, it creates clean edges around the diabetic foot ulcer and encourages healthy tissue to grow.
Recommended Reading: Can A Person Die From Ulcerative Colitis
What Can Caregivers And Loved Ones Do To Contribute To Prevention
Education and instruction on the proper process for general foot care should be available to the patient and family, especially anyone who carries the most responsibility for daily care. General foot care steps include:
- Daily foot washing
- Drying the feet thoroughly
- Proper moisturization
If the patients feet are not sweating or visibly dirty, a little means a lot when it comes to soap. Older patients already have reduced natural body oil, so it is necessary to preserve the moisture that is there. Moisturizing soaps are recommended. If bedside bathing is necessary, a few drops of baby oil can be added to the water for extra moisturization followed by moisturizing lotion after the body has been patted dry. Getting dressed for the day after moisturizing is important, as the clothing will easily slide over the lotioned limbs.
Do not apply moisturizer between the toes of the foot, as this can promote fungal growth. If excessive feet sweat is an issue, roll-on antiperspirant can be applied to the soles of the feet before putting on socks.
Socks and shoes should always be worn whether the patient is in a wheelchair or not. Footwear is not for walking, but for protection, in diabetics. Shoes are barriers between toes and items a patient may kick accidentally and a support structure. Footrests should be kept on wheelchairs. When the patient is pushed, they may be dragging their feet and not even realize it, and an injury can be sustained.
Diabetic Foot Ulcer Symptoms
Normally a wound or sore on the skin would cause pain. But the same loss of feeling in the feet that often contributes to the development of a diabetic foot ulcer means that theres often no pain associated with the ulcer. This can make it difficult for people to realize that an ulcer is even there in the early stages, when treatment is most effective.
Aside from pain, another sign to look for is discharge or drainage from the wound in the socks. Ulcers that have been present for some time and that have become infected may also cause an unpleasant odor.
Recommended Reading: What To Eat When You Have Ulcers And Acid Reflux
Who Is At Risk For A Decubitus Ulcer
Individuals with limited mobility and who remain for long periods of time sitting or lying in the same position are vulnerable to developing pressure ulcers. Older individuals with more fragile skin are also at risk. Other risk factors include:
- Poor diet with insufficient nutrients for skin health.
- Not drinking enough water to hydrate skin.
- Medical conditions such as diabetes which causes poor blood circulation to skin tissue.
Preventing & Curing Diabetic Ulcers With Wellstar Wound Care
When someone is diabetic, a small wound can escalate into a major health issue and, in many cases, lead to an amputation. However, with proper wound care and accelerated healing with hyperbaric medicine, Wellstar patients are partnering with providers to treat wounds like diabetic foot ulcers.
Diabetic foot ulcers can develop if diabetes is not well-managed, and some causes of ulcers include poor circulation and high blood sugar. Ulcers may go unnoticed at first because many people with diabetes are also affected by neuropathy and do not have feeling in their feet, said Dr. Ricardo Duran, Medical Director of the Wound Care and Hyperbaric Medicine Department at Wellstar North Fulton Hospital.
Also, if a diabetic person gets a wound, it may not heal as quickly, as people with diabetes are more likely to also experience poor circulation, immune system deficiencies and elevated blood sugar levels.
When you combine the lack of sensation in the foot with the lack of healing, that leads to even more damage, Dr. Duran said.
Foot ulcers should be taken seriously when a diabetic person has an open wound, their five-year mortality rate increases by about 32%, according to Dr. Duran.
Recommended Reading: Low Dose Naltrexone Ulcerative Colitis
Do Not Completely Cut Down On Iodine
Many people who suffer from diabetes give up consuming iodine with the fear of increased insulin resistance. But in actuality, some amount of iodine is essential for your body. Iodine is even helpful in enhancing the healing process of diabetic foot ulcers. Thus, there is no harm in including some iodine in your diet to treat the problem of diabetic foot
Recommended Reading: Ulcerative Colitis Weakness And Fatigue
Why Wont My Foot Ulcer Heal
With adequate blood circulation, superficial foot ulcers normally heal within 12 weeks. Due to a lack of preventive and remedial actions, a third of all cured foot ulcers pose a risk of recurrence. Deep ulcers with a serious infection and poor circulation may need surgery and a prolonged period of recovery.
Also Check: Good Snacks For Ulcerative Colitis
How To Heal Leg Ulcers Naturally
What You Have To Do
How Often You Should Do This
Do this 2-3 times daily.
Why This Works
Aloe vera is a therapeutic herb that is widely used to treat various ailments. It is extremely effective in healing leg ulcers as it not only inhibits the growth of bacteria but also prevents further infection . It contains compounds like anthraquinones and certain hormones that are said to render wound healing properties to it .
Also Check: What Can You Eat With A Stomach Ulcer
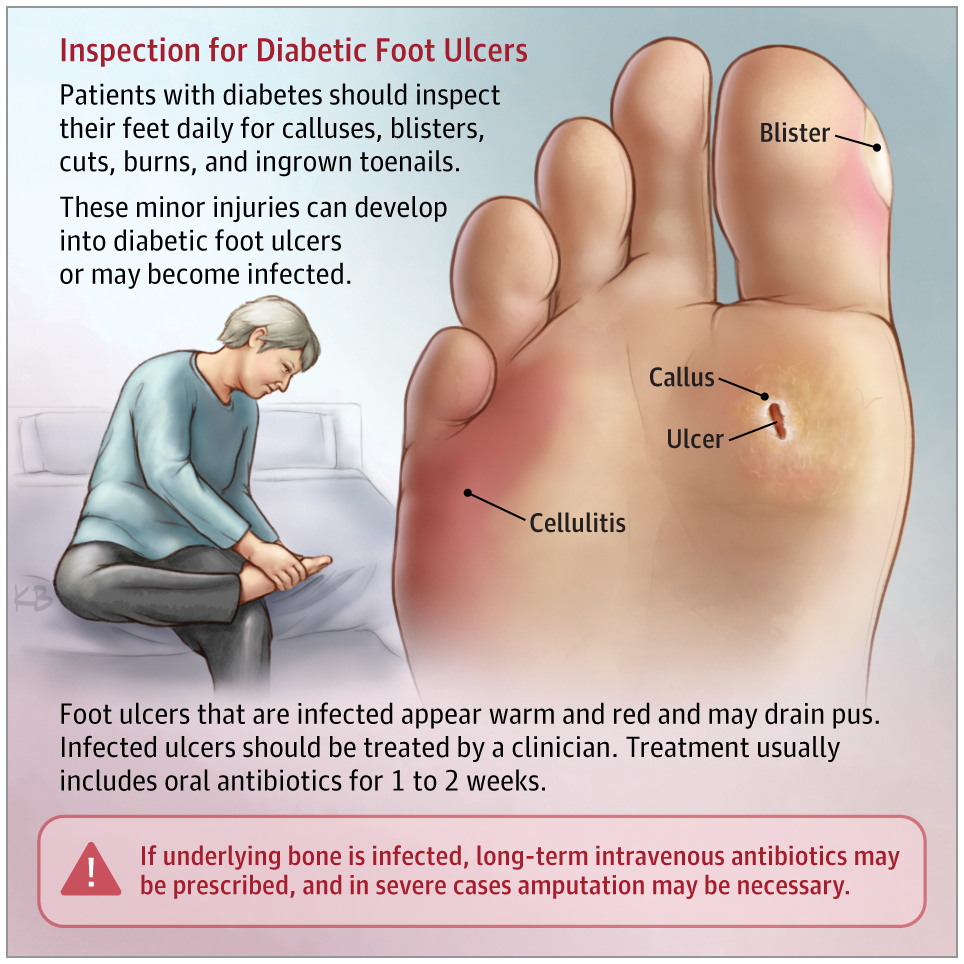
What Does A Foot Ulcer Caused By Diabetes Look Like
If the stage of the ulcer has progressed, it should be evident. A foot ulcer resembles a red, round crater in the skin that is surrounded by thicker, calloused skin. Ulcers of severe severity might be so deep as to reveal tendons or bones. However, some symptoms may be difficult to diagnose or may indicate another issue.
You May Like: High Fiber Diet For Ulcerative Colitis
Nonsurgical Treatment For Diabetic Foot Ulcers
To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
Tips To Prevent Ulcers

Thereâs a lot you can do to lower your chance of having ulcers in the first place:
Keep your blood sugar in check. Good blood sugar control is the single best way to prevent small cuts and sores from becoming ulcers. If you have trouble managing your blood sugar, tell your doctor. They can work with you to make changes to your medication and lifestyle that will keep your blood sugar from getting too high. Even if your blood sugar level is fairly steady, itâs still important to see your doctor regularly. Thatâs especially key if you have neuropathy, because you may not feel damage to your skin and tissue.
Check your skin every day, and pay special attention to your feet. Look for blisters, cuts, cracks, sores, redness, white spots or areas, thick , discoloration, or other changes. Donât rely on pain even feeling more warmth or cold than usual can be a sign that you have an open wound on your skin, and itâs possible that you may feel nothing at all.
Ulcers are most likely to form on the ball of your foot or the bottom of your big toe, so be sure to check your feet every night. If you notice a problem, or you arenât sure if somethingâs normal, call your doctor.
Donât smoke.Smoking damages your blood vessels, decreases blood flow, and slows healing. Those things raise your risk of ulcers and amputation.
Show Sources
Don’t Miss: How Do They Treat Stomach Ulcers
Risks Of Bed Sores During The Pandemic
Not only has the COVID-19 pandemic increased the number of patients who need hospitalization, but it has also complicated care and bed sores prevention. Sedated COVID patients are usually placed on their belly instead of their neck to assist with breathing. So, in this position, nurses dont look for pressure injuries on the patients back but keep a sharp eye on their:
Moreover, rare coronavirus symptoms may be mistaken for bed sores in elderly patients. For that purpose, the National Pressure Injury Advisory Panels position paper warns health care providers to be alert to skin discoloration in COVID-19 patients. In other words, skin manifestations like COVID toespinkish-reddish pernionlike lesions that turn blue to purple in timecan resemble deep tissue injury but are actually a symptom of the virus.
Skin Grafts For Diabetic Ulcer Treatment
When a diabetic ulcer does not improve after conservative treatment, your podiatrist may use a skin graft as a sort of bandage. Skin grafts close wounds and help them heal. Traditionally, skin grafts are done in a hospital setting under general anesthesia. However, diabetic ulcers can often be treated with biosynthetic skin substitutes that are grown in a lab and applied on an outpatient basis.
When you come to the office, your doctor will first clean the ulcer and then debride the wound, which means cutting off all the dead skin with surgical tools to make sure no infection remains and the wound is clean.
The doctor will then apply the biosynthetic skin, which looks a bit like a square of tissue paper. While it might not look like much, this miraculous bit of bioengineering covers and protects your wound, bonds to your skin, and promotes healing.
Finally, the doctor will bandage the area in gauze to keep it clean. It can take several treatments before your ulcer is completely healed, and you may also wear a boot during that time to help keep pressure off the ulcer.
Recommended Reading: What Are Ulcers In Horses
Signs & Symptoms Of A Foot Ulcer
A foot ulcer can be shallow or deep. When it starts, it looks like a red crater or dimple on the skin. If it becomes infected, it can develop drainage, pus, or a bad odor.
If you have nerve damage in your feet, then you won’t notice the pain of a small stone, too tight shoes, or the formation of a foot ulcer. As you get older or have a medical condition like diabetes or Raynaud’s phenomenon, it’s best to check your feet regularly for damage and sore spots and consult your doctor.
Venous ulcers – Patients with vein ulcers may complain of swollen, tired, and achy legs. Venous ulcers are not typically very painful unless touched, or unless they are infected.
Arterial ulcers – Patients with arterial disease may complain of tingling, burning, or coldness in the feet or toes. Patients may also experience leg pain when walking, or foot pain when elevating the legs. Ulcers usually occur at the tips of toes or on the sides of the ankles or lower calves. The ulcer may look punched out with a yellow-brown or black color. They are often very painful unless there is nerve damage.
Prolonged Pressure On The Feet
As mentioned in the previous example, when shoes fit poorly, ulcers can occur. In people without nerve damage, this is usually due to severe atherosclerosis, or a deformity such as a fracture. Elderly patients often have difficulty or find it uncomfortable to examine their feet, ignoring moderate pain from pressure on the feet, which may result in the development of an ulcer.v
Recommended Reading: How To Heal A Diabetic Foot Ulcer
What Are Foot And Toe Ulcers
An ulcer is an open wound or sore that will not heal or keeps returning. When you have ulcers on your feet and toes, it can be related to diabetes specifically, a complication called neuropathy that causes you to lose feeling in your feet. A scrape, cut or puncture in your skin can turn into an ulcer, but you might not know its there if you have neuropathy.
Ulcers can lead to infections. Sometimes, the infection wont go away and you may need to have part of your foot or toe surgically removed . About 15% of people with diabetes will get a foot or toe ulcer. Around 14% to 24% of people with diabetes in the U.S. need an amputation after they get an ulcer.
Sensory And Autonomic Neuropathy
Distal symmetric polyneuropathy is perhaps the most common complication affecting the lower extremities of patients with diabetes mellitus. This complication occurs in up to 58 percent of patients with longstanding disease.19 Neuropathy, a major etiologic component of most diabetic ulcerations, is present in more than 82 percent of diabetic patients with foot wounds.4 This lack of protective sensation, combined with unaccommodated foot deformities, exposes patients to undue sudden or repetitive stress that leads to eventual ulcer formation with a risk of infection and possible amputation.20
In the diabetic foot, autonomic neuropathy has several common manifestations. First, denervation of dermal structures leads to decreased sweating. This causes dry skin and fissure formation, which predispose the skin to infection. In vascularly competent patients, this autosympathectomy may lead to increased blood flow, which has been implicated as one of the primary etiologic factors in the development of Charcot’s joint and severe foot deformity.2123
The nylon monofilament test is a simply performed office test to diagnose patients at risk for ulcer formation due to peripheral sensory neuropathy.24 The test is abnormal if the patient cannot sense the touch of the monofilament when it is pressed against the foot with just enough pressure to bend the filament25 . Physicians can obtain a monofilament kit at a small cost from the National Diabetes Information Clearing-house .
Read Also: What Is Refractory Ulcerative Colitis
Wound Care And Dressings
Care for your wound as instructed by your provider. Other instructions may include:
- Keep your blood sugar level under good control. This helps you heal faster and helps your body fight infections.
- Keep the ulcer clean and bandaged.
- Cleanse the wound daily, using a wound dressing or bandage.
- Try to reduce pressure on the healing ulcer.
- Do not walk barefoot unless your provider tells you it is OK.