Challenge : Current Treatment Strategies Of Asuc Are Based On Low Quality Evidence
Current management of ASUC is not based on high-quality evidence with only a few good quality RCTs performed and these are performed on only a limited number of patients. This lack of sound evidence might explain why the evolution of successful management in ASUC are far behind compared to general IBD management.
Using corticosteroids as a medical salvage therapy was investigated by Truelove and Witts as early as 1955. It was one of the first randomized controlled trials and established corticosteroids as the cornerstone for ulcerative colitis management.5 In this pivotal study, 210 patients with moderate to severe colitis were randomized to treatment with 100 mg of cortisone or placebo for a period of six weeks. Clinical remission rates were higher in the steroid-treated group compared to the placebo group . This was accompanied by a reduction in mortality and an improvement in endoscopic appearance. In a follow-up trial in 1974, 49 patients with severe ulcerative colitis were treated with 5 days of intravenous methylprednisolone achieving remission in 73%.20 In a meta-analysis, Turner et al combined 32 studies between 1974 and 2006 and found a pooled response rate of 67% with a colectomy rate of 27%.21 In a retrospective study in 142 ASUC patients, patients responding to IV corticosteroids were shown to have a low 5-year colectomy risk despite high relapse rates .22
Optimal Dose Targeting Is Primordial
Several lines of evidence suggest that conventional weight-based dosing of infliximab salvage therapy might be insufficient in ASUC. The severe intestinal inflammation is associated with an important intestinal loss of protein resulting in hypoalbuminaemia but also a rapid clearance of infliximab in the faeces.58 Additionally, high concentrations of mucosal metalloproteinases, associated with inflammation, lead to degradation and inactivation of anti-TNF antibodies.59,60
In a pharmacokinetic study, Brandse et al showed that patients with a faster intestinal clearance of infliximab were at risk for worse clinical outcomes and had an increased chance of infusion-related reactions compared to patients with a normal drug clearance. Drug clearance seemed to be highest in the group of patients with higher CRP levels .59 In a retrospective analysis of 50 patients hospitalized for ASUC an accelerated dosing strategy of infliximab was associated with a lower colectomy rate .61 However, in another multicentre, retrospective study including 213 patients with steroid refractory ASUC no difference was found between normal and accelerated dosing strategy, although dosing regimens including a higher induction dose of infliximab were associated with a lower rate of colectomy.62
Patients not responding to rescue therapy with infliximab or cyclosporin by day 7 or that develop serious complications earlier should be referred for colectomy.25
Studying Tofacitinib In Treatment Of Acute Severe Ulcerative Colitis
The team examined two groups of patients with ASUC who previously failed to respond to a biologic medication . The first group received standard care, which involved intravenous corticosteroids, as well as a rescue dose of infliximab or cyclosporine, as needed.
The second group received tofacitinib, in addition to corticosteroids. The tofacitinib group was stratified according to dosage to determine if an off-label and high-intensity 10 milligram dose administered three times a day was more effective than the approved dose of 10 milligrams administered two times a day.
We found that tofacitinib reduced the rate of colectomy in patients admitted with ASUC compared to the control group, said Berinstein. But the reduction in colectomies was driven entirely by the 10 milligram dose of tofacitinib administered three times a day. Notably, we saw no benefits among the patients who only received the drug twice daily, even when compared to steroid use alone.
Read Also: Foam Dressings For Pressure Ulcer Prevention
Small Study Found That Patients Appeared To Benefit From Limited
byZaina Hamza, Staff Writer, MedPage Today June 1, 2021
For biologic-experienced patients hospitalized with acute severe ulcerative colitis, off-label, high-intensity doses of tofacitinib given with intravenous corticosteroids may have reduced their chances of undergoing a colectomy, a small retrospective study found.
Within 90 days, 15% of patients receiving tofacitinib at standard or more frequent dosing and 20% of patients in the control group underwent a colectomy, with a multivariate model finding that tofacitinib reduced the risk of colectomy , reported Jeffrey A. Berinstein, MD, MSc, and colleagues from the University of Michigan in Ann Arbor.
Giving hospitalized patients 10 mg of tofacitinib three times per day for a total of nine doses was significantly protective against a colectomy , but giving 10 mg of tofacitinib to patients twice daily was not significantly protective , the authors wrote in Clinical Gastroenterology and Hepatology.
The group noted that while the study was not powered for safety, “we did not observe any increased risk of infection, venous thromboembolic events, or cardiovascular events with inpatient tofacitinib.”
Safety with the JAK inhibitor has been a particular concern of late, with the FDA issuing an alert after a post-marketing safety study in rheumatoid arthritis patients turned up a significantly higher risk of malignancy and a numerical increase in major adverse cardiovascular events versus other available treatments.
Significance Of This Study
What is already known on this subject?
-
The British Society of Gastroenterology has published evidence-based guidelines for the management of patients with acute severe UC , but it is unknown whether these are appropriate in the setting of severe acute respiratory syndrome coronavirus-2 infection.
-
Currently there are limited data to inform clinicians in this area and there is no published guidance for the management of ASUC in the setting of the COVID-19 pandemic.
What are the new findings?
-
The current BSG IBD guidelines provide a management pathway which remains largely appropriate during the COVID-19 pandemic.
-
However, some treatment options were deemed uncertain or inappropriate in patients with established COVID-19 pneumonia.
-
It is appropriate to involve COVID-19 specialists in decision-making for patients with ASUC who are SARS-CoV-2 positive.
-
Steroid tapering as per BSG guidance was deemed appropriate for all patients apart from those with COVID-19 pneumonia in whom a 46week taper was preferred.
-
Prophylactic anticoagulation postdischarge is appropriate in patients with a positive SARS-CoV-2 swab.
Don’t Miss: List Of Foods Good For Ulcers
Early Recognition Close Monitoring And Timely Re
Any patient meeting the criteria for severe disease should be recognized promptly and admitted in the hospital. Stool cultures for enteric pathogens and Clostridium difficile should be taken at the earliest possibility but results should not be awaited before rapid IV corticosteroid therapy. Flexible unprepared sigmoidoscopy with minimal air insufflation should be performed within 24 hours of admission to confirm diagnosis and exclude a superimposed infection with the cytomegalovirus .3,8
Following initiation of corticosteroid therapy patients should be closely monitored with daily blood works, clinical examination and serial abdominal films as clinically indicated. Positive stool cultures should prompt treatment with antibiotics, presence of a significant amount CMV inclusions on colonic biopsy are an indication for ganciclovir treatment. Formal re-assessment is performed between days 3 and 5.3,8 As discussed above, current evidence does not allow for a singular recommendation. Failure of corticosteroid therapy is therefore based on a clinical, biochemical and radiological assessment. Several indices such as stool frequency, CRP and albumin levels and colonic dilatation on plain radiography can be used as described above.
Comparing Infliximab And Cyclosporine
Two head-to-head studies have compared efficacy of infliximab and cyclosporine for ASUC showing equivalence among the two medications. In the open-label CYSIF trial, there was no statistically significant difference between infliximab and cyclosporine in treatment failure, adverse events, mucosal healing rates, colectomy rates and colectomy-free survival at 1 and 5 years . The CONSTRUCT trial was an open-label pragmatic randomised trial of infliximab and cyclosporine and again showed no significant difference in clinical effectiveness . Moreover, a systematic review and meta-analysis of infliximab and cyclosporine randomised controlled trials showed no difference in response rates up to 1 year of therapy . Cyclosporine and infliximab are equally effective in ASUC, but infliximab is simpler in use although more expensive . The choice between rescue therapies should be individualised and several other factors, such as co-morbidities, contra-indications, previous exposure to medications, expertise and feasibility of laboratory testing, should be taken into consideration on decision .
Also Check: Stage 2 Pressure Ulcer Treatment Dressing
Integrating Novel Therapies Into The Management Of Moderate
- AffiliationsDivision of Gastroenterology and Hepatology, University of Calgary, Calgary, AB T2N 4Z6, CanadaDepartment of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB T2N 4Z6, CanadaAlimentiv, London, ON, Canada
- Division of Rheumatology, University of Calgary, Calgary, AB T2N 4Z6, CanadaMcCaig Institute for Bone and Joint Health, University of Calgary, Calgary, AB T2N 4Z6, Canada
Optimal Asuc Care Is Multidisciplinary In Nature
ASUC management requires early liaison with other medical specialities from the start of the admission with the multidisciplinary team consisting of a gastroenterologist specialised in IBD, an abdominal surgeon, a radiologist, the IBD nurse and a nutritionist.
Discussing the timing and advantages of surgery early on with the patient is important and requires not only the colorectal surgeon but an early intervention of the stoma nurse. Despite offering the prospect of a restored bowel function, IPAA in itself has a significant impact on functionality and quality of life. Frequently occurring complications such as leakage, sexual dysfunction, soiling and the occurrence of inflammatory disorders of the pouch in up to 50% of IPAA patients should be discussed upfront. Importantly, ileal pouch-anal anastomosis has profound effects on female fertility in a population often within the child-bearing age, although laparoscopic approaches tend to have less severe effects, presumably due to less intra-abdominal adhesions.54,55
Recommended Reading: Is Constipation A Symptom Of Ulcerative Colitis
Tofacitinib For Severe Ulcerative Colitis: Will It Prevent Colectomies
Gastrointestinal experts explore the benefits of the drug when treating patients with acute severe ulcerative colitis.
Acute severe ulcerative colitis, or ASUC, can be extremely debilitating. Symptoms for the condition range from frequent bloody bowel movements to anemia, weight loss, and even fevers and chills. And nearly 30% of individuals who develop an episode of ASUC require a colectomy, which is a surgery that involves removing parts, or all, of your colon.
When someone with ASUC has a colectomy, its irreversible and certainly can have a huge impact on the quality of their life, said Jeffrey Berinstein, M.D., a gastroenterologist and clinical lecturer at Michigan Medicine. Janus kinase inhibitors, which are better known as JAK inhibitors, are drugs that work to inhibit the activity of certain enzymes. The JAK inhibitor, tofacitinib, has shown itself to be an effective drug when treating ASUC. But I teamed up with several of my colleagues, including Peter Higgins, M.D., Ph.D., to truly examine if its use could prevent individuals from having this life-altering surgery.
The teams research on tofacitinib was recently published in Clinical Gastroenterology and Hepatology.
According to Berinstein, ASUC is considered a medical emergency and requires treatment quite quickly.
Like Podcasts? Add the Michigan Medicine News Break on iTunes or anywhere you listen to podcasts.
Sequential Therapy In Asuc
Sequential therapy is defined as the use of a calcineurin inhibitor as rescue therapy in patients not responding to infliximab and vice versa. Sequential therapy is not recommended by current guidelines as it has been associated with serious side effects and infections because of cumulative immunosuppression . According to ECCO guidelines, only one attempt at rescue therapy should be considered before referral for colectomy and third-line medical therapy should only be considered in specialist referral centres and highly selected cases .
Also Check: How To Test For Ulcerative Colitis
Predictors Of Outcomes In Asuc Response To Corticosteroid Therapy And Indicators For Rescue Therapy
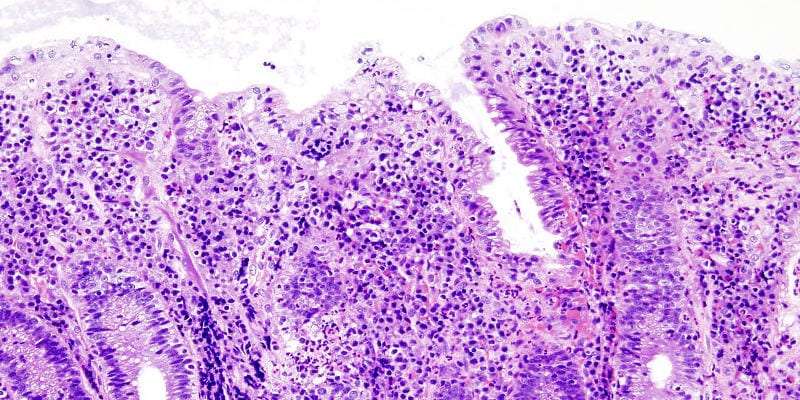
Several markers have been studied as predictors of outcome in ASUC. These can be divided into clinical, biochemical, endoscopic and radiological and several indices and scoring systems have been developed, that can potentially predict disease outcomes and therefore guide patient management. Low albumin levels have been associated with an increased risk for colectomy and a CRP/albumin ratio of 0.85 on day 3 of intravenous steroid therapy was found to predict the need for colectomy with a sensitivity of 70% and specificity of 76% in one study . Endoscopic markers can also be used as predictors and severe endoscopic lesions including deep ulcers, extensive loss of mucosal layers, well-like ulcers or large erosions have been associated with non-response to corticosteroids and need for colectomy . As previously mentioned, a UCEIS of7 on admission is a predictor of the need of rescue therapy or colectomy . The use of faecal calprotectin as a predictor of failure of corticosteroid therapy has also been investigated. A prospective cohort study by Jain et al. found that all patients with UCEIS> 6 on admission and faecal calprotectin> 1000 g/g on day 3 failed steroid therapy .
Implications For Patient Care

J Crohns Colitis.
- Steinhart A.H.
- et al.
Clin Gastroenterol Hepatol.
- Branche J.
- et al.
Lancet.N Engl J Med.Gastroenterology.
- Redmond C.E.
- et al.
Clin Gastroenterol Hepatol.
- Waljee A.K.
- et al.
Dig Dis Sci.
N Engl J Med.J Crohns Colitis.J Crohns Colitis.Clin Gastroenterol Hepatol.Clin Gastroenterol Hepatol.Drug Metab Dispos.
- Wildenberg M.E.
- et al.
Gastroenterology.
- Truong S.
- et al.
Clin Gastroenterol Hepatol.
Don’t Miss: Does Ulcer Pain Come And Go
Editorial: Is Tofacitinib Another Rescue Option For Acute Severe Ulcerative Colitis
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
IBD Centre, Guys and St Thomas NHS Foundation Trust, London, UK
School of Immunology and Microbial Sciences, King’s College, London, UK
Solutions Towards A Better Asuc Management In The Future
Despite the fact that numerous challenges remain to be solved in ASUC management, current evidence does already provide several solutions to improve our current care of patients with ASUC. How we can integrate these in clinical practise is represented in Figure 1 and Box 1.25
|
Figure 1 Treatment algorithm for acute severe ulcerative colitis. Adapted with permission from Hindryckx P, Jairath V, DHaens G. Acute severe ulcerative colitis:from pathophysiology to clinical management. Nat Rev GastroenterolHepatol. 2016 13:654664. Copyright © 2016, Nature Publishing Group, a division of Macmillan Publishers Limited. All Rights Reserved.3 |
|
Box 1 Tips to Improve Your Care of ASUC Patients |
Read Also: How To Treat A Diabetic Ulcer
Challenge : Identifying Patients At Risk Remains A Problem In Clinical Practise
Early diagnosis of ASUC is historically based on the Truelove and Witts criteria consisting of the presence of bloody stools 6 times a day and at least one of the following signs of systemic toxicity: pulse rate > 90 bpm, temperature > 37.8, haemoglobin < 10.5 g/dl or erythrocyte sedimentation rate > 30 mm/h. Despite being 60 years old, they still remain the most sensitive criteria to define ASUC, although they must always be applied and considered in view of the circumstances and setting.7 Other indices like the clinical partial Mayo clinic score and the Montreal classification are less frequently used in clinical practise, however comparative studies for diagnosis of ASUC are not available.3,8
|
Table 1 Truelove and Witts Criteria for Acute Severe Ulcerative Colitis |
Predicting which patients are likely to fail initial treatment with corticosteroids is essential in the management of ASUC. This allows for early and multidisciplinary planning of medical and/or surgical rescue therapy.3,8 Several predictive indices have been developed but are infrequently used in clinical practise.
|
Table 2 Predictive Indices for Corticosteroid Failure in Acute Severe Ulcerative Colitis |
Lastly, plain abdominal radiography can also provide prognostic information. The presence of visible mucosal islands or a colonic diameter of > 5.5 cm predicts corticosteroid failure in 75% of patients.10 Additionally, small bowel distention conveys an increased risk for colectomy during the same admission.19
Accelerated/intensified Infliximab Dosing For Asuc
Two studies have demonstrated that higher infliximab serum concentrations are associated with greater efficacy and better outcomes . Moreover, the are several other factors that would support the need for dose optimisation of infliximab in the acute phase. These include the high TNF burden in ASUC, the proteolytic degradation of anti-TNF associated with increased drug clearance and faecal losses from increased gut permeability associated with severe inflammation . According to BSG guidelines, patients who have not responded sufficiently 35 days after the first infliximab infusion should be treated with an accelerated induction regimen after a colorectal surgical review to exclude the need for emergency colectomy . Some clinicians also use an initial 10 mg/kg dose as salvage therapy, however, optimal timing and dose are yet to be defined and further studies are needed for dose intensification to be implemented into clinical practice.
Recommended Reading: Treating Leg Ulcers With Sugar
Other Jak Inhibitors In Ulcerative Colitis
A more selective JAK inhibitor could ideally improve the safety profile and clinical efficacy. Taking advantage from the experience of multiple JAK inhibitors available for other immune-related disease, several new compounds are being tested in UC and CD. Peficitinib is an oral JAK inhibitor, which showed a moderate selectivity for JAK3 over JAK1, JAK2, and TYK2 in in vitro studies. Efficacy and safety of peficitinib in UC patients were investigated in a Phase 2b dose-ranging trial. Two hundred and nineteen patients with moderate-to-severe UC were randomized to 25 mg once daily , 75 mg OD, 150 mg OD, 75 mg twice daily or placebo, and the primary outcome was peficitinib dose-response after 8 weeks. Secondary endpoints included clinical response, clinical remission and mucosal healing. Although a statistically significant peficitinib dose-response was not demonstrated, a higher rate of patients receiving peficitinib 75 mg OD achieved clinical response, remission and mucosal healing. Moreover, such an improvement was accompanied by IBDQ improvement and inflammatory biomarker normalization. The AE rate was higher in the peficitinib group compared to placebo.