What Types Of Surgeries Can Help With Diabetic Ulcers
As podiatrists, we consider future foot function along with wound healing. If surgery is right for you, we will recommend a procedure that treats your pain or infection now so you can move more easily and with less pain.
Procedures we might discuss include:
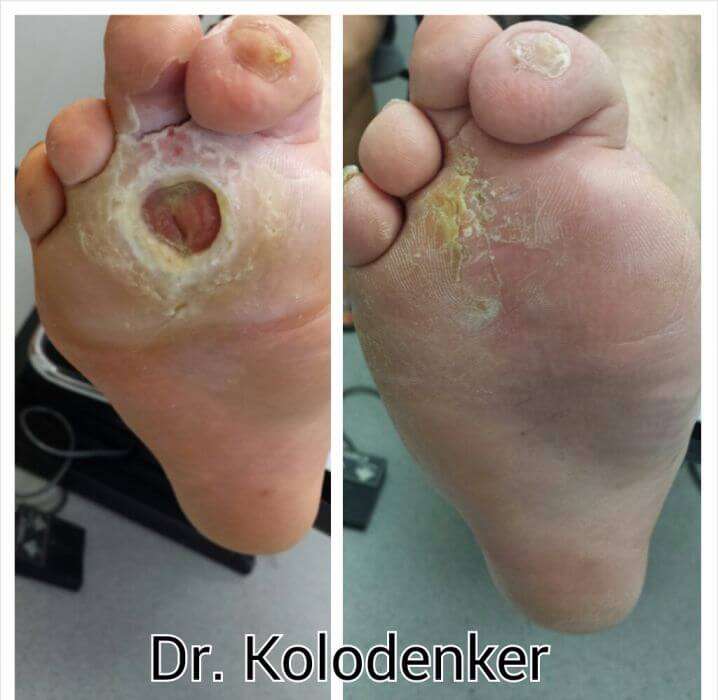
- Debridement to remove dead or infected skin and tissue from the wound, which encourages healing.
- Skin grafts to reconstruct weakened or missing skin, which promotes healing and helps reduce the risk of infection. Skin can be taken from another part of the patients body, such as the thigh, or come from a donor it depends on each individual.
- Vascular surgery, which helps restore proper blood flow to the wound site, promoting healing and healthier skin.
- Shaving or removing bone to correct deformities that put pressure on the surrounding area, such as hammertoes, bone spurs, or bunions.
- Reconstruction of deformities such as flat or high-arched feet, which can cause areas of high pressure.
- Realigning or fusing joints to address biomechanical defects that increase pressure
- Lengthening tendons to release tension and take pressure off an ulcer, allowing it to heal, or prevent a new one from forming.
- Amputation of a toe or the foot if tissue is severely damaged or an infection will not stop spreading. Our limb salvage team exhausts all other options before recommending amputation.
Related reading:3D bunion surgery gets you back on your feet faster
Diabetic Foot Ulcer Prevention
Prevention of DFUs often goes hand in hand with intervention. The ultimate goal is to allow the ulcer to heal properly and avoid future complications such as amputation.
Glycemic control. Individuals with diabetes must monitor their blood glucose closely to prevent hypoglycemic or hyperglycemic episodes. These events can have long-term consequences, including a DFU.
The human body requires balanced blood glucose to heal appropriately. Recent literature suggests that a hemoglobin A1c value between 7.0% and 8.0% is optimal for facilitation of ulcer healing.4 However, this is dependent on the individuals glycemic control at baseline. Additionally, an individual who has a DFU, an HbA1C of over 8.0%, and a fasting blood glucose greater than 126 mg/dL is more likely to have a lower extremity amputation.5
Other studies also indicate that strict glycemic control after a DFU has formed can lead to better healing rates. This was true for DFUs that did not respond to conventional care.6 Better glycemic control leads to improved healing and prevention.
Proper footwear. As discussed earlier, individuals with diabetes may not be able to feel the touch or pain of a sharp object or pressure point on their foot. Therefore, proper footwear is essential to preventing ulceration initially. Proper footwear includes:
- Sufficient coverage of the foot
- Appropriate sizing of footwear
- Walker
- Orthotic
- Total contact casting
Who Gets Diabetic Foot Ulcer
Diabetic foot ulcer has an annual incidence of 26% and affects up to 34% of diabetic patients during their lifetime. Risk factors for developing a diabetic foot ulcer include:
- Type 2 diabetes being more common than type 1
- A duration of diabetes of at least 10 years
- Poor diabetic control and high haemoglobin A1c
- Being male
- A past history of diabetic foot ulcer.
You May Like: Foods You Can Eat With An Ulcer
Diabetic Foot Ulcer: Treatment And Prevention
Estimates are that by 2030 there will be 550 million individuals with diabetes in the world. Because almost a quarter of all people with diabetes will develop a foot ulcer at some point, health care workers need to know the best practices for diabetic foot ulcer prevention and treatment.
Determining which diabetic foot ulcer type is important to determine an effective treatment. Here are the different types of these wounds:
- Neuropathic ulcers arise when the nerve damage from diabetic neuropathy causes the individual with diabetes to not feel pain from an injury, which often leads to the ulcer progressing substantially before the person is even aware of it. Foot and toe deformities, corns, calluses and areas repetitive stress are likely places of injury. Footwear can not only hide these issues, but can exacerbate the injury if the shoe is ill-fitting.
- Ischemic ulcers or arterial ulcers as they are sometimes called may occur due to lack of blood flow to the extremity. When an ulcer occurs as the result of an injury to the extremity, the lack of blood flow makes these ulcers difficult to heal.
- Neuroischemic ulcers occur in individuals with both neuropathy and poor arterial blood flow and are the most difficult to heal.
- Infected wounds occur in about half of patients with a diabetic foot ulcer and require particularly close care.
Vitamin E For Immunity And Recovery

Vitamin E is essential for the optimal functioning of the body. In the case of foot ulcers too, vitamin E produces amazing results. Vitamin E speeds up the healing process. It also improves the circulation of blood in the body. A proper supply of blood and oxygen to the wounded region prevents the wound from getting infected.
Also Check: How To Fix A Stomach Ulcer
Diabetic Wound Care: 6 Ways To Treat Diabetic Foot Ulcers
Neuropathic ulcers, often caused by diabetes, are slow to healeven more so as patients age, if they have longer-term diabetes, or if theyre smokers. Other factors that may stall healing include hypertension, hypercholesterolemia, and abnormal blood sugar levels, often associated with diabetes.
Diabetic ulcers typically occur below the ankle at any site of pressure, friction, shear, or trauma. The wound is likely to be round, with margins often characterized by a periwound callus. The presence of diabetes increases the risk for infection.
Treating neuropathic/diabetic ulcers can be challenging, so be sure to take the following steps to simplify the process and help improve outcomes:
Zinc To Speed Up The Healing
Zinc-rich foods like eggs, nuts, and legumes can prove to be very beneficial for both your diabetes and diabetic foot ulcers. Zinc promotes the production and secretion of insulin in the body and thus helps to keep blood sugar levels in check. Zinc also hastens the healing of the wound by maintaining the structural integrity of the dermal tissue.
Also Check: Surgical Management Of Ulcerative Colitis Ppt
Taking Pressure Off Your Foot Ulcer
Foot ulcers are partly caused by too much pressure on one part of your foot.
Your provider may ask you to wear special shoes, a brace, or a special cast. You may need to use a wheelchair or crutches until the ulcer has healed. These devices will take the pressure off of the ulcer area. This will help speed healing.
Sometimes putting pressure on the healing ulcer for even a few minutes can reverse the healing that happened the whole rest of the day.
Be sure to wear shoes that do not put a lot of pressure on only one part of your foot.
- Wear shoes made of canvas, leather, or suede. Don’t wear shoes made of plastic or other materials that don’t allow air to pass in and out of the shoe.
- Wear shoes you can adjust easily. They should have laces, Velcro, or buckles.
- Wear shoes that fit properly and are not too tight. You may need a special shoe made to fit your foot.
- Don’t wear shoes with pointed or open toes, such as high heels, flip-flops, or sandals.
Insurance Coverage For Pure Oxygen Treatment Is Limited But Expanding
The Food and Drug Administration considers the oxygen delivery product, a class II medical device, to which it granted premarketing clearance in 2009.
The therapy is available now in limited areas of the country but the company is working to gain broader availability, says Mike Griffiths, DProf, CEO and medical director of AOTI Inc. based in Oceanside, California, and Galway, Ireland.
This therapy is now prescribed in Veterans Administration facilities, he says, and ”we have approval for New York State Medicaid reimbursement.” He declined to provide the cost to a patient who doesnt have insurance coverage, but he says the new study results is expected to help the company get broader healthcare coverage from Medicare and other insurers soon.
You May Like: Stomach Ulcer Treatment Over The Counter
What Types Of Physicians Specialize In Treating Diabetic Foot Ulcers
The doctors that are qualified to treat diabetic foot ulcers include wound care specialists, orthopedic surgeons, vascular surgeons, and endocrinologists.
- Wound care specialists are clinicians who have received specialized training in caring for and treating all wounds, both acute and chronic. One of the most treated wounds are diabetic wounds. The percentage of these wounds that become stubborn and refuse to heal is high. This creates an issue with the patients quality of life.
- Podiatrists are foot health specialists who are specially trained in treating all injuries and illnesses pertaining to the feet, including the diagnosis and treatment of diabetic ulcers.
- Orthopedic surgeons can offer prevention measures to patients who have diabetic foot ulcers. Long-term protection of the feet is provided to patients by Orthopedists subscribing footwear that will protect them in the future. The surgeon can also correct bunions, hammertoes, and deformities in the feet to avoid the formation of an ulcer.
- A vascular surgeon does not directly treat diabetic foot ulcers. They are involved in the treatment of peripheral arterial disease, which is a critical catalyst for the impediment of blood flow to the lower legs and feet.
- Endocrinologists are specially trained physicians who address several conditions, including diabetes. An endocrinologist will be the doctor who will make referrals to the other specialists mentioned here.
Recommended Reading: Does Type 2 Diabetes Need Insulin
Diabetic Foot Ulcers: Prevention Diagnosis And Classification
DAVID G. ARMSTRONG, D.P.M., and LAWRENCE A. LAVERY, D.P.M., M.P.H., University of Texas Health Science Center at San Antonio and the Diabetic Foot Research Group, San Antonio, Texas
Am Fam Physician. 1998 Mar 15 57:1325-1332.
See related patient information handout on maintaining healthy feet in diabetics, written by the authors of this article.
Diabetic foot complications are the most common cause of nontraumatic lower extremity amputations in the industrialized world. The risk of lower extremity amputation is 15 to 46 times higher in diabetics than in persons who do not have diabetes mellitus.1,2 Furthermore, foot complications are the most frequent reason for hospitalization in patients with diabetes, accounting for up to 25 percent of all diabetic admissions in the United States and Great Britain.35
The vast majority of diabetic foot complications resulting in amputation begin with the formation of skin ulcers. Early detection and appropriate treatment of these ulcers may prevent up to 85 percent of amputations.6,7 Indeed, one of the disease prevention objectives outlined in the Healthy People 2000 project of the U.S. Department of Health and Human Services is a 40 percent reduction in the amputation rate for diabetic patients. Family physicians have an integral role in ensuring that patients with diabetes receive early and optimal care for skin ulcers.
Read Also: What Will Help Stomach Ulcer Pain
New Wound Therapytopical Pure Oxygenappears Effective In Healing Food Ulcers
Investigators from Midwestern University invited 73 people who had diabetes, both type 1 and 2, to participate in a study to test this new treatment for diabetic foot ulcers.
They found that nearly 42% of those who were randomly assigned to receive the oxygen therapy experienced significant symptom relief, compared to just 13.5% of those who were treated with regular room air for 12 weeks.2
This new food ulcer therapy is called TWO2 for Topical Wound Oxygen home care therapy. The treatment involves placing an inflatable chamber, similar to a large stocking, over the wound, and then an oxygen generator fills the chamber with pure oxygen administered under pressure.2
As a result of the oxygen therapy, Dr. Frykberg says, “it stimulates production of collagen, growth factor, new blood vessels and increased ability to fight infection.”
Oxygen has long been viewed as crucial in the wound-healing process,3-7 the researchers say. For years, hyperbaric oxygen therapy has been studied intensely to heal foot ulcers and prevent amputation. But results remain inconsistent, the researchers say.
However, Dr. Frykberg and his colleagues say that the use of topically administered oxygen therapy has been hampered by studies that weren’t well designed and complicated by results that were inconsistent.8-10
Why Is Foot Ulcers Healing Slow
When you have diabetes, several factors can affect your bodys ability to heal ulcers. A diabetic foot ulcer has various causes, often including external ischemia, neuropathy, or both. A few of them include:
- High blood sugar levels
- Immune system deficiency
- Infection
If you get an ulcer or notice any change in your skin that youre unsure about, consult a doctor, could be a primary doctor or a diabetes specialist. A debridement procedure will be given to the infected area, removing unhealthy tissue from the wound to spur healing. The doctor will also work with you to keep your sore or ulcer from getting infected and becoming more significant.
If the foot ulcer doesnt heal within a month or the infection spreads to the bone, in this case, patients may need other treatments. These can include surgery and hyperbolic oxygen therapy to help the body heal.
Don’t Miss: Boost Vs Ensure Ulcerative Colitis
Treatment Management & Guidelines
Treatment: People with diabetes have more risk of foot ulcers. Foot ulcers are the main reason for leg amputations worldwide. Immediately treating foot ulcers is therefore necessary. Treatment varies from person to person condition and this includes:
Medication: Medicine treatment includes:
- Antibiotics to control infection of sore or wound
- Anticlotting medicines to reduce blood clots and improve blood circulation
- Diabetic control medicines to control diabetes.
- Painkillers to relieve pain due to foot ulcers.
Surgical options: Surgery may include:
Summary:
Foot ulcer treatment includes antibiotics and anti-clotting medicines, and it may require surgeries for increasing blood flow.
Management: Management of foot ulcers consists of providing relief from the ulcer pain or itching and to stop its growth. This includes:
Summary:
Cleveland Clinic Heart Vascular & Thoracic Institute Vascular Medicine Specialists And Surgeons
Choosing a doctor to treat your vascular disease depends on where you are in your diagnosis and treatment. The following Heart, Vascular & Thoracic Institute Sections and Departments treat patients with all types of vascular disease, including blood clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular disease. In addition, the Non-Invasive Laboratory includes state-of-the art computerized imaging equipment to assist in diagnosing vascular disease, without added discomfort to the patient. Call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an appointment online.
Department of Vascular Surgery: surgery evaluation for surgical treatment of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, toll-free 800-223-2273, extension 44508 or request an appointment online.
You may also use our MyConsult second opinion consultation using the Internet.
The Heart, Vascular & Thoracic Institute also has specialized centers and clinics to treat certain populations of patients:
Read Also: Liver Disease Associated With Ulcerative Colitis
Q: What Causes Heel Pain
A: Typically, heel pain is not caused by one single incident or injury, and the most common cause is plantar fasciitis, which can lead to long-term pain that may one day require surgical treatment if not corrected.
Repetitive stress/pounding of the heel can cause heel pain.
Other common causes can include inflammation of the plantar fascia, inflammation of the back of the heel, inflammation of the heel pad, progressive degeneration of the Achilles tendon, or a stress fracture caused by repetitive stress to the heel.
Peripheral Arterial Occlusive Disease
Peripheral arterial occlusive disease is four times more prevalent in diabetics than in non-diabetics.11 The arterial occlusion typically involves the tibial and peroneal arteries but spares the dorsalis pedis artery.12 Smoking, hypertension and hyperlipidemia commonly contribute to the increased prevalence of peripheral arterial occlusive disease in diabetics.13,14
The presence of lower extremity ischemia is suggested by a combination of clinical signs and symptoms plus abnormal results on noninvasive vascular tests. Signs and symptoms may include claudication, pain occurring in the arch or forefoot at rest or during the night, absent popliteal or posterior tibial pulses, thinned or shiny skin, absence of hair on the lower leg and foot, thickened nails, redness of the affected area when the legs are dependent, or dangled, and pallor when the foot is elevated.
The sensitivity and specificity of noninvasive vascular tests are a matter of some controversy. Commonly accepted abnormal values for transcutaneous oxygen measurement, ABI determinations and toe systolic pressure are given in Table 2. The noninvasive tests have been faulted for underestimating the severity of arterial insufficiency.18 If lower extremity ischemia is strongly suspected, arteriography or some other imaging study should be performed to confirm or rule out ischemia.
|
Less than 40 mm Hg |
|
|
Ankle-brachial index |
|
|
Less than 0.45: severe, limb-threatening |
|
|
Absolute toe systolic pressure |
Less than 45 mm Hg |
Recommended Reading: What Not To Eat If You Have An Ulcer
Tea Tree Oil To Fight The Infection
Tea tree oil is rich in antibacterial properties. You can mix the tea tree oil in equal quantity with coconut oil and use it for dressing the diabetic foot ulcer. You can even keep the wound open for some time after applying the tea mixture of tea tree and coconut oil. This home treatment of diabetic foot hastens the process of healing of the wound.