Complications Of Liver Disease
In some cases, liver disease is first discovered when it starts to cause complications, such as:
- Fluid buildup in the legs or the abdomen
- Excessive bruising and bleeding
- Jaundice, which is yellowing of the eyes and skin caused by the buildup of bilirubin
- Itching, which is caused by a buildup of bile in the skin
- Gallstones, which develop when bile is blocked from entering the gallbladder
- Toxin buildup in the blood and the brain
- Medication sensitivity caused by the inability of the liver to process drugs
- Portal hypertension, which is an increase in blood pressure in a vein called the portal vein
- Varices, which are enlarged blood vessels caused by the slow blood flow through the portal vein
- Various other complications such as immune system dysfunctions, infections, and kidney problems
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Common Hepatobiliary Manifestations Of Ibd
Hepatic Steatosis is one of the more common hepatobiliary manifestations of IBD found in patients with Crohns disease and ulcerative colitis. This is characterized by large collections of fat droplets found within liver cells seen when tissue from a liver biopsy is analyzed. Hepatic Steatosis may also be seen with abdominal ultrasound with the liver appearing large and fatty. There are usually no signs or symptoms, or laboratory abnormalities to suggest fatty infiltration of the liver. As well, the presence of hepatic steatosis is usually benign and usually does not present with any further complications. However, one must realize that fatty infiltration can be directly related to the severity of the IBD, and also to malnutrition and corticosteroid use. As the IBD improves and better nutritional status is maintained then the fatty infiltration may improve and be reversible.
You May Like: Ulcerative Colitis And Back Pain
Who Is At Risk Of Ulcerative Colitis
- Age: Ulcerative colitis may affect any age group, although there are peaks at ages 15 to 30 years, and again at ages 50 to 70 years.
- Race/ethnic background: Ulcerative colitis is more common among caucasians and in people of Ashkenazi Jewish descent.
- Family history: People with a first-degree relative with ulcerative colitis are at greater risk of developing the condition.
Animals And Experimental Protocol

Male C57BL/6 mice were obtained from Laboratory Animal Centre of Hebei Medical University . All mice were maintained under standard conditions , and free access to food and water. All experimental protocols were conducted according to the Institutional Animal Care guidelines and approved by the Laboratory Animal Ethics Committee of Hebei Medical University.
You May Like: What To Do For Ulcer Pain
Mechanism Of Ulcerative Colitis
- 1Department of Gastroenterology, The Second Hospital of Hebei Medical University, Shijiazhuang, China
- 2Department of Gastroenterology, Dingzhou Peoples Hospital of Hebei Province, Dingzhou, China
Background: The progression of liver disorders is frequently associated with inflammatory bowel disease through the gut-liver axis. However, no direct evidence showed the mechanisms of ulcerative colitis in the development of liver fibrosis per se. Thus, this study aimed to evaluate the effects of UC on liver fibrosis and its potential mechanism in the experimental model.
Methods: Male C57BL/6 mice were allocated into five groups to receive either drinking water , 2% dextran sulfate sodium , olive oil, carbon tetrachloride or DSS + CCl4 for 4 cycles. Blood was collected for biochemical analysis. Colons were excised for the evaluation of colon length and morphological score. Liver, colon, and mesenteric lymph nodes were collected for histopathological staining, expression analysis, and bacterial translocation assay to evaluate the inflammation, fibrosis, the activation of hepatic stellate cells , and gut barrier function.
The present study verified that UC aggravated CCl4-induced liver injury, inflammation, and fibrosis in mice through the gut-liver axis. Gut barrier dysfunction in UC leads to bacterial translocation and elevated lipopolysaccharide, which may promote the activation of TLR4 signaling and HSCs in the liver.
Colitis Score And Histological Score
The revised versions of both scores of Kajiya et al. were used. We blindly evaluated for both. For the colitis score, the weight loss rate, stool hardness, and anal bleeding were quantified as shown in Table . Weight loss was divided into five categories based on the degree of reduction rate. Stool hardness and anal bleeding were classified into three categories according to the following criteria: Stool hardness was classified according to the shape of the stool and the presence or absence of stool adhesion to the anus, and anal bleeding was classified according to the degree of bleeding . The average value of the numerical values of the above three items was used as the colitis score. The colitis score was 0 when healthy and 4 when colitis was maximally active.
For the histological score, the epithelial tissue disorganization, crypt disorganization, immunocyte invasion, and erythrocyte invasion were quantified as show in Table . The epithelial tissue disorganization and crypt disorganization were divided into five categories according to the degree of disorganization of each tissue. Immunocyte invasion and erythrocyte invasion were divided into five categories according to the degree of invasion in the large intestine. Each item in the histological colitis score was 0 when healthy and 4 when colitis was maximally active.
You May Like: Can I Donate Blood If I Have Ulcerative Colitis
Dss Induced The Intestinal Inflammation In Ccl4
To investigate the mechanism of UC in liver fibrosis, liver fibrosis mouse models with intestinal inflammation were established. After that, the severity of intestinal inflammation was evaluated using the indexes including body weight loss, DAI score, histopathological indicators and the expression of proinflammatory cytokines in colon. As shown in Figure 1A, body weights of mice in DSS and CCl4 groups decreased significantly compared to mice in their corresponding control group . Notably, we found that DSS treatment significantly aggravated the CCl4-induced body weight loss . Meanwhile, an obvious increase of DAI score were found in DSS and CCl4 groups compared to their controls . Moreover, the increase of DAI after CCl4 induction were further enhanced by DSS treatment .
Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
Also Check: Probiotics Good For Ulcerative Colitis
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Impact Of Uc Activity On Psc Recurrence After Liver Transplantation
The presence of active inflammation in the colon may increase the risk of recurrence of PSC in the allograft. A previous study showed that use of corticosteroids to treat IBD flares following OLT may be associated with recurrence of PSC in the allograft . Aggressive measures to prevent colon inflammation in the post-OLT setting may be required to protect the liver from recurrence of PSC.
Don’t Miss: What To Eat And Drink If You Have An Ulcer
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Be underweight
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Diet And Lifestyle Changes

Although diet and stress do not cause ulcerative colitis, there may be times when changes in your lifestyle may help control your symptoms and lengthen the time between flare-ups. The following changes may help to ease your symptoms:
- Limit milk/dairy products. If you are lactose intolerant , milk and dairy products can produce symptoms of excess gas and diarrhea.
- Restrict intake of certain high-fibre foods: such as nuts, seeds, and raw vegetables.
- Limit intake of caffeine, alcohol, carbonated drinks and fatty foods. .
- Eat small, frequent meals, rather than large meals..
- Exercise regularly to promote movement of the colon and reduce stress..
- Minimize stress. Yoga, meditation and slow, relaxed breathing techniques can help people with ulcerative colitis manage stress..
Ask your doctor or pharmacist if one of these formulations may be right for you. It is important to take the probiotic in the dose and duration recommended by the manufacturer to achieve the best results.
Also Check: Wheatgrass Spray For Leg Ulcers
Primary Sclerosing Cholangitis And Colon Cancer
Patients with IBD have a significantly increased risk of developing CRC, mainly because of the pro-neoplastic effect secondary to chronic intestinal inflammation. The risk is greater if there is an association with PSC.20 In 77 patients with PSC-IBD, CRC was detected in 7.8% versus 2.3% in the control group .13 Interestingly, in PSC-UC, all colorectal tumours were located proximal to the splenic flexion. In UC without PSC, tumour location was predominantly in the left colon.
Additional risk factors for the development of CRC include the duration of the disease and the extent of IBD . In a comparative study, 46 of 273 patients with PSC , it was established that patients with UC had a 56% higher risk of developing CRC compared to CD.21
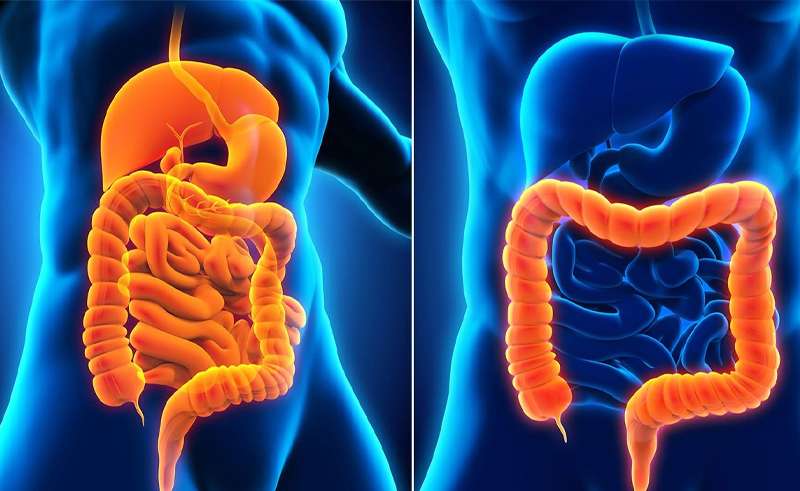
What Is Ulcerative Colitis
Ulcerative colitis is a chronic disorder affecting the large intestine . The digestive system converts food into nutrients and absorbs them into the bloodstream to fuel our bodies. The colons main role is to absorb water and salts from undigested food waste. This action helps to thicken and solidify the stool, which is then expelled from the body through the anus.
Ulcerative colitis causes inflammation and ulceration along the lining of the colon which can lead to abdominal pain, cramps, bleeding and diarrhea. The disease usually begins in the rectal area, which holds stool until you go to the bathroom, and may involve the entire colon over time. Ulcerative colitis is classified as an inflammatory bowel disease , due to the inflammation that occurs in the intestines. Another common form of IBD is called Crohns disease. Although the symptoms of ulcerative colitis are similar to Crohns disease, the conditions are different in several ways.
While both ulcerative colitis and Crohns disease are types of IBD, they should not be confused with Irritable Bowel Syndrome , a disorder that affects the muscle contractions and the sensitivity of the colon. Unlike ulcerative colitis and Crohns disease, IBS does not cause intestinal inflammation nor damage the bowel.
Recommended Reading: What Foods Irritate An Ulcer
Testing For Ulcerative Colitis
Often, symptoms alone can provide doctors with the information they need to diagnose ulcerative colitis. Your doctor will perform a physical examination and take a complete medical history that includes a careful review of your symptoms. For this reason, it is important to be candid and specific with your doctor about the problems you are having.
There is no one specific laboratory test, X-ray or scope to diagnose ulcerative colitis, however, to help confirm the condition and rule out other problems, your doctor may send you to have one or more of the following tests:
Ibd And Liver Disease
Inflammatory Bowel Disease is often associated with other diseases that develop alongside intestinal and perianal involvement. These other diseases are called extraintestinal manifestations of IBD. Extraintestinal organ systems that may be involved with IBD are listed in below. The associations of these manifestations with IBD have been recognized for many years but are not well known in terms of the mechanisms, or cellular changes that occur in the development of the disease.
Read Also: How To Heal Ulcers In Large Intestine
What Complications Are Associated With Ulcerative Colitis
Yes. There are some complications related to ulcerative colitis. Possible complications include:
- Severe bleeding
- Perforated colon
- Kidney stones
- Osteoporosis
- Toxic megacolon
- Liver disease
People with ulcerative colitis are also at increased risk of developing colon cancer. The risk of colon cancer is related to the length of time since you were diagnosed and how much of your colon is affected by inflammation. However, a regular examination by your doctor and colorectal cancer screening tests can help to reduce the risk of cancer and detect problems early.
Liver Conditions Linked To Ulcerative Colitis
There’s more than just proximity between your colon and your liver. Find out about ulcerative colitis and liver disease risks.
Yaroslav Danylchenko/Stocksy Everyday Health
Liver disease can be a complication of inflammatory bowel disease , such as ulcerative colitis or Crohns disease. The liver, which processes the food you ingest, can develop inflammation if IBD isnt treated appropriately. Unfortunately, some drugs used to treat IBD may also damage the liver.
According to a study published in 2019 by the American Gastroenterological Association, the prevalence of nonalcoholic liver diseases in patients with UC was more than double that of the general population. Considering the increased risk, it makes sense to take precautions. Laura Raffals, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota, recommends that people with UC have their liver enzymes checked annually. Its also wise to be aware of the common symptoms of liver disease so you can address the problem before it gets worse. According to the Crohns & Colitis Foundation, these symptoms include the following:
- Fatigue or low energy
- Jaundice
- Pain or a feeling of fullness in the upper right abdomen
- Fluid retention
- Easy bruising
Here are five conditions related to the liver or ducts that transport bile that may develop alongside ulcerative colitis.
Also Check: Best Treatment For Diabetic Foot Ulcer
Liver And Gallbladder Disease
Primary sclerosing cholangitis causes narrowing of the bile ducts in the liver and is closely associated with UC. Roughly 4 percent of people with UC develop PSC, and 60 percent to 80 percent of people with PSC develop a form of IBD. Currently, there is no effective treatment for PSC.
People with IBD are also more prone to develop gallstones and hepatic steatosis , which are treatable with ursodeoxycholic acid, a bile acid. PSC also increases the risk of developing bile duct cancer . In addition, having both IBD and PSC increases the risk of colorectal cancer. Close follow-up and colonoscopy can help monitor for the development of cancer in high-risk individuals.
Causes Of Cirrhosis Of The Liver
In people with IBD, cirrhosis could be caused by autoimmune hepatitis or primary biliary cirrhosis. Autoimmune hepatitis is associated with a dysfunctional immune system. Primary biliary cirrhosis is an inflammation of the bile ducts that can inhibit bile from leaving the liver and going to the small intestine. When the bile gets backed up it can cause further damage to liver tissues. Primary sclerosing cholangitis, which is largely associated with ulcerative colitis, can also overlap with autoimmune hepatitis .
Also Check: Can Ulcerative Colitis Cause Eye Problems
What Is The Liver
The liver, which is the largest organ in the body, provides several important functions without which the body can not survive. The liver removes impurities and foreign bodies from the blood, makes the proteins that help blood clot, and produces bile. When disease interferes with the functioning of the liver, it can cause significant medical problems.