Inflammation And Your Immune System
Inflammation is your immune systems normal reaction to protect your body from bacteria, viruses, and other potentially harmful substances. However, for people with UC, the immune system is mistakenly triggered to attack the inner lining of the large intestine. This results in excess inflammation, leading to the symptoms of UC.
Although it isnt known for sure what triggers the excess inflammation, too much of the protein TNF alpha may be to blame. Your bodys immune system naturally produces TNF alpha, but if you have UC, your body may be producing too much of it.
What Makes Yale Medicines Approach To Ulcerative Colitis Stand Out
At our Inflammatory Bowel Disease Program, we know the key to properly managing a patients disease is coordinating care among our specially trained physicians. Our program offers expertise in gastroenterology, surgery, pathology and radiology.
We have a team approach with doctors, physician associates, nurses and surgeons all working together, Dr. Proctor says. Plus, we have more than 25 years of experience to help our patients.
A goal is to empower people with ulcerative colitis to take an active role in their health care and improving their quality of life. To this end, Yale Medicine care providers work hard to educate patients about their disease. In our Inflammatory Bowel Disease Program, a dedicated APRN works closely with patients to offer nutritional resources, medication and surgical options and discuss topics like pregnancy and IBD and depression and chronic disease.
The Main Types Of Drugs
The aim of drug treatment for Ulcerative Colitis is to reduce inflammation. The main types of drugs are:
Aminosalicylates reduce inflammation in the lining of the intestine. Examples include mesalazine , olsalazine , sulphasalazine and balsalazide .
Corticosteroids work by blocking the substances that trigger allergic and inflammatory responses in your body. They include prednisolone, prednisone, methylprednisolone, budesonide , hydrocortisone and beclometasone dipropionate .
Immunosuppressants suppress the immune system, and reduce levels of inflammation. The main immunosuppressants used in IBD are azathioprine , mercaptopurine or 6MP , methotrexate, ciclosporin and tacrolimus. They are often used in patients who relapse when they come off steroids.
Biological drugs are the newest group of drugs used to treat IBD. Anti-TNF drugs, such as infliximab , adalimumab and golimumab target a protein in the body called TNF, or tumor necrosis factor, preventing inflammation. Another type of biological drug is vedolizumab , which works by stopping white blood cells from entering the lining of the gut and causing inflammation.
You can find more information about some of the drugs used for Colitis: Adalimumab, Aminosalicylates , Azathioprine and Mercaptopurine, Biologic Drugs, Golimumab, Methotrexate, Infliximab, Steroids, Ustekinumab and Vedolizumab.
About a quarter of people diagnosed with Crohn’s or Colitis are children or adolescents at the time they are diagnosed.
Read Also: What Foods Should I Avoid With A Stomach Ulcer
Allergic Colitis In Infants
Allergic colitis is a condition that can occur in infants, usually within the first months after birth. The condition can cause symptoms in infants including:
- reflux
- fussiness
- possible flecks of blood in a babys stool
Doctors dont know exactly what causes allergic colitis. One of the most popular theories is that infants with allergic colitis have an allergic or hypersensitive reaction to certain components in breast milk. A 2020 review of studies indicated that a protein allergy, either through breast milk, cows milk, or formula, could contribute.
Eosinophilic colitis is a type of allergic colitis that can also show up in infants with these symptoms. Its causes are similarly unknown , but its likely also related to a protein allergy.
Doctors will often recommend an elimination diet for the birthing parent, which involves slowly cutting out certain foods known to contribute to allergic colitis. Examples include cows milk, eggs, and wheat. If the baby stops having symptoms of allergic colitis, these foods were likely causing the problem.
In severe cases, monoclonal antibodies, such as those used to inflammatory bowel disease , may also be another treatment option.
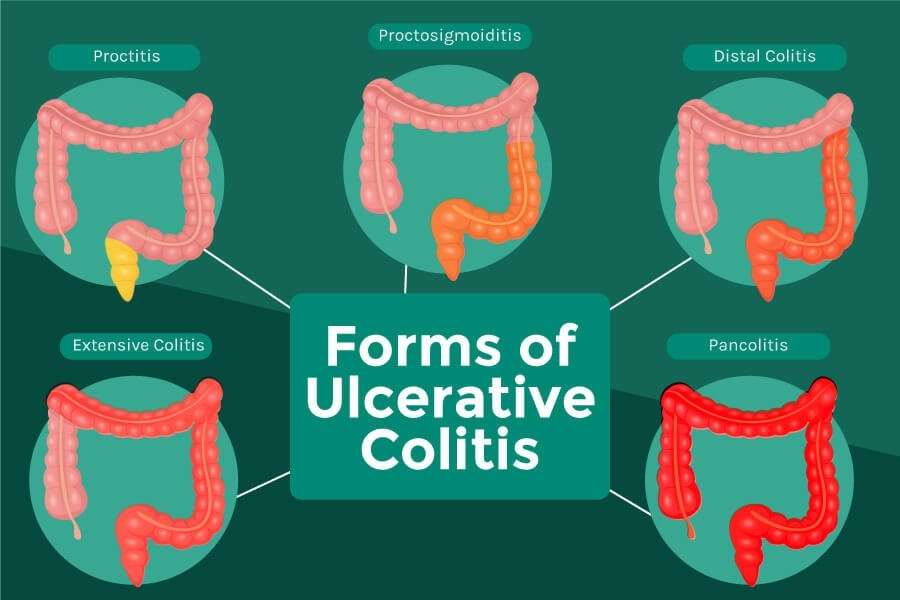
What Are The Types Of Ulcerative Colitis
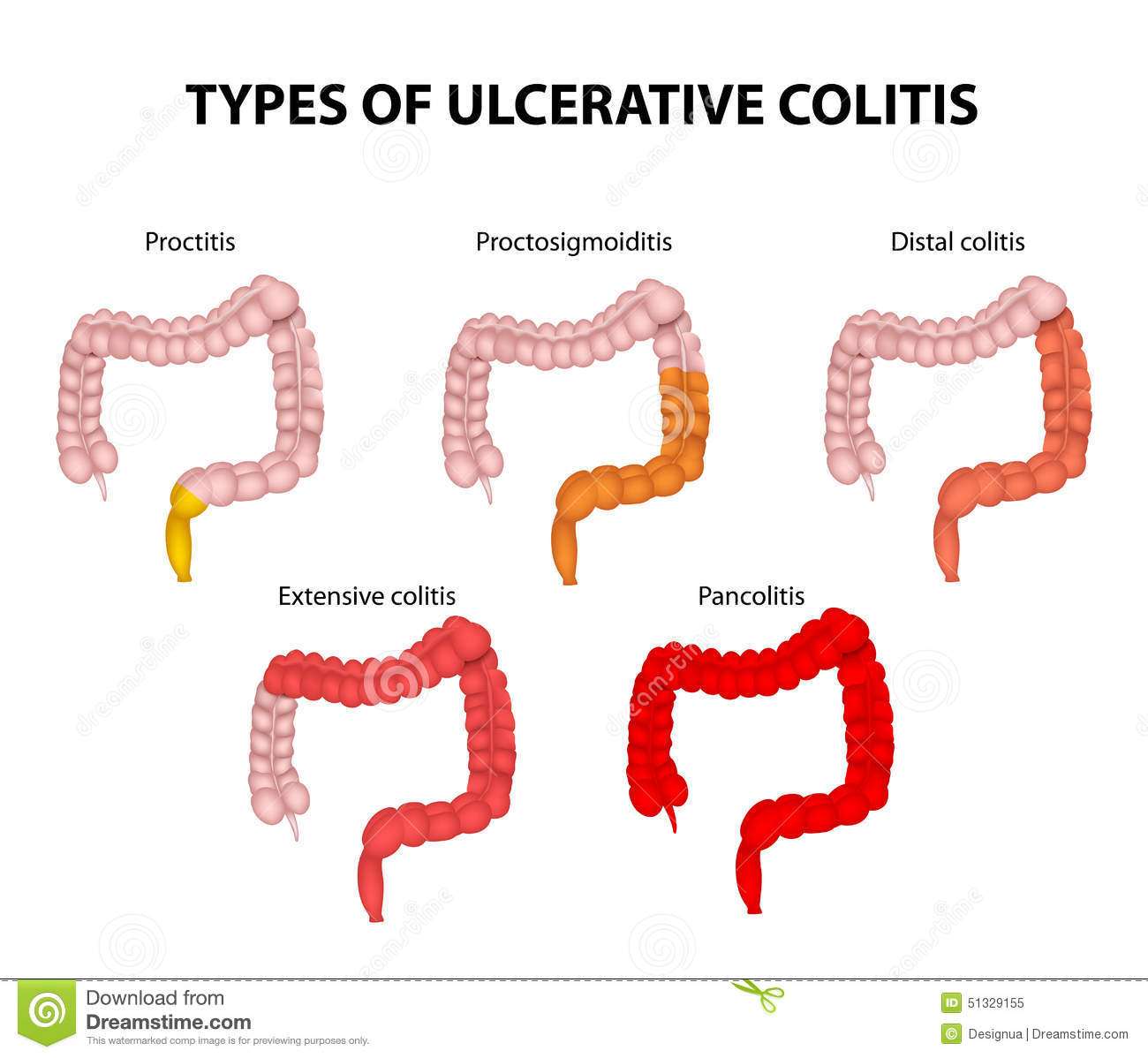
Another way to categorize ulcerative colitis is by identifying what areas of the colon it affects, as seen in a colonoscopy. According to Stein, UC always affects the rectum, the lowest section of the colon. But it may also affect higher parts of the colon.
There are four main types of UC based on how much of the rectum and the colon are affected:
Ulcerative Proctitis This form of UC usually affects less than six inches of the rectum and is found in about 30 percent of people at the time of diagnosis. Because of its limited extent, it tends to be associated with less severe disease and fewer complications.
Proctosigmoiditis This form of UC affects the rectum as well as the sigmoid colon, located just above the rectum. Proctosigmoiditis tends to be more severe than ulcerative proctitis, frequently causing symptoms such as bloody diarrhea, cramps, and tenesmus .
Left-Sided Colitis Inflammation extends even farther up the colon in this form of UC, to a point where it bends near the spleen. It tends to be even more severe, with common symptoms including diarrhea, bleeding, loss of appetite, weight loss, and severe abdominal pain on the left side.
Pan-Ulcerative Colitis This form of UC involves inflammation throughout the entire colon and tends to be the most severe variation with the greatest risk of complications that require surgery. Symptoms often include severe diarrhea, bleeding, cramps, abdominal pain, and weight loss.
Recommended Reading: Side Effects Of Ulcerative Colitis
Medications For Ulcerative Colitis
No medicine can cure UC. The goal of medication is to make a patients ulcerative colitis manageable. People with UC may have to take medicines indefinitely to control their condition.
Medications for treating ulcerative colitis:
- Aminosalicylates
- These medications may be used in people with mild or moderate symptoms and most people can tolerate them. They contain an active ingredient called 5-aminosalisylic acid, or 5-ASA, which helps control inflammation. Drugs in this class include balsalazide, mesalamine, olsalazine and sulfasalazine.
- Corticosteroids
- More commonly known simply as steroids, these medicines reduce the immune systems response. They are used if aminosalicylates dont seem to work. Drugs in this class include prednisone, methylprednisone, hydrocortisone and budesonide. These drugs shouldnt be used long-term.
- Immunomodulators
- These drugs reduce immune system activity as well, but may take as long as three months to work. Immunomodulators include Azasan or Imuran and Purinethol or Purixan .
- Biologics or TNF therapy
- This group includes Humira , Simponi and Remicade , medications that decrease inflammation by targeting a protein made by the immune system called tumor necrosis factor, or TNF. Side effects of these medications include higher risks for tuberculosis, fungal infections, skin cancer and psoriasis.
Doctors may also recommend antibiotics to prevent infection and other medications to treat diarrhea.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Also Check: How Do I Know If I Have A Peptic Ulcer
Outcome And Complications From Ileoanal Anastomosis
Complications are common with any intestinal operation. In a small percentage of IPAA procedures, complications occur that require conversion to an ileostomy.
Pouchitis
Inflammation of the pouch is the most common complication of the pouch procedures. Symptoms include rectal bleeding, cramps, and fever. It can usually be successfully treated with antibiotics such as metronidazole or ciprofloxacin .
Bowel obstruction
Bowel obstruction may occur although it is less common than pouchitis. With most people, this condition can be treated by avoiding food for several days and administering intravenous fluids. In some cases of bowel obstruction, surgery may need to be performed to remove the blockage.
Pouch failure
Pouch failure occurs in a small percentage of people. It requires permanent removal of the pouch and use of ileostomy.
Irritable Pouch Syndrome
Irritable pouch syndrome is a problem that includes frequent bowel movements, an urgent need to defecate, and abdominal pain. However, there are no signs of inflammation as there are with pouchitis. Stress and diet play a role in this condition, and it is usually relieved after a bowel movement.
Infertility
IPAA can cause infertility in women because the surgery can scar or block the fallopian tubes.
Are There Any Special Dietary Requirements For Persons With Ulcerative Colitis
Although it seems plausible that a specialized diet might benefit patients with ulcerative colitis, there is actually no evidence to support treatment with dietary modification. Despite extensive research, no diet has been found to slow progression, treat, or cure the disease. It is recommended that patients stay on a balanced, healthy diet rich in fruits, vegetables, grains, lean meats, beans, fish, eggs, nuts. Patients should also try to limit foods with saturated fatshigh cholesterol. During flare-ups, patients should continue to eat as tolerated. The Crohn’s and Colitis Foundation of America recommends a bland diet with soft food during a flare including hot cereals, boiled eggs, mashed potatoes, steamed vegetables, canned or cooked vegetables to minimize discomfort.
Recommended Reading: How To Check A Horse For Ulcers
Symptoms Beyond The Intestine
When ulcerative colitis is raging, it can take its toll on more than just the GI tract.
The inflammation from ulcerative colitis can make patients feel very fatigued lead to blood loss, causing anemia and cause weight loss due to difficulty absorbing nutrients, says Dr. Ather.
Symptoms beyond the intestine affect mental health and quality of sleep, too. A study published in 2018 in the International Journal of Behavioral Medicine found higher rates of mental health and sleep disorders in people with ulcerative colitis.
It is important for us to screen for these issues and refer our patients to get the help they need, Dr. Ather says.
What Are Immunomodulator Medications
Immunomodulators are medications that weaken the body’s immune system. The immune system is composed of immune cells and the proteins that these cells produce. These cells and proteins serve to defend the body against harmful bacteria, viruses, fungi, and other foreign invaders. Activation of the immune system causes inflammation within the tissues where the activation occurs. Normally, the immune system is activated only when the body is exposed to harmful invaders. In patients with Crohn’s disease and ulcerative colitis, however, the immune system is abnormally and chronically activated in the absence of any known invader. Immunomodulators decrease tissue inflammation by reducing the population of immune cells and/or by interfering with their production of proteins that promote immune activation and inflammation. Generally, the benefits of controlling moderate to severe ulcerative colitis outweigh the risks of infection due to weakened immunity. Examples of immunomodulators include azathioprine , 6-mercaptopurine , cyclosporine , and methotrexate .
Azathioprine and 6-MP
Azathioprine and 6-MP are increasingly recognized by doctors as valuable drugs in treating Crohn’s disease and ulcerative colitis. Some 70% of patients with moderate to severe disease will benefit from these drugs. Because of the slow onset of action and the potential for side effects, however, 6-MP and azathioprine are used mainly in the following situations:
Other Issues in the Use of 6-MP
Methotrexate
Read Also: Does Smoking Cause Ulcers After Gastric Bypass
What Are The Risk Factors Of Ulcerative Colitis
The cause of ulcerative colitis is unclear, but its thought that a combination of genetics and environmental factors are at play. Up to 20 percent of people with ulcerative colitis have a parent, sibling or child with the disease.
Ulcerative colitis is more common for people living in urban, industrialized areas compared to undeveloped countries, which indicates that highly refined diets may play a role. Although all ethnic groups are affected, the problem is most common among Caucasians and people of Eastern European Jewish descent.
Lastly, there appears to be a connection to nonsteroidal anti-inflammatory medications. Its not that these medications cause the disease but, because they inflame the bowel, they can worsen symptoms. This category of medication includes ibuprofen , naproxen sodium and diclofenac sodium .
Complications Outside The Intestine
Bones
Ulcerative colitis, and the corticosteroid and immune-suppressing drugs used to treat it, can cause osteopenia and osteoporosis . Osteoporosis is more common with Crohn disease than with ulcerative colitis.
Liver and Gallbladder Disorders
In severe cases, IBD can cause problems with the liver and pancreas and increase the risk for gallstones. In addition, patients with IBD are at increased risk of developing primary sclerosing cholangitis. This is a disease of the bile ducts in the liver that eventually leads to liver failure and the need for liver transplantation.
Thromboembolism
People with inflammatory bowel disease are at higher risk for blood clots, especially deep venous thrombosis where blood clots form in the legs. They are also at risk for pulmonary embolism, when a blood clot travels from the legs to the lungs.
Urinary Tract and Kidney Disorders
IBD may increase the risk for urinary tract and bladder infections. People with IBD have an increased risk for kidney stones.
Delayed Growth and Development in Children
Children with ulcerative colitis are at slightly higher than average risk for delayed growth, but their risk is lower than with Crohn disease.
Emotional Factors
Read Also: L Glutamine Ulcerative Colitis Dosage
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohn’s and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohn’s or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Also Check: Snack Ideas For Ulcerative Colitis
What Causes Ulcerative Colitis
Autoimmune disorders are not fully understood and the medical community isnt quite sure exactly how a person gets ulcerative colitis. But doctors and researchers have found that a variety of genetic and environmental factors may play a role in the case of UC.
Genetic Causes
Ulcerative colitis seems to run in some families. Studies have identified variations in genes that may play a role in causing UC, but researchers arent sure exactly how these genetic differences are directly linked to the condition.
Overactive Intestinal Immune System
The immune system protects the body by reacting to harmful invaders such as viruses, bacteria and other threats. Researchers believe these invaders may confuse the immune system, tricking it into launching an immune response in the lining of the large intestine, causing UC.
Environmental Causes
Most research suggests environmental factors may increase the chance of developing ulcerative colitis, but believe the risk is low. High-fat diets may trigger UC in some people. Individuals may notice specific foods cause a reaction for them.
Some drugs may also increase a persons risk. Nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen , naproxen and Celebrex may increase a persons risk. Anti-acne drug Accutane has been blamed for increased UC risk. Antibiotics and oral contraceptives are also suspected of slightly increasing a persons ulcerative colitis risk.
Emotional Stress
What Research Is Being Done Regarding Ulcerative Colitis
Active research is also ongoing to find other biological agents that are potentially more effective with fewer side effects in treating ulcerative colitis including adalimumab, visilizumab, and alpha-4 integrin blockers.
Research in ulcerative colitis is very active, and many questions remain to be answered. The cause, mechanism of inflammation, and optimal treatments have yet to be defined. Researchers have recently identified genetic differences among patients which may allow them to select certain subgroups of patients with ulcerative colitis who may respond differently to medications. Newer and safer medications are being developed. Improvements in surgical procedures to make them safer and more effective continue to emerge.
Health Maintenance
It is recommended that adults with inflammatory bowel disease generally follow the same vaccination schedules as the general population.
Osteoporosis has also increasingly been recognized as a significant health problem in patients with IBD. IBD patients tend to have markedly reduced bone mineral densities. Screening with a bone density study is recommended in:
- postmenopausal woman,
Don’t Miss: How Long Does An Ulcerative Colitis Flare Up Last