Updates In Part : Management Of Pediatric Ulcerative Colitis
There are no major updates in the management of acute severe pediatric colitis cases. The new updates in the revised guidelines include:
- The new guidelines emphasise on the practice of therapeutic drug monitoring the use of thrombotic prophylaxis.
- As per the new guidelines, sequential therapy should be started only when an undetectable amount of the previous drug has been documented. If sequential therapy is given, then Pneumocystis jiroveci pneumonia prophylaxis is recommended especially in triple immunosuppressive treatment.
- The sequential therapy with calcineurin inhibitors must be given after the steroids are weaned out completely as concomitant administration of steroid may increase the risk of infection.
The updates in the guidelines are based on latest clinical trials and review of the literature. They have been provided with an aim to help practitioners at all levels, however they do stress that each patient is unique and therefore the recommendations should be used in conjunction with local practice patterns.
DoctorsM3 India account
-
Exclusive Write-ups& Webinars by KOLs
- Daily Quiz by specialty
Guidelines And Conflicts Of Interest
All members of the expert panel complied with the IDSA policy on conflicts of interest, which requires disclosure of any financial, intellectual, or other interest that might be construed as constituting an actual, potential, or apparent conflict. To provide thorough transparency, IDSA requires full disclosure of all relationships, regardless of relevancy to the guideline topic . Evaluation of such relationships as potential conflicts of interest is determined by a review process that includes assessment by the SPGC chair, the SPGC liaison to the development panel, and the BOD liaison to the SPGC, and, if necessary, the COI Task Force of the Board. This assessment of disclosed relationships for possible COI is based on the relative weight of the financial relationship and the relevance of the relationship . See Acknowledgments section for disclosures reported to IDSA.
Differences In Treatment Strategies Between Adult Uc And Pediatric Uc
While in adult-onset UC the choice of induction and maintenance treatment is determined by both disease extent and severity, in children disease activity dominates treatment strategies. Since limited disease is less common, disease extent is not a very useful parameter in managing childhood UC. Despite the generally accepted step-up approach in pediatric UC, more children will require rapid treatment escalation both for induction and maintenance of remission, due to a more severe disease presentation. Children with a refractory disease or those with frequent flares must be carefully evaluated for adherence to treatment using published strategies. Lastly, all children should be offered support programs that teach coping skills with this deliberating chronic disease. Although this is also true in adult medicine, the importance of such programs is higher in the vulnerable pediatric age group.
Recommended Reading: Colon Cancer Symptoms Vs Ulcerative Colitis
Pediatric Uc Epidemiology And Disease Features
Worldwide, the prevalence of UC is rising, and while the incidence is stabilizing in much of the Western world, rates are increasing in newly industrialized countries, specifically in parts of South Asia . To address the increasing disease burden, there is an urgent need to develop biomarkers that predict disease severity and disease course in a wide diverse population .
Features indicative of pediatric UC are well-described in the criteria set forth by the North American and European Societies for Pediatric Gastroenterology Hepatology and Nutrition . UC typically presents with a continuous inflammation of the rectum and colon proximally and is further categorized based on disease location and severity by the Paris pediatric modification of the Montreal classification of IBD . It is well-recognized that, in children, UC can present with atypical features, including macroscopic rectal sparing , backwash ileitis in association with severe pancolitis, and limited distal disease associated with mild cecal inflammation with an otherwise normal right colon . The presentation and natural history of pediatric UC are distinct from those of adult UC in that the majority of pediatric-onset UC presents with extensive colitis affecting the entire colon . On the contrary adults predominately present with left-sided colitis , with more than half in remission or with mild disease activity after initial presentation .
Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
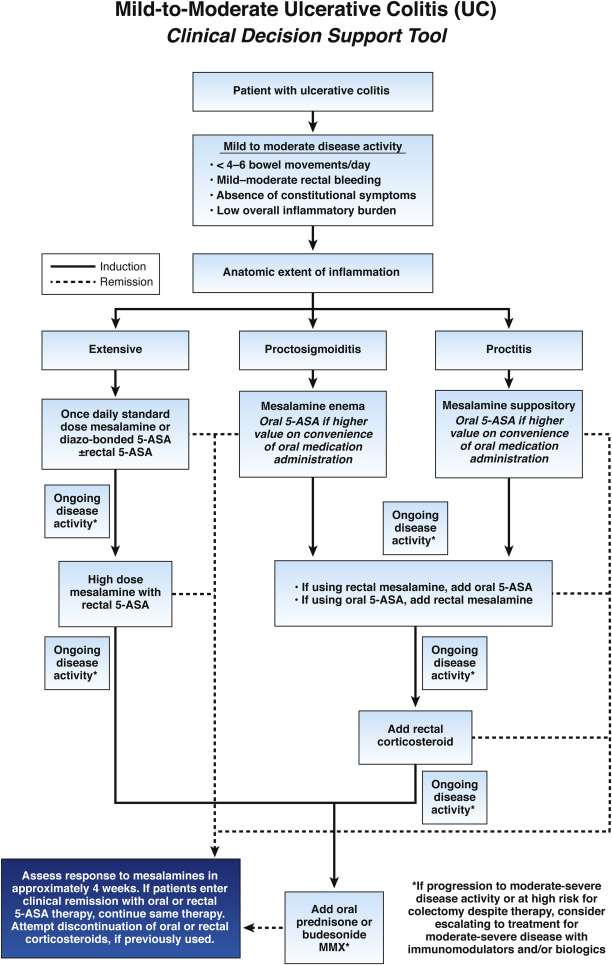
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
You May Like: What Is An Ulcer Diet
American Gastroenterological Association Guidelines
The AGA released new guidelines on the management of mild-to-moderate ulcerative colitis in February 2019, with a focus on the use of oral and topical 5-aminosalicylates agents, rectal corticosteroids, and PO budesonide.
Strong recommendations
Patients with extensive mild-moderate UC: The AGA recommends using either standard-dose mesalamine or diazo-bonded 5-ASA rather than low-dose mesalamine, sulfasalazine, or no treatment.
Patients with mild-moderate ulcerative proctitis who choose rectal therapy over oral therapy: The AGA recommends using mesalamine suppositories.
Conditional recommendations
Patients with extensive or left-sided mild-moderate UC: The AGA suggests adding rectal mesalamine to oral 5-ASA.
Patients with mild-moderate UC with a suboptimal response to standard-dose mesalamine or diazo-bonded 5-ASA or with moderate disease activity: The AGA suggests using high-dose mesalamine with rectal mesalamine.
Patients with mild-moderate UC being treated with oral mesalamine: The AGA suggests using once-daily dosing rather than multiple times per day dosing.
Patients with mild-moderate UC: The AGA suggests using standard-dose oral mesalamine or diazo-bonded 5-ASA, rather than budesonide MMX or controlled ileal release budesonide for induction of remission.
Patients with left-sided mild-moderate ulcerative proctosigmoiditis or proctitis: The AGA suggests using mesalamine enemas rather than oral mesalamine.
No recommendations
References
Infection Prevention And Control: Isolation Measures For Patients With Cdi
XIII. Should private rooms and/or dedicated toilet facilities be used for isolated patients with CDI?
XIV. Should gloves and gowns be worn while caring for isolated CDI patients?
XV. When should isolation be implemented?
XVI. How long should isolation be continued?
XVII. What is the recommended hand hygiene method when caring for patients in isolation for CDI?
XXI. Should cleaning adequacy be evaluated?
You May Like: Natural Supplements For Ulcerative Colitis
Rationale For Precision Medicine In Uc
Pediatric UC patients exhibit a wide variety of disease activity and heterogeneity in disease course. While pediatric UC patients often present with extensive colitis at first presentation, response to initial therapies, and disease course varies . Thus, it can be challenging to predict which patients will have progression of disease and require colectomy based on phenotypic description at presentation alone. Predictors that identify which treatments will be effective for which patients are critically needed so that patients can achieve rapid and sustained improvement in symptoms and quality of life , normalize growth and development , reduce cumulative exposure to corticosteroids and their associated toxicities, and avoid disease complications including toxic megacolon and colitis-associated colorectal cancer later in life . Moreover, we wish to consistently use the safest treatment approach that will achieve this goal for any individual patient.
Predicting And Monitoring Response To Medical Therapy
Traditionally, the treatment choice for pediatric UC is determined based on disease activity classified as mild, moderate, or severe . However, full implementation of personalized medicine in pediatric UC requires predictors or response to treatments with distinct mechanisms of actions to direct the right treatment to the right patient and predictors of drug pharmacokinetics as well as PK and pharmacodynamic targets to optimize a specific therapy and ensure its sustained effect. Factors associated with response to medical or surgical therapy, discussed in more detail below, are listed in Table 1.
Table 1. Factors associated with response to therapy in pediatric UC.
Read Also: Surgical Management Of Ulcerative Colitis Ppt
Response To Other Biologic And Small
Vedolizumab , an 47 anti-integrin inhibitor, is from a second biologic class that was approved for the use of adult IBD in 2014. The first pediatric retrospective study of VDZ identified that 76% of UC patients were in remission at week 14. In a subanalysis at week 22 that included both patients with UC and CD, anti-TNF-naïve patients were more likely to be in remission than anti-TNF-exposed patients . Another retrospective pediatric study demonstrated that 59% of anti-TNF-naïve patients with UC achieved endoscopic remission, compared to 15% of anti-TNF-exposed patients. However, the authors noted that anti-TNF-naïve patients had lower partial Mayo baseline scores compared with exposed patients . The anti-TNF exposure findings were similar to the original adult GEMINI study in which anti-TNF-naïve patients had faster symptom improvement , and a subsequent network meta-analysis confirmed that more anti-TNF-naïve patients achieved remission compared with anti-TNF-exposed patients .
Even fewer pediatric-specific predictors of response are known for anti-TNF therapy beyond IFX and adalimumab such as golimumab or other biologic classes not yet approved for pediatric UC beyond anti-TNF and VDZ or biosimilars or novel small molecules such as Janus kinase inhibitors.
Complications After Colectomy And Ileal Pouch Anal Anastomosis
Within 5 years of diagnosis, 1215% of children with UC will have disease refractory to medical therapy and require total colectomy and IPAA . In this staged surgical procedure, the diseased colon and rectum are removed, and a pouch reservoir is constructed from the distal ileum and anastomosed to a short rectal cuff to preserve continuity and avoid a permanent ileostomy. Although outcomes after colectomy and IPAA in pediatric patients are generally quite good, inflammatory complications such as acute pouchitis , chronic pouchitis , and de novo CD of the pouch can occur . Rates of overall pouch failure are fortunately quite low at ~8% .
Attempts at identifying predictors of chronic pouchitis or de novo CD in children with IPAA have generally been limited by mostly retrospective single-center designs with relatively small sample sizes. Several factors either directly related or likely related to preoperative disease severity including PUCAI score, preoperative cumulative corticosteroid use, and preoperative peripheral blood neutrophil percentage have been associated with higher risk for development of chronic pouchitis in children .
Read Also: Ulcerative Colitis Is It Deadly
Predicting Outcomes In Pediatric Ulcerative Colitis For Management Optimization: Systematic Review And Consensus Statements From The Pediatric Inflammatory Bowel Diseaseahead Program
- AffiliationsUniversity Medical Center Rostock, Department of Pediatrics, Rostock, GermanyQueen Mary University of London, The Barts and the London School of Medicine and Dentistry, Blizard Institute, Center for Immunobiology, London, United Kingdom
- Séamus HusseyAffiliationsNational Childrens Research Centre, Royal College of Surgeons of Ireland and University College Dublin, Dublin, Ireland
- Frank M. RuemmeleAffiliationsUniversité Paris Descartes, Sorbonne Paris Cité Assistance Publique-Hôpitaux de Paris, Hôpital Necker-Enfants Malades, Service de Gastroentérologie Pédiatrique Institute IMAGINE Inserm U1163, Paris, France
- David C. WilsonAffiliationsChild Life and Health, University of Edinburgh, Paediatric Gastroenterology and Nutrition, Royal Hospital for Sick Children, Edinburgh, Scotland, United Kingdom
- Dan TurnerCorrespondenceCorrespondence Address correspondence to: Dan Turner, MD, PhD, The Juliet Keidan Institute of Pediatric Gastroenterology and Nutrition, Shaare Zedek Medical Center, The Hebrew University POB 3235, Jerusalem 91031, Israel fax: +972-2-6555756.
- Authors share co-first authorship.
Probiotics As Potential Treatment
Probiotics are defined as live microbial food products that have beneficial effects on the host. Probiotics have been suggested as potential treatments for numerous digestive disorders whether they are effective treatments remains controversial, however.
In an investigation of a specific probiotic preparation, subjects in the treatment group achieved a 93% remission rate versus 36% in the control group, with a lower relapse rate at 1 year seen in the treatment group as well .
Probiotics may represent an appealing adjunct to other treatments, given their low propensity for side effects.
Probiotics may have a more important role with pouchitis in patients with ulcerative colitis.
References
Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011 Jun. 17 :1314-21. .
Siow VS, Bhatt R, Mollen KP. Management of acute severe ulcerative colitis in children. Semin Pediatr Surg. 2017 Dec. 26 :367-72. .
Rinawi F, Assa A, Eliakim R, et al. Risk of colectomy in patients with pediatric-onset ulcerative colitis. J Pediatr Gastroenterol Nutr. 2017 Oct. 65 :410-5. .
Koike Y, Uchida K, Inoue M, et al. Early first episode of pouchitis after ileal pouch-anal anastomosis for pediatric ulcerative colitis is a risk factor for development of chronic pouchitis. J Pediatr Surg. 2018 Oct 30. .
Also Check: Do You Still Have Ulcerative Colitis After Colectomy
Clinical Practice Guidelines For Clostridium Difficile Infection In Adults And Children: 2017 Update By The Infectious Diseases Society Of America And Society For Healthcare Epidemiology Of America
Clinical Infectious Diseases, Volume 66, Issue 7, 1 April 2018, Pages e1e48, : 15 February 2018
L Clifford McDonald, Dale N Gerding, Stuart Johnson, Johan S Bakken, Karen C Carroll, Susan E Coffin, Erik R Dubberke, Kevin W Garey, Carolyn V Gould, Ciaran Kelly, Vivian Loo, Julia Shaklee Sammons, Thomas J Sandora, Mark H Wilcox
For full document, including tables and references, please visit the Oxford University Press website.
To view the 2021 focused update, please visit the Oxford University Press website.
New Guidelines For Treating Patients With Ulcerative Colitis
David Rubin, MD
New guidelines on diagnosing and managing ulcerative colitis are aimed at helping patients experience sustained periods of remission from the debilitating inflammatory disease while relying less on traditionally used steroids.
These novel recommendations will help doctors better prevent and care for patients with ulcerative colitis by shifting us from managing flare-ups to better monitoring and preventing them in the first place, said gastroenterologist David Rubin, MD, chief of gastroenterology, hepatology, and nutrition and co-director of the Digestive Diseases Center at the University of Chicago Medicine.
Rubin led the team of experts that established the guidelines, published in the March issue of The American Journal of Gastroenterology.
Ulcerative colitis , a chronic disease affecting roughly 1 million Americans, is characterized by periods of inflammation and ulcers in the lining of the large intestine. Symptoms include bloody stool, diarrhea, abdominal pain and urgency to go to the bathroom, as well as joint pain.
Rubin says the new management guidelines are geared towards relieving symptoms, preventing harmful secondary effects that may be brought on by treatment, and helping patients into remission. The guidelines place added importance on reducing inflammation and ulcers in the innermost lining of the colon and rectum, which physicians refer to as mucosal healing.
You May Like: How Can I Get Rid Of Mouth Ulcers
New Aga Guideline: Management Of Ulcerative Colitis
Check out the new AGA clinical guideline in Gastroenterology with recommendations for the management of adult outpatients with moderate to severe ulcerative colitis as well as adult hospitalized patients with acute severe UC. The guideline focuses on immunomodulators, biologics and small molecules to bring on and maintain remission for patients with moderate to severe UC and to decrease the risk of colectomy.
Here are five of the most noteworthy recommendations. For all 15 recommendations, review the full guideline.
New Guideline Provides Recommendations For The Treatment Of Mild
Bethesda, MD Most patients with ulcerative colitis have mild-to-moderate disease characterized by periods of activity or remission, but practice variations exist in disease management. A new clinical guideline from the American Gastroenterological Association published in Gastroenterology, the official journal of AGA, addresses the medical management of these patients, focusing on use of both oral and topical 5-aminosalicylates medications, rectal corticosteroids and oral budesonide, to promote high-quality care for UC patients.
AGAs new clinical guideline is meant to help with the management of patients with mild-to-moderate UC, but not all patients will effectively respond to the outlined therapies. In those cases, there may be a need to escalate treatment to systemic corticosteroids, immunomodulators and/or biologic therapies for induction and maintenance of remission. However, the use of biologic therapies and/or immunomodulators are not specifically addressed within the guideline.
The guideline recommends the following for the medical management of mild-to-moderate ulcerative colitis: 1. Use either standard dose mesalamine or diazo-bonded 5-ASA rather than low dose mesalamine, sulfasalazine or no treatment in patients with extensive mild-moderate UC.
2. In patients with extensive or left-sided mild-moderate UC, add rectal mesalamine to oral 5-ASA.
11. In patients with mildmoderate UC , AGA makes no recommendation for use of probiotics.
You May Like: Ulcerative Colitis Abdominal Pain Relief