Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
How Do You Do A Bowel Rest At Home
Start with clear liquids and then progress to full liquids, such as gelato or ice cream, if you can tolerate milk products. Add soft, mushy foods such as porridge, scrambled eggs, and overcooked pasta. If you can tolerate these, you can add chopped meats like chicken and ultimately cooked vegetables, too.
Hydrogen Sulphide: Bad Malodorous Gas Responsible For Relapses In Uc
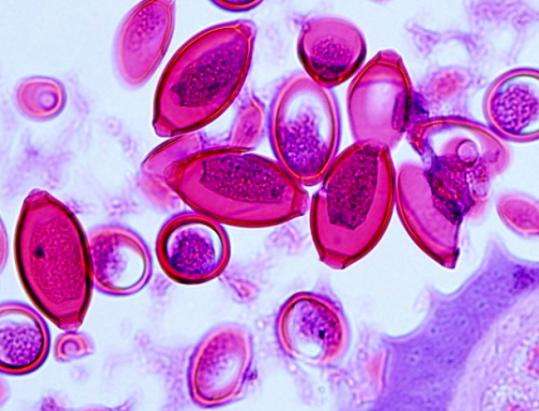
Mercaptides such as sodium hydrogen sulphide are reducing agents that help maintain anaerobic conditions in the colonic lumen. They are produced in the human large intestine by bacterial reduction of dietary inorganic sulphate and sulphite and by fermentation of sulphur amino acids. The acute toxicity of hydrogen sulphide appears to result from inhibition of cytochrome oxidase leading to mucosal damage, loss of barrier function, and histological changes resembling UC. Hence the colonic mucosa has developed a very effective means of detoxifying hydrogen sulphide.
Mainly exogenous sources contribute to the colonic pool of sulphur, such as red meat, cheese, milk, fish, nuts, and eggs, and as preservatives found in commercial breads, beers, many alcoholic drinks, sausages, and dried fruits. Faecal sulphide levels increase after consumption of increasing amounts of meat, providing evidence that meat is an important substrate for sulphide generation by bacteria in the human large intestine.
Recommended Reading: How Long Does A Ulcerative Colitis Flare Up Last
How To Eat During An Ibd Flare
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
People with inflammatory bowel disease often face an uphill battle when it comes to diet, especially when the disease is active. Many people with IBD don’t know what food to eat when the Crohn’s disease or ulcerative colitis is flaring. Everyone with IBD is different, and one person’s flare-up diet isn’t going to work for another, but there are some broad ideas that may work for many.
-
Milk, cheese, ice cream, and yogurt
-
Brown rice, popcorn, oats, and barley
-
Fried food
-
Raw veggies
Are Bananas Good For Colitis
Bananas are high on the list of healthy foods if youre in an ulcerative colitis flare. Theyre easy to digest and rich in potassium . People with irritable bowel disorders, like ulcerative colitis, are often deficient in this mineral. Blend one cup of low fat milk with one cup of yogurt, a ripe banana, and ice.
Recommended Reading: Dog Skin Ulcer Home Treatment
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
Treatment Of Ulcerative Colitis And Food
The treatment of ulcerative colitis involves controlling symptoms and preventing flare-ups, and your diet plays an important role in it. Research has shown that certain foods can provide symptomatic relief whereas others can make the symptoms worse. To help you keep your symptoms of ulcerative colitis under control, here we are listing the most important foods that you should eat and avoid along with some general dietary guidelines.
Recommended Reading: How Do You Check For A Stomach Ulcer
Which Nutrients Are Important In Crohn’s And Colitis
Vitamins and mineralsYour body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
IronHaving low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
- feeling tired and lacking in energy
- feeling short of breath
- fast or irregular heartbeat
- pale skin.
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
- wind
- stomach rumbling and pain
- diarrhoea loose and runny stools.
- sipping a cold drink
Foods To Eat With Colitis Flare Up
Since ulcerative colitis cause diarrhea, most experts recommend you to limit your fiber intake when you have colitis flare. However, it is good to replace high fiber foods such as nuts, seeds, raw fruits, and vegetables with more easily digestible diet.
Here are some foods to eat with colitis and the reasons how they can help.
1. Cooked Vegetables
For many people with ulcerative colitis, cooked veggies such as carrot and spinach can be a great source for getting important nutrients like Vitamins A and K.During a colitis flare-up, ensure that the carrots are cooked until they are soft and tender. Cooked carrots are not just easy to digest, but also contain antioxidants that may help ease ulcerative colitis symptoms.
2. Yogurt
Live and active culture yogurt can be a good source of protein if you have colitis flare. The probiotics in this form of yogurt have good bacteria that help ease gastrointestinal problems. Also, moderate amounts of dairy products will not lead to diarrhea but if milk causes bloating or stomach discomfort, turn to lactose-free milk.
3. Salmon
Salmon is good for colon which is rich in omega 3 fatty acids, have health benefits beyond the digestive tract and reduce inflammation. By adding salmon to the foods they eat, people with ulcerative colitis get more protein to their diet and ease symptoms of colitis flare-ups.
Try baking or grilling fish, as frying fish lose a lot of its nutritional value.
4. Applesauce
5. Soft bland foods
6. Oatmeal
7. Eggs
You May Like: How Does Ulcerative Colitis Affect The Body
Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this “good” fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didn’t like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs — a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods — may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
What You Should Do On A Regular Basis:
- Eat small, frequent meals.
- Consume a high calorie, high protein diet.
- Drink plenty of fluids, especially water.
- Eat a high fiber diet, including:
- 4 servings/day of whole grain breads and cereals
- 5 servings/day of fruits and vegetables
Don’t Miss: How Do You Get A Peptic Ulcer
Effect Of Alcoholic Intoxication On The Risk Of Inflammatory Bowel Disease: A Nationwide Retrospective Cohort Study
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
-
Affiliations School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan, Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
-
Affiliations Department of Emergency Medicine, Chang Gung Memorial Hospital, Chiayi, Taiwan, Department of Nursing, Chang Gung University of Science and Technology, Chiayi, Taiwan
-
Affiliations Graduate Institute of Clinical Medicine, National Taiwan University College of Medicine, Taipei, Taiwan, Department of Dermatology, National Taiwan University Hospital Yunlin Branch, Douliou, Taiwan
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
Dont Miss: What To Eat When You Have Gastric Ulcer
Ulcerative Colitis Diet: Foods To Eat And Foods To Avoid
- Keeping a food journal can help you identify foods that trigger ulcerative colitis symptoms.
- Avoiding common trigger foods may help manage symptoms during UC flares.
- Knowing which foods are most nutritious for those with UC and how to safely prepare them can help you eat healthier.
- Working with a registered dietitian can help you get the most nutrients out of the foods you can safely eat.
Ulcerative colitis is an autoimmune condition caused when the immune system attacks the tissues of the digestive tract, specifically the large intestine and rectum. Along with Crohns disease, ulcerative colitis is a type of inflammatory bowel disease. IBD inflammation leads to gastrointestinal symptoms, such as diarrhea, bloating, and cramping, as well as problems with digestion and absorption of nutrients.
No specific foods cause ulcerative colitis, and there is no specific diet that has been proven to cure it. However, each person with UC finds that certain foods can trigger or worsen symptoms, while other foods can be digested safely and comfortably. The foods on each list vary by individual. As one MyCrohnsAndColitisTeam member put it, This disease is not one-size-fits-all, so you will have to experiment to see what works for you and what does not.
The list of foods to avoid and foods to eat with ulcerative colitis may also change depending on whether youre currently experiencing a disease flare or remission .
Recommended Reading: Causes Of Bleeding Ulcers In Stomach
My Experience Of Drinking Alcohol With Ulcerative Colitis
Given that I suffer from migraines as well as IBD, alcohol always makes things worse for me. I stopped drinking any kind of alcohol when I was about 24. When I was younger, on the nights I would drink with my friends, I stuck to clear liquids . I found them to affect my ostomy and intestines the least.
The heavy, regular beer never sat well with me. Basically, I kind of went by the rule the less alcohol in my system that will get me where I want to be, the better which is why I was never someone who sipped on cocktails and really enjoyed the flavor. Thinking back, I probably would have had better luck if I did the latter but, we all live and learn.
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Tom
Don’t Miss: Besivance Dosage For Corneal Ulcer
Nutritious Foods To Combat Ulcerative Colitis Complications
People with ulcerative colitis commonly experience anemia and unintended weight loss. Anemia is a low red blood cell count caused by chronic blood loss. It can cause fatigue unless treated. For this reason, the nutrients folate, magnesium, calcium, and iron are of special importance for individuals with UC.
Furthermore, steroid medications such as prednisone may contribute to risk of osteoporosis, which puts emphasis on dietary intake of calcium, vitamin D, magnesium, and vitamin K. Here are the vital body functions that depend on each of these nutrients, along with food sources rich in each.
Calcium
Calcium is important for healthy bones, teeth, and the heart. The best food sources include dairy products, such as yogurt, milk, cottage cheese, and more. Nondairy sources of calcium include sardines , fortified soy milk and almond milk, tofu, kale, broccoli, and chia seeds.
Folate
Folate is crucial for cell division and DNA synthesis. It is found in avocados, black-eyed peas, spinach, Brussels sprouts, asparagus, and fortified breakfast cereals.
Iron
Iron is an important mineral that helps transport oxygen in red blood cells from the lungs to body tissues. It is found in fortified breakfast cereals, tofu, spinach, lentils, chickpeas, and cashews.
Magnesium
Magnesium is an important electrolyte that may be lost through sweating or diarrhea. Foods such as halibut, nuts, nut butters, spinach, potatoes with skin, black-eyed peas, and spinach are rich in magnesium.
Vitamin D
Is Black Pepper Bad For Ulcerative Colitis
Refined sugar can pull more water into the gut and cause diarrhea. Spicy foods, hot sauces, and pepper can cause diarrhea in many people, and in someone with ulcerative colitis experiencing a flare spicy hot foods may trigger or worsen symptoms.
What spices to avoid with ulcerative colitis? Spices that may worsen IBD symptoms:. Pepper.. Cloves.. Curry.. Chili powder.. Garlic.. Mustard.. Nutmeg.. Horseradish.
Is turmeric and black pepper good for ulcerative colitis? The Indian spice, long prized for its medicinal and anti-inflammatory properties, may hold promise for people with ulcerative colitis. Besides being a staple of Asian cuisine, turmeric has been used for centuries in Ayurvedic and traditional Chinese medicine to help treat a wide range of inflammatory diseases.
What foods heal ulcerative colitis? The following foods may be suitable for a person who has just had a flare-up of Crohns disease or ulcerative colitis:. diluted juices.. applesauce.. canned fruit.. oatmeal.. plain chicken, turkey, or fish.. cooked eggs or egg substitutes.. mashed potatoes, white rice, or noodles.. sourdough or white bread.
Don’t Miss: How To Treat An Ulcer In Your Esophagus
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.