What Is A Stage 2 Pressure Ulcer
Bedsores, or pressure ulcers, are complex medical conditions that can lead to serious complications. Without appropriate intervention and treatment, pressure ulcers progress through a number of stages that become harder to treat. When an improperly treated stage 1 bedsore becomes more serious, it may develop into a stage 2 bedsore. Knowing the signs, symptoms, and treatment options for this classification of ulcer can help caregivers and loved ones intervene before the condition becomes more serious. If you or somebody you love has developed a stage 2 bedsore due to negligence, consider speaking with a compassionate West Virginia nursing home abuse lawyer. You may be entitled to compensation for your injuries.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Recommended Reading: Can I Donate Blood If I Have Ulcerative Colitis
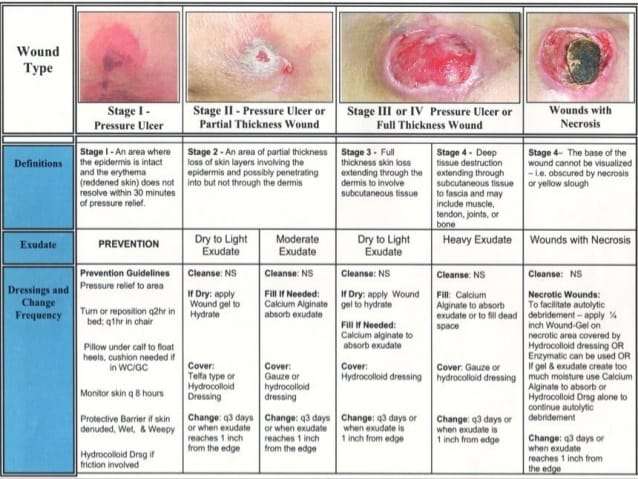
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Recommended Reading: How Do You Know If You Have Ulcerative Colitis
Stage 2 Bedsore Treatment
The Model Systems Knowledge Translation Center encourages people with stage 2 bedsores to see a health care provider as soon as possible.
Treatment for stage 2 bedsore typically involves:
- Bandaging: Bandages help keep bedsores dry and reduce the risk of infection.
- Cleaning: Doctors may use a saltwater solution called saline to clean the open wound when bandages are changed.
- Debriding: The Mayo Clinic notes that damaged and dead tissue must be removed so the bedsore can heal properly. This process is known as debridement.
- Getting Good Nutrition: The MSKTC recommends a diet rich in vitamin A and C, protein, zinc, and iron as part of a stage 2 bedsore treatment plan. Drinking enough water is also important. Johns Hopkins Medicine found that bedsores wont properly heal without these dietary changes.
- Reducing Pressure: Taking pressure off the bedsore will prevent it from getting worse and allow the skin to start repairing itself.
Seek medical advice from trusted doctors or nurses to learn more about treating pressure sores.
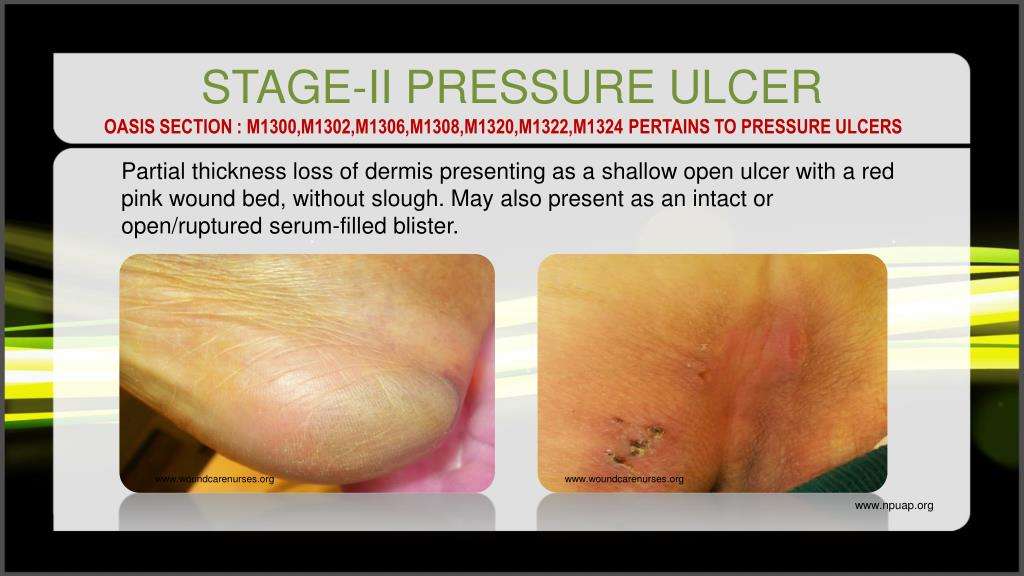
Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are shallow with a reddish base. Adipose and deeper tissues are not visible, granulation tissue, slough and eschar are not present. Intact or partially ruptured blisters that are a result of pressure can also be considered stage 2 pressure ulcers. Note that causes of erosion, ulceration, or blistering that aren’t a result of pressure are not included in the definition of a stage 2 ulcer.
Also Check: Support Surfaces For Pressure Ulcer Prevention
The Four Stages Of Pressure Injuries
We know pressure injuries are dangerous for our patients and costly for our medical system, so the question becomes, how can we recognize them in order to guard against them? Pressure injuries are broken into four stages, where the stage indicates the extent of tissue damage. Following are the key indicators for each stage.
Use Liquid Collagen Protein To Heal Faster
Protein is a vital nutrient in healing from any injury, and pressure ulcers are no exception. There are two big reasons one should consider protein supplementation during pressure ulcer treatment: One, patients with chronic pressure ulcers lose some of their protein stores through open wounds and body fluids. Two, protein is the building block for restoring healthy skin and plays a big role in the speed of recovery.
One should focus on consuming high-quality protein from their diet from sources such as chicken, fish, beef, beans, nuts, tofu, or other complete protein sources. The recommended daily protein intake is about 0.8 grams per kilogram of body weight but may be increased for someone who is already deficient or recovering from an injury.
On top of this, supplementation with a fortified, hydrolyzed collagen supplement may be beneficial. Collagen is a complex structural protein that makes up a large portion of our skin, tendons, and other connective tissues. Because it is not found in most meat products the best way to get collagen is through a supplement.
In a study published in Advances in Skin & Wound Care: The Journal for Prevention and Healing, researches spent 8 weeks studying the impact of hydrolyzed collagen supplementation on patients recovering from pressure ulcers.
They found that after 8 weeks of standard care + collagen supplementation, patients healed twice as quickly as those receiving standard care + placebo.
You May Like: What Causes Acute Ulcerative Colitis
Overall Completeness And Applicability Of Evidence
The network is sparse, in terms of the total number of participants, the total number of wounds healed, the number of studies per contrast, the size of the constituent studies and the duration of followup: 21 of 27 direct contrasts were informed by only one study and the average number of events per mixed treatment contrast was around four. The median study size was 41 and several studies had zero events. The duration of followup was relatively short for most studies : only 3/39 studies in the network had a followup duration of 16 weeks or more.
In parallel we conducted a second NMA, grouping together some classes of dressings. We had hoped that the group network would provide more power in the analysis, but in practice too many data were excluded from the network, and the network was also unbalanced, being dominated by the advanced dressing versus basic dressing contrast, which involved about 55% of the participants in the group network. The group network provided equally uncertain evidence and the findings are not discussed further here, but are reported in for the interested reader.
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
-
the proportion of wounds healed
-
time to complete healing .
Don’t Miss: Medications For Ulcers Over The Counter
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Don’t Miss: Foods That Irritate Stomach Ulcers
What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
Don’t Miss: Diabetic Foot Ulcer Treatment Guidelines
Pressure Ulcer Treatment: Understanding Your Options
Pressure ulcers, commonly known as bedsores or pressure injuries, are caused by constant friction and pressure on particular parts of the body, causing damage in the underlying tissue, coupled with inflammation and even infection.
They are most often associated with people in wheelchairs or those that spend prolonged amounts of time lying down. They can also be quite painful and are difficult to treat. In this post, we will discuss the best evidence-based treatment strategies and products that support optimum healing and skin repair.
Background And Objectives For The Systematic Review
Uninterrupted pressure exerted on the skin, soft tissue, muscle, and bone can lead to the development of localized ischemia, tissue inflammation, tissue anoxia, and necrosis. Pressure ulcers can result from these effects about 3 million adults in the United States suffer from pressure ulcers. Estimates of the incidence of pressure ulcers vary according to the setting and range from 0.4 to 38.0 percent in acute-care hospitals, from 2.2 to 23.9 percent in long-term nursing facilities, and from 0 to 17 percent in the home-care setting.1,2 Various systems have been used to assess the severity of pressure ulcers, but most use a four-stage categorization with higher numbers indicating higher severity.3 Healing rates of pressure ulcers vary considerably and are dependent on comorbidities, clinical interventions, and severity of the ulcer. This variability can add to the length of hospitalization and impede the return of patients to full functioning.2 Data on the costs of treatment for a pressure ulcer vary, but some estimates range between $37,800 and $70,000, with total annual costs in the United States as high as $11 billion.1,4
Recommended Reading: Foam Dressing For Pressure Ulcer
F Grading The Evidence For Each Key Question
The strength of evidence for each KQ will be assessed by one researcher for each applicable outcome by using the approach described by Owens et al.10 To ensure consistency and validity of the evaluation, the grades of each reviewer will be reviewed by the entire team of investigators to evaluate:
- Risk of bias
- Consistency
- Directness
- Precision
We will also estimate publication bias by examining whether studies with smaller sample sizes tended to have positive or negative assessments of pressure ulcer treatment.
The strength of evidence will be assigned an overall grade of high, moderate, low, or insufficient according to a four-level scale:
- HighâHigh confidence that the evidence reflects the true effect. Further research is very unlikely to change our confidence in the estimate of effect.
- ModerateâModerate confidence that the evidence reflects the true effect. Further research may change our confidence in the estimate of effect and may change the estimate.
- LowâLow confidence that the evidence reflects the true effect. Further research is likely to change the confidence in the estimate of effect and is likely to change the estimate.
- InsufficientâEvidence either is unavailable or does not permit estimation of an effect.
D Assessment Of Methodological Quality Of Individual Studies
Predefined criteria will be used to assess the quality of individual controlled trials, systematic reviews, and observational studies. Each study evaluated will be reviewed dually by 2 individuals, a principal investigator and a research staff member, who will use a clearly defined template and criterion to assess methodological quality. Randomized trials and cohort studies will be evaluated by using appropriate criteria and methods developed by the USPSTF.9These will be used in conjunction with the approach recommended in the chapter âAssessing the Risk of Bias of Individual Studies When Comparing Medical Interventionsâ in the AHRQ Methods Guide for Effectiveness and Comparative Effectiveness Reviews.8
Individual studies will be rated as âgood,â âfair,â or âpoor.â Studies rated âgoodâ will be considered to have the least risk of bias, and their results will be considered valid. Good-quality studies include clear descriptions of the population, setting, interventions, and comparison groups a valid method for allocating patients to treatment low dropout rates and clear reporting of dropouts appropriate means for preventing bias and appropriate measurement of outcomes.
Don’t Miss: Foam Dressings For Pressure Ulcer Prevention