Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
Read Also: Best Ulcerative Colitis Diet Book
Talk To Your Doctor Asap
Heres the thingUC treatment for mild disease is typically oral medication and for moderate to severe disease, often biologics. But medications can stop working for many reasons, says Andrew Boxer, M.D., a gastroenterologist at Jersey City Medical Center RWJBarnabas Health Medical Group, Jersey City, NJ. Or you might have an infection. Both scenarios can cause a UC flare. So its key that you tell your doctor as soon as you experience symptoms, he says. If a flare is caught early, treatment may help stop the flare, Dr. Boxer explains.
Recommended Reading: Foam Boots For Pressure Ulcers
Mental And Emotional Health With Flare
Going through a UC flare is also emotionally draining. You mentioned feeling depressed, anxious, and generally down. During a flare, your quality of life takes a sharp downturn, which impacts mental health.
“Hopeless, anxious, dreary.”
“Depressing, painful, hopeless.”
If these symptoms persist beyond flares, have a conversation with your doctor. Those living with chronic illness often endure more days of depression and anxiety than the general public. Talk therapy and prescription drugs can address depression and anxiety tied to UC.2
Don’t Miss: Can I Eat Oatmeal With Ulcerative Colitis
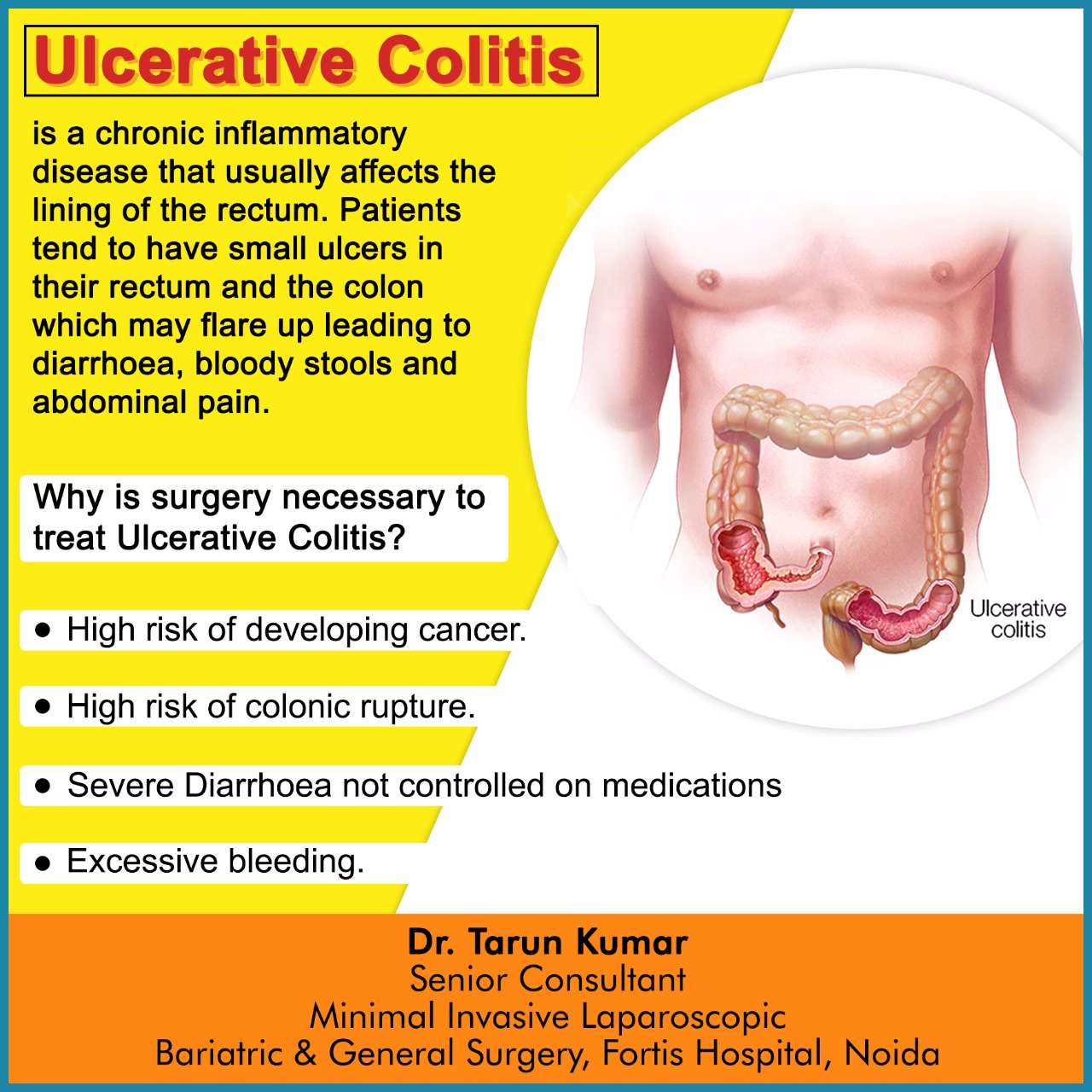
Surgery For Managing Uc Flare
Surgery may be used to manage the symptoms of ulcerative colitis when other treatments are unable to get the disease under control . While surgery can often eliminate UC entirely, it usually requires removing the entire colon and rectum in a procedure called a total proctocolectomy. Some people with UC later have another procedure to create a J-pouch .
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Don’t Miss: Indian Diet For Ulcerative Colitis
Skipping Or Forgetting To Take Your Uc Medication
UC causes inflammation and ulcers in the colon. If left untreated, this condition can lead to life threatening complications, such as:
- bowel perforation
- colorectal cancer
- toxic megacolon
Your doctor will likely prescribe a medication to reduce inflammation, such as an anti-inflammatory drug or an immunosuppressant drug.
These medications help ease symptoms of UC and can also function as maintenance therapy to keep you in remission. Symptoms could return if you dont take your medication as directed.
At some point, your doctor may discuss slowly tapering off the medication. However, you should never decrease your dosage or stop taking your medication without speaking with your doctor first.
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
Don’t Miss: Herbal Medicine For Stomach Ulcer
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
- Monosaccharides
- Polyols
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Also Check: How To Cure Gastritis And Ulcers Naturally
Recommended Reading: How To Heal Leg Ulcers Quickly
Different Therapies Can Also Aid In Easing The Flare
Different therapies can also aid in easing the flare-up in ulcerative colitis. The frequency and intensity of lesion pain and symptoms are often lessened by use of complementary and different therapies, additionally to standard medical aid. These different therapies include yoga treatment, massage and psychotherapy. However, you must consult your doctor before taking any different medical aid, so as to avoid complications and to understand the merits and demerits.
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
Don’t Miss: Best Wound Care For Stage 2 Pressure Ulcer
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Talk With Onewelbeck Today

No one should have to think of flare-ups as something that become part of daily life. The team at OneWelbeck Digestive Health work with patients looking to get treatments for a number of gastrointestinal conditions.
You can see the main conditions we help with here, but if you want to speak with someone about ulcerative colitis, we are here to help. Please get in touch by leaving a message on our contact page, or by calling us directly on .
Recommended Reading: Why Are Bedridden Patients At Risk For Developing Decubitus Ulcers
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Recommended Reading: Foam Dressings For Leg Ulcers
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Eating Healthy Diet Will Surely Ease Flare
Eating healthy diet will absolutely ease flare-up of ulcerative colitis. Always confirm your diet is healthy and avoid consumption processed foods. Also, you must avoid sweet and spicy foods in your diet, as they cause irritation to your colon. Your diet ought to be composed of vegetables as a serious supply of super molecule. The vegetables ought to be recent and leafed inexperienced, as they are a decent supply of naphthoquinone. Naphthoquinone deficiency is associated to redness being severe. Additionally, avoid consumption beef however instead supply super molecule from chicken and turkey or baked fish. Beef causes stress in your colon.
Read Also: Best Way To Prevent Pressure Ulcers
Identify Daily Stressors And Put Your Health First
The second tip to help you prevent an ulcerative colitis flare-up is to ensure that you learn how to identify daily stressors so that you may eliminate them. Stressors for many people come up on a daily basis, whether it be work based, family based, or even relationship/friends based. I think that always keeping in mind that your health comes first no matter what. In other words, no issue is as important as your own health. By always keeping this in mind I find that it helps me mentally to filter things that brings stress instead of peace.
Warning Signs Of A Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission.
Symptoms of a flare may be different depending on the severity and location of the inflammation in the colon and rectum. Nevertheless, common symptoms include:
- Abdominal pain or cramps
- Fever
Recommended Reading: How To Prevent Pressure Ulcers In The Hospital
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
Also Check: How To Cure Tongue Ulcer
How Long Does An Ulcerative Colitis Flare
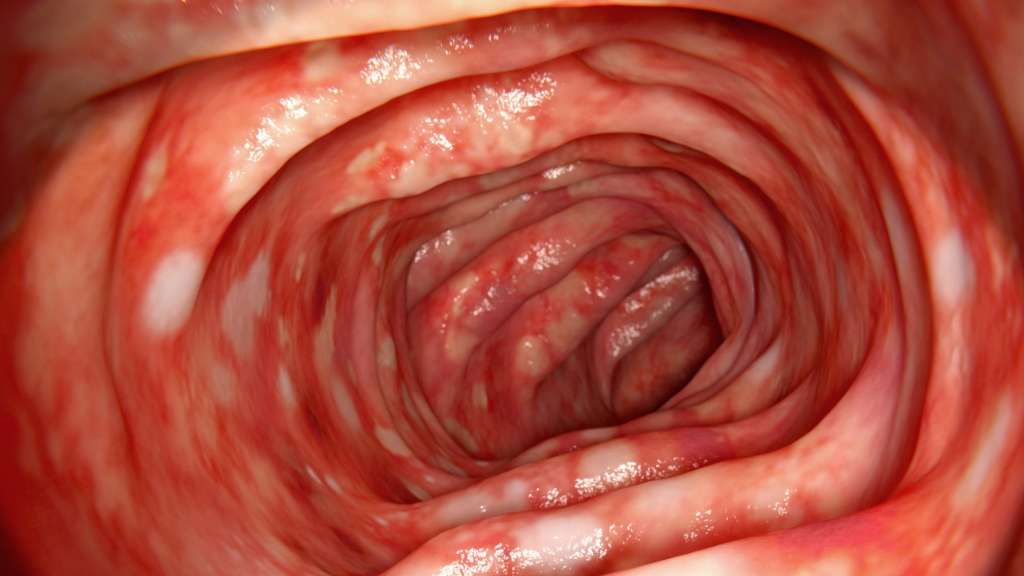
Ulcerative colitis is a chronic disease that causes inflammation and ulcers in the inner lining of the large intestine and rectum. If you have UC, you may experience repeated cycles of flare-ups and remissions .
A flare-up can last a few days or a few weeks and then be followed by a remission that lasts for months or even years. How long a flare-up lasts depends on factors such as:
While there is no cure for UC, several treatment options and lifestyle modifications can help reduce symptoms or prevent flare-ups.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Don’t Miss: How To Treat An Ulcer After Gastric Bypass
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
What Are The Causes Of Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The following have been suggested:
- Immune system
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body’s immune system malfunctions and attacks the tissues of the bowel.
Ulcerative colitis may occur at any age, but it is most common in young adults in the 15-30 age group or later on, in the 50-70 age group. Women are affected more than men.
You May Like: Foods To Eat During Ulcerative Colitis Flare Up
I Remembered What It Was To Have A Life Again
Mary Elizabeth Ulliman, 33, was diagnosed with ulcerative colitis in 2011 and says she was fatigued and made constant trips to the bathroom. But in 2015, Ulliman started taking two new medications that greatly improved her symptoms.
After a few months, I started noticing differences, she tells SELF. By 2016 my quality of life had done a complete 180 from where I’d been since 2011, she says. In the thick of my ulcerative colitis journey, I genuinely forgot how much fun life could be. I was slogging through, day after day, thinking that feeling miserable was how it was going to be forever, willing myself to make it through work days so I wouldn’t lose my job and insurance.
Remission, she says, allowed her to live fully again. Suddenly, life wasn’t made up of sleeping, bathroom trips, forcing myself to eat, and willing myself to not fall asleep at my desk at work, she says. I had some extra energy. I startedhesitant, at firstto exercise. I could eat food without immediately regretting it afterward. I could have a glass of wine now and again. I had the wherewithal to do activities after workcoaching, going to a happy hour, taking my dog to play. I remembered what it was to have a life again.
Ulliman wants other ulcerative colitis patients to have hope. When you’re in the black hole that is trying to find somethinganything that will work to control your it can be easy to forget how much fun and joy life can bring you, she says. Mary Elizabeth Ulliman
Related: