Causes Of Venous Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesn’t fall as you’re walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood can’t flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
Can Venous Leg Ulcers Be Prevented
There are several ways to help prevent developing a venous leg ulcer in people at risk.
These include:
- elevating your leg when possible
- stopping smoking if you smoke
These measures are particularly important if you previously had a leg ulcer.
This is because you’re at increased risk of having another one in the same leg within months or years.
Will I Need Any Tests
Testing lets your healthcare provider know how severe the ulcer is. You may also undergo regular testing to determine whether venous ulcer treatments are working.
Tests for venous ulcers include:
- Ankle-brachial index, which takes blood pressure readings of your arms and legs.
- Doppler study to listen to blood flowing through your veins.
- Imaging studies, such as a CT scan to identify damaged or nonfunctioning valves.
Don’t Miss: Signs You May Have Stomach Ulcers
Venous Leg Ulcers And Infection
The venous leg ulcer is the most common type of chronic leg wound, and it can be challenging to manage.1 VLUs account for up to 90% of all chronic leg ulcers.1 Proper diagnosis and treatment planning are key to wound healing outcomes. This fact is particularly true for older adults, who have an annual VLU prevalence of 1.7%.2
Treatments For Venous Leg Ulcers
The following treatments may be used for venous leg ulcers:
Compression Bandages
The main and by far the most effective treatment for venous leg ulcers are tight compression bandages. They are wrapped around the ulcers and work by helping the static blood near the surface of the leg flow back up the legs and by preventing further pooling of blood and leakage. However, the dressing takes a long time to put on and it can sometimes be uncomfortable and awkward to wear.
Sometimes, compression bandages cannot be used in patients with poor arterial blood circulation. The arteries carry blood away from the heart to all parts of the body and, if the circulation is poor , there will be an inadequate supply of fresh blood to the leg. Arterial insufficiency ulcers can be often treated surgically by bypassing the blockage in the artery. However, venous leg ulcers in patients with arterial disease that is not suitable for such surgery are difficult to treat because compression cannot be applied.
Compression Stockings
Skin Grafting
Skin grafting is sometimes used to treat large venous ulcers that are difficult to heal. A piece of skin is taken from the thigh and applied to the area with the ulcers. Compression is needed after the surgery to prevent the ulcer from returning.
Also Check: Nursing Interventions For Pressure Ulcers
Symptoms Of Venous Insufficiency Ulcers
Whe a venous ulcer begins to develop, stasis dermatitis may be present causing scaling and erythema of the lower extremities. Hemosiderin staining may also occur, causing the presence of brownish or yellow patches underneath the skin. Other skin changes may include the appearance of dark red or purple as a result of blood leaching into the surrounding tissue. Venous ulcers will present with shallow but large wounds with irregular margins that typically develop on the lower leg or ankle. The base of the ulcer is typically red, can result in a significant amount of exudate depending on the level of infection, and will ooze venous blood when manipulated. Typically the wound will be relatively painless, with any pain resulting from subsequent infection or edema. Often the entire leg will become swollen, and the skin will become more firm and reddish brown in color, otherwise known as stasis dermatitis. Elevation of the limb will help to relieve discomfort and swelling.
Figure 1: Venous ulcer with obesity as cofactorFigure 2: Large superficial venous ulcer
Main Causes Of Venous Ulcers
There are a few reasons that venous ulcers occur.
Varicose veins
Venous ulcers can also be caused by varicose veins. In fact, did you know that five to ten percent of people with varicose veins will potentially develop open sores or ulcers? Varicose veins are enlarged, bulgy veins that occur under the skin, but can oftentimes go much deeper to places where you cant even see them. If left untreated, varicose veins can lead to bigger issues such as venous ulcers. Varicose veins cause blood to pool in the lower leg, which can cause a whole slew of issues.
Deep vein thrombosis
According to a National Library of Medicine study, as the pressure in the damaged venous system remains pathologically high, a result of DVT, swelling develops . . . and varicosities often develop. These symptoms are a precursor to chronic venous ulcers, and many patients suffering from deep vein thrombosis experience them.
Recommended Reading: Can You Give Blood If You Have Ulcerative Colitis
Ways To Treat Venous Leg Ulcer And Its Symptoms
Venous leg ulcer is a sore that develops on the leg and heals very slowly, typically due to poor circulation through the limb. The sore may persist for only a few weeks, or it may last for years.
There are preventative steps you can take to keep from getting them. Venous leg ulcers can cause more serious issues if theyre untreated.
The condition occurs when the veins in your leg fail to send blood adequately back to your heart. The built-up backflow of blood increases the pressure at the end of your leg, which weakens this skin.
In turn, its more difficult for a scrape or cut to heal. These ulcers often occur on bony areas like the ankle.
What Questions Should I Ask My Healthcare Provider
You may want to ask your healthcare provider:
- What caused the leg ulcer?
- What is the best treatment for me?
- What changes can I make to heal the wound and prevent future ulcers?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Leg ulcers can be painful, unsightly and difficult to treat. Chronic leg ulcers need specialized wound care to prevent infection and aid healing. Your healthcare provider may recommend other treatments like medicines or procedures to improve blood flow to the leg. Even after they heal, leg ulcers can break open again. Your provider can offer suggestions on how to prevent a wound recurrence.
Last reviewed by a Cleveland Clinic medical professional on 06/23/2022.
References
Recommended Reading: 5 Asa Drugs Ulcerative Colitis
Read Also: Stomach Ulcer Blood In Stool
Trust South Valley Vasculars Expertise
The medical experts at South Valley Vascular in Visalia, Porterville, and Hanford, California, specialize in the diagnosis, treatment, and management of diseases and conditions of the blood vessels. Our vascular surgeons will determine a treatment plan that provides the best benefits for your specific needs.
You May Like: Ulcerative Colitis And Blood Thinners
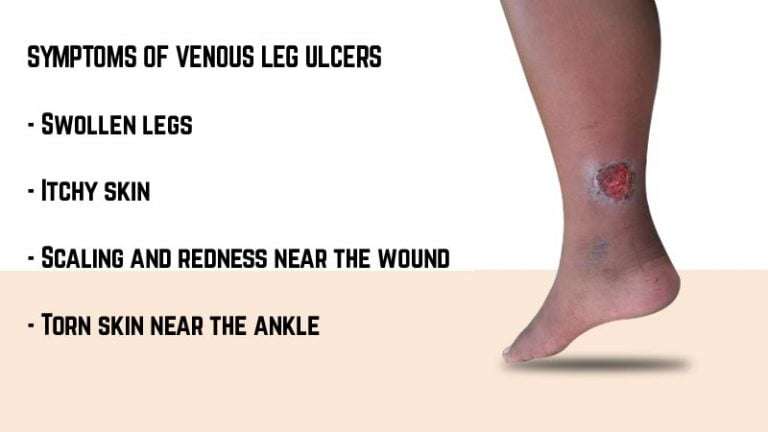
Symptoms Of Venous Leg Ulcers
The signs and symptoms of venous leg ulcers include:
- A dark or patchy colour on the skin of the ankle or calf
- Swelling of the ankles
- Itchy skin with a scaly red rash surrounding the ulcer
- A leakage of fluid from the ulcer
If venous leg ulcers are left untreated, they can become infected. Signs of infection include:
- Redness of surrounding skin
- An increase in the amount of fluid oozing from the ulcer
- An unpleasant, embarrassing smell
Also Check: Corneal Ulcer Dog Home Remedy
What Is A Venous Leg Ulcer
The cause of venous leg ulcers is venous insufficiency due to damage in the valves in the larger veins. Venous leg ulcers can be painless, but some are very painful. They can become infected. There is often an inflammation around the venous leg ulcer.
Competent and well functioning valves are necessary for:
- Fractionating blood flow
When you valves are damaged:
- Blood accumulates in the lower legs
- High blood pressure
This means that the veins or blood vessels by which the blood returns to the heart, are not functioning efficiently, which results in accumulation of the blood in peripheral blood vessels and increased pressure in lower leg veins. The consequence is fluid leackage from the veins beneath the skin. This results in swelling, thickening and damage to the skin. The damaged fragile skin may break down and form an ulcer.
Are Other Venous Ulcer Treatments Available

Venous ulcers that are severe or not responding to standard therapies may require additional treatments such as:
- Growth factor therapy, injectable substances that attract healthy cells to ulcers.
- Hyperbaric oxygen therapy, a treatment in which you sit in a special, pressurized chamber and inhale pure oxygen.
- Lymphedema therapy, massage, skin care and bandaging techniques that clear fluid buildup.
- Skin graft, replacing diseased skin with healthy skin from another part of your body.
- Stem cell therapy, injections of bone marrow to generate healthy tissue.
- Venous disease treatment to correct blood pooling problems and improve circulation.
Recommended Reading: Medications Used For Ulcerative Colitis
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. It’s important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
Identifying Patients At Risk Of Ulceration
Not all people who have CVD will develop ulceration specific risk factors are associated with ulceration in this patient group.
Skin changes are the biggest predictor of lower-leg ulceration: patients with CVD who have varicose veins, lipodermato-sclerosis or venous eczema are at significantly increased risk .
Oedema is the most common cause of lower-leg oedema and present in 90% of cases . It occurs when the rate of capillary filtration exceeds lymphatic drainage because of increased capillary filtration , inadequate lymphatic flow or both . This leads to a build-up of interstitial fluid, causing the lower legs to swell. Chronic oedema is common and its prevalence rises with age from 3.93 per 1,000 in the general adult population to 28.75 per 1,000 in people aged > 85 years .
Lower-limb oedema and CVD both significantly reduce quality of life. Symptoms can include pain, heaviness in the legs, cramps and itching, as well as significant aesthetic effects . When severe, this can lead to reduced mobility, poor body image and social isolation .
Oedema and CVD also have a substantial physiological impact on the skin, causing multiple chemical inflammatory mediators to be released, resulting in the tissue becoming chronically inflamed. This can lead to haemosiderin staining , lipodermatosclerosis and, ultimately, cellular hypoxia and ulceration .
Don’t Miss: How Do You Treat An Ulcer Naturally
Compression Hosiery For Preventing Venous Leg Ulcers Returning
Venous leg ulcers can be caused by a blockage or breakdown in the veins of the legs. Compression, using bandages or hosiery , can help heal most of these ulcers and is also widely used after healing to prevent ulcers returning. One small trial confirms that compression reduces ulcer recurrence compared with no compression. There is some evidence that people wearing high rather than moderate-compression hosiery are less likely to get a new ulcer. It is not clear whether moderate strength hosiery is better tolerated than high compression. There is, therefore, some evidence that compression hosiery might prevent ulcers, but the evidence is not strong.
There is evidence from one trial that compression hosiery reduces rates of reulceration of venous ulcers compared with no compression. Results from one trial suggest that recurrence is lower in high-compression hosiery than in medium-compression hosiery at three years whilst another trial found no difference at 5 years. Rates of patient intolerance of compression hosiery were high. There is insufficient evidence to aid selection of different types, brands, or lengths of compression hosiery.
The majority of venous ulcers heal with compression bandages, however ulcers frequently recur. Clinical guidelines therefore recommend that people continue to wear compression, usually in the form of hosiery after their ulcer heals, to prevent recurrence.
How To Help The Healing Process Along
To help the healing process along, follow these tips:
Do regular self-checks. Catching wounds early is the key to avoiding infections and complications. Make sure you do daily self-checks and look for new wounds, especially on your feet. Dont forget to check in between and under your toes.
Remove dead tissue. Necrosis and excess tissue often occur with diabetic wounds. This can promote bacteria and toxins and increase wound infection. It can also prevent you from being able to inspect the underlying tissue. Your doctor will often help you with the removal process.
Keep dressings fresh. Regularly changing dressings can help reduce bacteria and maintain appropriate moisture levels in the wound. Doctors often recommend special wound care dressings.
Keep pressure off the area. Pressure can cause wear and tear that damages the skin and leads to a deeper wound or ulcer.
If youre dealing with a foot wound, consider wearing white socks during the healing process. This will make it easier to see blood or other signs of drainage on your socks.
See your doctor if you experience any of the following:
- tingling
Also Check: Why Are Bedridden Patients At Risk For Developing Decubitus Ulcers
Also Check: Are Eggs Bad For Ulcerative Colitis
What Is An Arterial Ulcer
Arterial leg ulcers are caused by insufficient arterial blood flow to the lower extremities. The direct cause of reduced blood flow is vessel wall arteriosclerosis and atherosclerotic plaque accumulation causing vessel occlusion. Peripheral vascular disease associated with arterial insufficiency may result in limb tissue ischemia. In case this condition is prolonged, the skin on the leg becomes thin with loss of hair, subcutaneous tissue and muscles atrophy, nails become thickened, leg color and temperature change becoming pale and cool, pulses become difficult to palpate and pain increases with exercise or leg elevation.
The treatment of arterial leg ulcers requires a multidisciplinary approach. It is necessary to ensure a proper blood flow, which often involves surgical intervention. The patient must be encouraged to adopt and maintain healthy lifestyle changes which will help to improve tissue perfusion.
Leg Ulcers: How To Relieve The Pain At Home
Patients most often present with either of the two main types of leg ulcers: venous or arterial. Less frequently, people suffering from diabetes can develop neuropathic ulcers as a result of unstable blood sugar.
Most often associated with varicose veins, venous ulcers make up the lionâs share of leg ulcers with 85% of diagnoses. These ulcers take a long time to heal, and it is a painful process. Worse still, 75% of these painful ulcers will reoccur. Home treatment and surgical intervention can help ease the pain associated with these types of wounds.
Also Check: Different Types Of Ulcerative Colitis
What Is Daily Life Like With A Venous Ulcer
While youre undergoing treatment, there are steps you can take to promote healing. These include:
- Eating a healthy diet, which supports your bodys natural healing abilities.
- Keeping the ulcer and nearby skin clean.
- Periodically raising your legs when seated to avoid blood pooling.
- Staying active with gentle exercises, like walking.
A note from Cleveland Clinic
Venous stasis ulcers are wounds that are slow to heal. They typically occur in people with vein issues. Timely specialized care is necessary to prevent complications, like infections that can become life-threatening. Nonhealing ulcers also raise your risk of amputation. Venous ulcers can come back after treatment, which is why care often includes preventive therapies. Most people make a full recovery. But its essential to follow all care instructions.
How To Use Honey For Leg Ulcers

You May Like: How To Treat An Ulcer In Your Mouth
What Is A Venous Stasis Ulcer
To understand venous stasis ulcers, you need to know what it is and what causes these ulcers to develop.
Venous stasis is a term used to refer to blood pooling in your veins. This tends to happen when the valves within these blood vessels stop working properly. Veins carry blood back to the heart and this blood does not move at the same velocity as the blood being pumped from the heart to the arteries. As such, the venous valves are required to prevent blood from moving back in the wrong direction. When you have issues with your valves, you can end up with blood pooling in the veins. When this occurs, it is known as venous stasis.
But what is a venous stasis ulcer? A venous stasis ulcer is an injury or wound caused As the blood pools, it starts to affect nearby tissues and cause fluids to leak out. This leads to inflammation in the area, which will create ulcers on the surface of your skin.