Who Is A J
J-pouch procedures have become the gold standard for treating chronic ulcerative colitis in which medical therapy has failed to control a patients symptoms. J-pouches also are used for familial adenomatous polyposis , and for selected patients who have been diagnosed and treated for colon and rectal cancer.
It Can Help To Meet Your Ostomy Care Nurse Before Your Operations
You may want to ask your doctor whether you can meet your enterstomal therapist, who can help you get comfortable using these bags, says Cristal Steuer, 39, who had her surgery in 2011. Enterstomal therapists are nurses who specialize in ostomy care, and some hospitals like the UNC School of Medicine allow you to meet with your nurse before your operation. Scheduling time with your nurse before your surgery can help you get more comfortable using the ostomy bags . And after the surgery, your doctor might not be as responsive as youd like, Steuer explains. When she was having issues with her ostomy, she would call the nurse and get a reply faster than if she tried to reach a doctor. I used to get terrible rashes around where you would stick the bag on. The ostomy care nurse would give me tips to fix that, or if something wasn’t working or if I had symptoms, I could find out if it was worth coming into the hospital, she tells SELF. The ostomy nurses were readily available and were very supportive. They deserve a lot of praise.
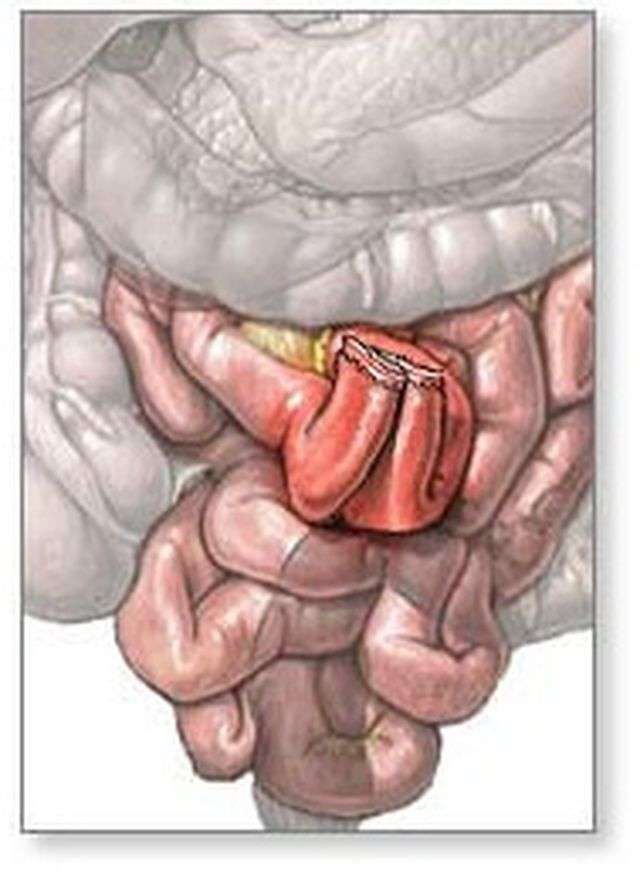
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
You May Like: Nutritionist Specializing In Ulcerative Colitis
One Step And Three Step Procedures
Occasionally, a surgeon and patient will decide to complete the entire procedure in one step. The surgeon will perform the colectomy, create the j-pouch and connect it all in one operation. The one step eliminates the need for a second or third surgery or a temporary ileostomy. In recent years the practice of doing this surgery all in one step has come into question because there may be a greater risk of pouch-related complications.
If a patient is very ill, the surgeon may elect to use three steps to complete the procedure. In the first step, the colectomy is done, and the temporary ileostomy is created. In the second step, the j-pouch is constructed, and the third step is the takedown. The wait between each of these surgeries is two to three months, depending on the health of the patient. The intervals may be longer for patients who were quite ill at the time of the colectomy. While three surgeries is a major investment, there is some evidence emerging that three surgeries may be associated with a lower risk of complications in the long run.
General Tips For Recovery
- Keep busy. Don’t stay home because you are having more bowel movements. Most people do not have many bowel movements during the day when they are away from home. They tend to have more when they get home in the evening.
- Start a regular exercise program, such as walking, swimming or playing a sport.
- Many people get frustrated about their progress after surgery and want a quicker recovery. Remember that this is a major operation and you will need time to feel better.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Read Also: Low Dose Naltrexone Ulcerative Colitis
A Messy Part Of Having Ulcerative Colitis
When I had a diseased colon, bowel movements were always a very messy business. Little did I know, j-pouches are ten times worse. I can clean the toilet and by the time my next bowel movement is over, it looks as though I never cleaned it at all.
This is very bothersome for meespecially when Im visiting someone elses house. Not everyone keeps a toilet brush in plain sight, so what you might consider doing is investing in one of those toilet brushes with a disposable head. It may be somewhat of a hassle, but at the end of the day, I feel it is only polite for me to clean up the mess my j-pouch made.
Foods That May Cause Diarrhea
Diarrhea occurs when food moves through your digestive system too quickly. The colon is responsible for reabsorbing extra water from stool. And when you dont have a large colon, stool tends to be looser.
Diarrhea, which is when stools are very watery and frequent, can also lead to dehydration. This can be dangerous, particularly for a person recovering from surgery and unable to eat a full diet.
The following foods are more likely to cause diarrhea:
- high fat or fried foods
- spicy foods
- high sugar foods and drinks, especially sodas or juices
- foods and drinks with caffeine, including coffee, teas, chocolate, or energy drinks
- alcohol
Also Check: Is Ulcerative Colitis A Gastrointestinal Disease
Your Bowel Movements Will Probably Change
Once youve had the final operation to connect the pouch, your bowel movements will be different: At first, you may go to the bathroom every hour, but the frequency will decrease as your muscles become stronger. Dr. Remzi tells his patients that once theyve recovered, they can expect to have three to nine bowel movements throughout the day.
Shortly after her surgery, Steuer says she would need to go to the bathroom almost immediately after eating. But now, I can definitely sit at a dinner table and talk for a little while before I have to get up, she says.
You may also notice that your stool smells differently, which Hooks describes as being somewhat stronger than it was when I had my colon. If the scent bothers you, Hooks swears by using a deodorizer that you spray directly into the toilet before using it. Honestly, I believe everyone should use this whether you are living with a J-pouch or not, she says. Poo-Pourri Before-You-go Toilet Spray is one popular option .
What Happens During Surgery
The J-pouch has really become the preferred standard of care for a person with colitis, Dr. Steven D. Wexner, Director of the Digestive Disease Institute at Cleveland Clinic Florida and Chairman of the Department of Colorectal Surgery, told Medical News Today.
Depending on a persons overall health, the surgery may involve two or three procedures.
In the initial procedure, a surgeon will remove the colon and rectum but leave the muscles that surround the rectum and the anus. They will then construct the J-shaped pouch from the end of the small intestine before attaching the pouch to the anus.
The first procedure is known as an ileostomy. During this surgery, a surgeon will create a temporary opening in the wall of the abdomen and attach the end of the small intestine to this opening. This allows stool to pass through into an attached ostomy bag while the small intestine and sphincter heal.
After 812 weeks, a person will undergo the second surgical procedure, in which a surgeon will reverse the ileostomy by reconnecting the small intestine. At this point, the person will be able to have a normal bowel movement.
If the surgeon needs to perform the surgery over three separate procedures, they will:
People who may require three surgeries rather than two include those:
- on high dosages of steroids
- in poor health
Don’t Miss: Signs Of Having An Ulcer
Whats Safe To Eat Or Drink
After surgery, youll start with a clear fluids diet. This allows your body to get some nutrients, while letting your digestive system rest and heal.
A clear fluids diet includes:
- gelatin
- puddings
- fully pureed soups
A full fluids diet provides a bit more variety and texture. But its still easy for your digestive system to handle.
Once you can tolerate a full fluids diet, youll transition to a low fiber diet. This is also known as a low residue diet.
This adds more solid foods into your diet without adding bulk. It includes a variety of foods that your body can still digest easily.
A low fiber, or low residue, diet includes the foods and drinks in a full fluids diet, plus:
- well-cooked vegetables without any skin or seeds
- soft fruit without skin or seeds
- soft starchy foods like white bread, white rice, and white pasta
- soft and well-cooked meats, poultry, and fish
- milk, cheese, and yogurt as well as non-dairy alternatives
- smooth nut butters
- eggs
Are There Any Risks Or Complications To Be Aware Of
Despite the potential benefits, the J-pouch procedure is still considered major surgery. As with any major surgery, you may be at risk for infections, bleeding, and side effects from general anesthesia.
Sometimes its possible for the newly formed J-pouch to become infected. However, such risks are higher in one-stage procedures.
Other potential complications from this procedure include:
Overall, the outlook for J-pouch surgery is positive, with few people experiencing pouch failure.
However, one study published in 2015 reported a J-pouch failure rate of between 3.5 and 15 percent. Pouch failures have also been found to be more common in men than women.
If you do develop pouch failure, your doctor may recommend either an ostomy or another type of colorectal procedure called a K-pouch surgery.
Pouchitis is the most common problem following J-pouch surgery and other pouch surgeries. This is a treatable condition and does not necessarily mean youll develop pouch failure. However, chronic pouchitis has been linked to possible failure of the J-pouch.
Recommended Reading: What Does An Ulcerative Colitis Flare Up Feel Like
Why Would Someone Get J
Someone might get J-pouch surgery for any of these reasons:
- Treating chronic ulcerative colitis . Most often, this procedure is used to treat chronic UC-related conditions, which carry a pretty big risk of colon or rectal cancer. J-pouch surgery is the most common procedure used to treat UC.
- Failure of UC meds. Its typically recommended only when UC medications fail to control the condition. Then, J-pouch surgery may be the next method of treatment.
- Treating cancerous or precancerous conditions. J-pouch surgery is sometimes performed to treat colon or rectal cancer or as a preventive measure when precancerous changes are detected.
- Addressing emergency conditions. J-pouch surgery is sometimes performed in emergency situations such as uncontrolled gastrointestinal bleeding or toxic megacolon .
You might be a candidate for J-pouch surgery if:
- your UC symptoms have persisted despite medication
- your UC symptoms are getting worse
- UC causes you to miss multiple days of school, work, or daily activities
- you have precancerous colon cells
- you have colon or rectal cancer
- youre experiencing uncontrollable bleeding from your colon
- your doctor has found holes in your colon due to chronic inflammation
- you need surgery to remove your colon, but youd rather have an internal pouch to collect waste than an external one
- you and your doctor decide that the procedures benefits outweigh the potential risks
Creation Of Ileoanal Pouch And Anastomosis
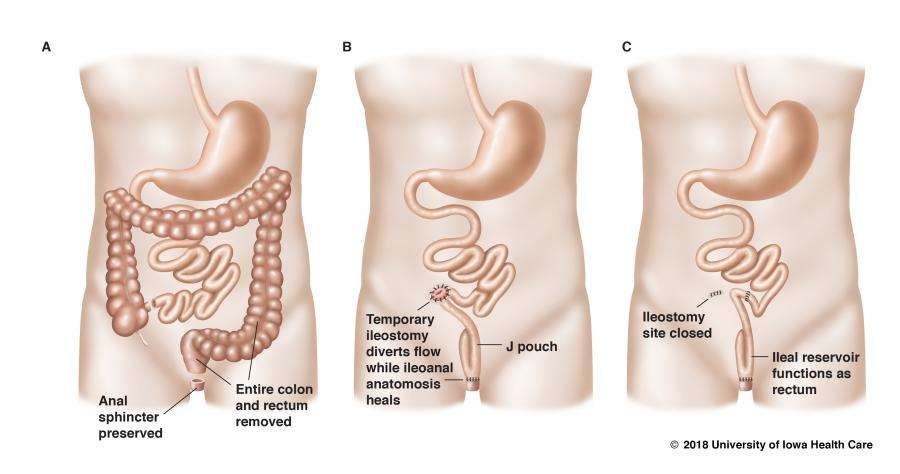
The key to successful pouch surgery is a tension-free anastomosis. For this reason, the small bowel mesentery should be mobilized adequately as far as the third part of the duodenum so that the ileal pouch will reach to the level of the levator floor with no tension. The reach of the ileal pouch to the anal canal in obese patients or in patients who had a prior small bowel resection might be difficult. The technique by grasping the apex of the pouch and simulating the reach down to the anastomosis level is useful to estimate the tension . Ileocolic vessels ligation at the origin of the superior mesenteric artery can be done to provide an anastomosis with no tension. This is especially a must when one has to do an S-pouch rather than a J-pouch due to reach issues. If there is still tension after these maneuvers, the peritoneal tissue to the right of the superior mesenteric vessels is excised using translumination. Also, small anterior and posterior peritoneal incisions over the superior mesenteric vessels border can be done as an additional maneuver .
An IPAA is constructed using either a stapled or hand-sewn technique. A stapler IPAA is a preferred technique over a hand-sewn IPAA because it is quicker and associated with better outcomes. The stapled IPAA is performed using either single- or double-stapling approaches.
Recommended Reading: How Does Ulcerative Colitis Affect The Body
Before During And After J
The ileal pouch-anal anastomosis procedure, commonly known as a J-Pouch procedure, is a complex surgical treatment for severe disease or injury affecting the large intestine . This procedure is designed to remove the damaged tissue of the colon and allow the patient to continue to have normal bowel movements, meaning stool leaves the body through the anus.
During the J-Pouch procedure or more often multiple procedures the colon is surgically removed and the small intestine is reconstructed to allow for stool to exit the body through the anus in a controlled fashion.
Before The First Operation:
The first operation involves removing your large intestine and creating the pouch. Prior to having this first operation several tests will be done. Tests that may be necessary include:
- Blood work
- Upper GI X-rays
- Colonoscopy
All patients need to have a colonoscopy performed at UNC Hospitals prior to surgery. This is an exam of the colon where a lighted flexible tube is inserted into the rectum so the inside of the entire large bowel can be visualized. It shows the surgeon the amount of disease in your intestine. You will be given instructions for a bowel prep when the appointment is made for your colonoscopy. During the exam you will be given medicines to sedate and relax you. In addition to the GI endoscopist, the surgeon or an assistant may be in the room during this exam. The surgeon will be given a full report and pictures by the doctor performing the test. This examination is often performed the day before your surgery.
Recommended Reading: How Do You Heal An Ulcer
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
The Clinic Visit Following The Operation
You will be scheduled to come back to clinic 1-2 weeks following discharge after the first operation. At this time you will be given a physical exam by your surgeon and be asked questions about how you have done following the operation. The second stage of IPAA can be discussed and a date decided upon. You can also see the enterstomal therapist at this time as well as other members of the team. The second stage of IPAA will take place sometime after 6 weeks, but usually not before.
Recommended Reading: Foods To Eat To Heal An Ulcer
Incorporation Of Vaginal Wall Into The Anastomosis
In female patients, one must always be aware of the risk of incorporating the vaginal wall during creation of the pouch-anal anastomosis as the posterior wall of the vagina may fall into the circular stapler as it is being closed. The perineal operator must always check the vagina digitally to be clear before employing the end-to-end stapler. If inspection of the anastomotic donuts after firing the stapler reveals a third portion of tissue, it is necessary to take down the anastomosis, repair the vaginal defect, and redo the pouch anastomosis.
Ulcerative Colitis Surgery Cost
As surgery for ulcerative colitis requires at least one and possibly three hospital stays, it comes at a higher cost than procedures that can be done as outpatient surgery. Ileostomy surgery may cost approximately $39,000, while j-pouch surgery may cost $50,000.
Check with your insurance provider to find out how much will be covered and what co-pays may be required. Using a hospital and surgical team in your plan’s network is key to preventing any unexpected charges.
Recommended Reading: Mouth Ulcer On Tongue Remedies