Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with Crohns and Colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 140,000 members come together to ask questions, give advice, and share their stories with others who understand life with IBD.
Have you ever experienced uveitis or other eye problems? Share your experience in the comments below, or start a conversation by posting on your Activities page.
What Is Life Like With Ulcerative Colitis
The only cure for ulcerative colitis is complete surgical removal of the colon. However, most patients will not require surgery to have their symptoms under control, and some patients may have complications after the surgery such as pouchitis. Whether they require surgery or not, our goal is to allow our patients to live a full and productive life with ulcerative colitis. Most patients will require medications for an indefinite period of time. Research has shown that patients with ulcerative colitis who do not take their medication, even if they are feeling well, are more likely to have a return of their symptoms compared to patients who continue their medications. It is very important that patients discuss with their doctor if they are considering stopping their medications.
It is important for patients with ulcerative colitis, even if they are feeling well, maintain regular visits with their physician. For example:
- Patients on medications may need routine blood work to monitor for side effects.
- Patients with ulcerative colitis should keep up to date on immunizations including influenza , pneumococcal , human papilloma virus , and hepatitis A and B.
- Some patients with ulcerative colitis, particularly those who have had been exposed to steroids , may need to have bone mineral density tests to screen for early osteoporosis.
- Patients with ulcerative colitis will need to have colonoscopies to screen for colon cancer.
Which Is Worse Crohns Or Colitis
Official Answer. Although ulcerative colitis and Crohns disease are both long-term, inflammatory conditions that affect the digestive tract, ulcerative colitis may be considered worse because surgery may be required earlier and, in certain circumstances, more urgently, in people with severe and extensive UC.
You May Like: Symptoms Of Intestinal Ulcers In Humans
Poor Growth And Development
Ulcerative colitis, and some of the treatments for it, can affect growth and delay puberty.
Children and young people with ulcerative colitis should have their height and body weight measured regularly by healthcare professionals.
This should be checked against average measurements for their age.
These checks should be carried out every 3 to 12 months, depending on the person’s age, the treatment they’re having and the severity of their symptoms.
If there are problems with your child’s growth or development, they may be referred to a paediatrician .
Ibd In Population Genetics

Detection of natural selection in the human genome is also possible via detected IBD segments. Selection will usually tend to increase the number of IBD segments among individuals in a population. By scanning for regions with excess IBD sharing, regions in the human genome that have been under strong, very recent selection can be identified.
In addition to that, IBD segments can be useful for measuring and identifying other influences on population structure. Gusev et al. showed that IBD segments can be used with additional modeling to estimate demographic history including bottlenecks and admixture. Using similar models Palamara et al. and Carmi et al. reconstructed the demographic history of Ashkenazi Jewish and Kenyan Maasai individuals. Botigué et al. investigated differences in African ancestry among European populations. Ralph and Coop used IBD detection to quantify the common ancestry of different European populations and Gravel et al. similarly tried to draw conclusions of the genetic history of populations in the Americas. Ringbauer et al. utilized geographic structure of IBD segments to estimate dispersal within Eastern Europe during the last centuries. Using the 1000 Genomes data Hochreiter found differences in IBD sharing between African, Asian and European populations as well as IBD segments that are shared with ancient genomes like the Neanderthal or Denisova.
You May Like: How To Heal Colon Ulcers
Ulcerative Colitis And Joint Pain
When you have ulcerative colitis , its normal to have pain in your abdomen, along with diarrhea and other gastrointestinal symptoms.
Up to 30 percent of people with UC also have arthritis, which is characterized by swollen, painful joints.
Heres a look at the connection between UC and joint pain, as well as what you can do to protect your joints if you have UC.
What Are The Complications Of Ulcerative Colitis
UC can also lead to complications, especially if left untreated or if you dont follow the directions for your medications to a T . Common complications of UC include:
-
Rectal bleeding, which can lead to iron-deficiency anemia
-
A rupture of the bowel
-
Increased risk of colon cancer
-
Deficiencies in vitamins and minerals, which can lead to bone loss in the form of osteopenia or osteoporosis
-
Inflammation throughout the body, such as the eyes, skin, and joints
If youve had surgery for UC, keep in mind there may be surgical complications as well. Talk with your doctor about any warning signs to watch for.
Recommended Reading: Foods Not To Eat With Ulcerative Colitis
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Uveitis Eye Condition And Inflammatory Bowel Disease
Inflammatory bowel disease not only affects the digestive tract but is also associated with conditions in several other parts of the body. The eyes seem like an unlikely place to be affected, but in fact, there are several eye conditions that are more prevalent in people who have IBD. Uveitis is an uncommon eye condition associated with IBD. If untreated, it can lead to loss of vision.
People with IBD not only need regular care from a gastroenterologist, but regular care from an eye doctor is also needed. Uveitis and other eye conditions associated with IBD aren’t common but it is important that they get diagnosed and treated right away if they do develop. People with IBD who have sudden eye pain or other symptoms in the eye should see an eye doctor right away and then call their gastroenterologist.
Uveitis is an inflammation in the middle layer of the eyethe uvea. The uvea contains the iris , ciliary body , and choroid . Uveitis can be a chronic condition. Types of uveitis include:
- Anterior: Inflammation is located in the iris
- Diffuse: Inflammation throughout the uvea
- Intermediate: Inflammation is in the ciliary body
- Posterior: Inflammation of the choroid
Recommended Reading: Wound Care For Diabetic Leg Ulcers
Back Pain Often Comes Directly From Back Or Spinal Structures But Sometimes Its A Sign Of A Medical Condition Elsewhere In Your Body Heres What Else Could Be Causing Your Back Pain
Heres a scene that plays out every day, all over the world: Someone thinks they have a little back strain. Perhaps they lifted something wrong or moved the wrong way. It was just a twinge, so they waited it out a few days for the pain to go away. It doesnt, so they head to their doctor. Turns out, they hadnt lifted anything wrong at all. It was the start of a kidney infection, or a UTI, or pancreatitis.
Heres how to tell the difference between a back strain and something more serious going on.
How do you know when the root cause of back pain is elsewhere in your body? There are two types of pain we look at, explains Matthew Crooks, MD, a pain specialist at Pinnacle Pain and Spine in Scottsdale, Arizona: visceral pain and somatic pain. Visceral pain is pain from an organ or internal pain that can radiate to the spine with conditions like pancreatitis, ulcerative colitis or Crohns disease, gall stones, cancers, kidney pain, and urinary tract infection, says Dr. Crooks.
Whats more, thanks to aging, injury, or a sedentary lifestyle, almost everyone has some wear and tear in the spine and pain in the musculoskeletal system . When you do develop visceral pain, it can flare up your somatic pain. And thats separate from the pain thats radiating from an organ, says Dr. Crooks. It can be activated from overall inflammation and the stress of the body dealing with the medical issue. Its the BOGO special that you never want.
Donât Miss: Succeed For Horses With Ulcers
Can You Eat Liver With Ulcerative Colitis
What are the diet recommendations for ulcerative colitis? People with ulcerative colitis often suffer from iron deficiency resulting from blood losses. This can be corrected with iron supplements or by eating high iron foods such as liver, beef, turkey, lamb, tofu, spinach, molasses, oatmeal, and eggs.
Read Also: Why Does Ulcerative Colitis Happen
Eye Problems Associated With Ibs
Since IBS is a chronic condition, there are some potential impacts on other parts of the body, including the eyes. These include the following:
- Light sensitivity
- Dry eyes
- Painful, red eyes
One survey found that eye problems occurred in 4 to 10 percent of people with IBS and seemed to be more common in Crohns disease than ulcerative colitis.
The list of eye conditions associated with IBS includes:
These conditions could develop before or after the diagnosis of IBS, but they tended to be associated with the onset of other symptoms.
Corticosteroids are the first choice for reducing inflammation associated with many autoimmune conditions, including IBS. These can help reduce swelling associated with parts of the eye too.
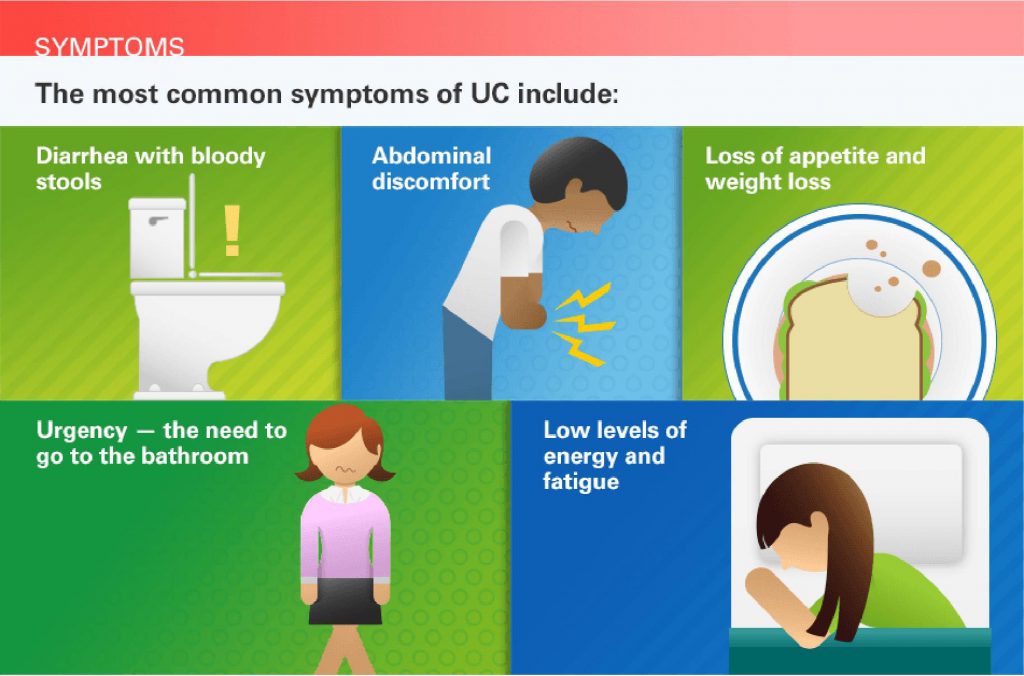
Signs And Symptoms Of Ulcerative Colitis
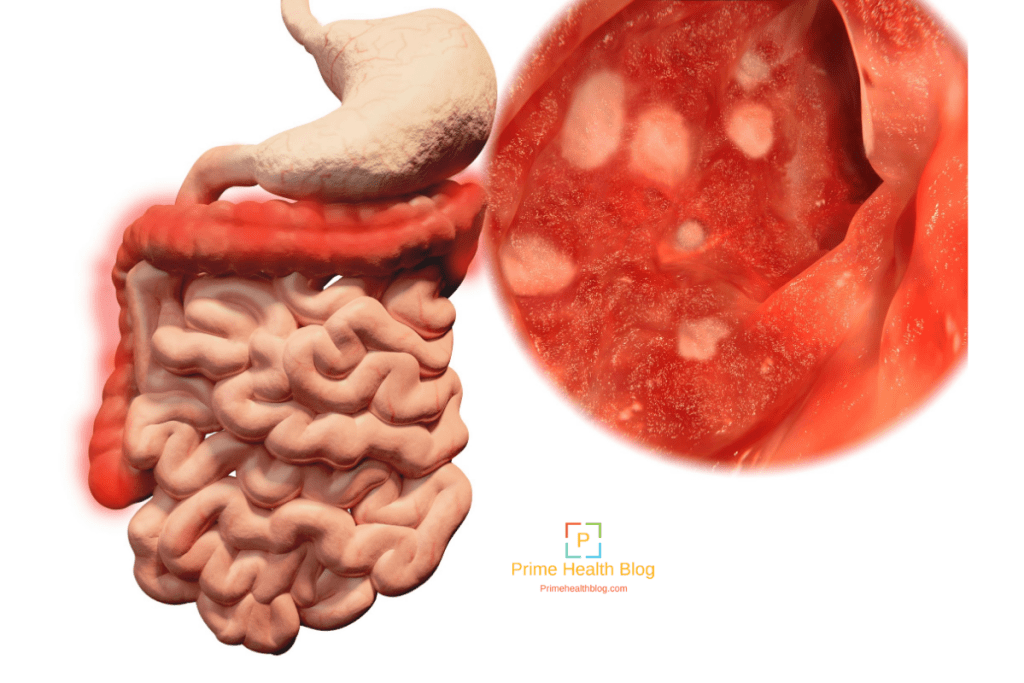
Recognizing the symptoms of ulcerative colitis is your first step toward knowing when your disease is in a flare and when to seek medical attention.
The symptoms of ulcerative colitis vary from person to person and about half of all ulcerative colitis patients experience mild symptoms. If you experience any of these symptoms, consult your healthcare provider.
-
Loose and urgent bowel movements
-
Bloody stool
-
Persistent diarrhea accompanied by abdominal pain and blood in the stool
Recommended Reading: Do You Still Have Ulcerative Colitis After Colectomy
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Treat Ulcerative Colitis Effectively
Your health care provider may determine that you are experiencing a puffy face as the result of an ulcerative colitis flare-up. In this case, treating your ulcerative colitis itself may help manage puffiness, as well.
Based on the medical advice you receive, you may need to take anti-inflammatory drugs, immunosuppressant drugs, or biologics to control ulcerative colitis effectively. Once the UC is under control, your puffy face may disappear, too.
Read Also: Can You Feel A Stomach Ulcer
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Also Check: How To Heal Ulcers In Large Intestine
Episcleritis Scleritis And Uveitis
Episcleritis, scleritis, and uveitis are all conditions that can cause swelling in different parts of the eyes. When swelling in the eyes becomes severe enough, it can make the face look swollen and puffy. These eye conditions tend to flare when bowel problems flare, so they are considered related conditions. Steroid drops usually help with the inflammation.
Reducing Your Arthritis Risk When You Have Ulcerative Colitis
Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis werent enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although its not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.
Also Check: Signs And Symptoms Of Peptic Ulcer
Don’t Miss: Can Stress Cause Flare Up Ulcerative Colitis
Coping With Ulcerative Colitis Skin Problems
Theres really nothing you can do to prevent any of the skin conditions related to ulcerative colitis, says Hagan. But since many of these problems coincide with flares, it can be helpful to manage the underlying ulcerative colitis as much as possible.
It can also be helpful to reduce stress, which can trigger flares and, in turn, skin problems, says Papantoniou. Meditation or deep breathing may be very helpful in reducing stress, she adds.
To minimize the outward appearance of skin problems, try covering up problem areas with clothes if you can and makeup is okay in some cases.
As long as the skin barrier isnt broken, its safe to cover up hyperpigmentation or red patches with a concealer, says Papantoniou. Ask your healthcare provider which products are safe for you to use.
Additional reporting by Jordan M. Davidson.
How Is Diagnosis The Same And Different
If you think you have either UC or diverticulitis, talk to your doctor about it. You might be referred to a gastroenterologist, a doctor who specializes in digestive issues, for a correct diagnosis.
Your doctor will first do a detailed medical exam. Theyâll ask you about your medical history including things like your diet, your bowel movements, and medications you might be taking.
Common tests to diagnose UC and diverticulitis include:
- Blood tests. This is done to check for infections
- Stool sample test. This checks for bacteria or parasites that might cause your stomach pain, cramps, or diarrhea
- Colonoscopy. The doctor will use a thin, flexible tube with a camera on the tip to explore your entire colon. They may take small tissue samples to test.
- Flexible sigmoidoscopy. This is similar to a colonoscopy, except your doctor will only explore your rectum and s-shaped sigmoid colon â both of which are located at the lower end of your colon. This is usually done if you have severe inflammation.
- Barium enema. This test is also called lower gastrointestinal tract radiography. In this test, your doctor injects a liquid containing barium into your butt. The barium coats your entire colon and makes it easier to see clearly under an X-ray scan.
- CT scan. This test allows your doctor to scan your abdomen and pelvic area and spot inflamed areas in your colon. The scan can detect the irritated or inflamed pouches for diverticulitis and confirm the condition.
You May Like: How Do You Treat A Duodenal Ulcer
He Had Recurring Pain For Nearly A Decade
- Read in app
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.