Refined Vs Unrefined Rice
Refined rice, commonly called white rice, is the same as brown rice with one big difference: the bran and germ are removed. This makes white rice more tender and delicate, and it breaks down faster during long cooking processes. Brown rice, also known as whole-grain rice or unrefined rice, comes in multiple colors, including red, brown and black. Whole-grain rice has a chewier texture and nuttier flavor as well as more dietary fiber and essential nutrients, such as protein.
Cabbage Celery And Brussels Sprouts
Avoid eating cabbage, celery, and Brussels sprouts because they are high in fiber and potential colon lining irritants. Instead, have sweet potato, potato, carrots, and squash.
NOTE: Dairy is not mentioned in this list because a few people do not get ulcerative colitis flare-ups while others do. So, check with your doctor to find out if you can consume dairy products.
It may seem like you have run out of options to eat, but thats not the case. Here is the list of foods that you can eat.
Our Own Recommendations For An Ibd Diet
We also have previously developed and tested an anti-IBD diet that restricts disaccharides wheat and other grains except white rice polyunsaturated fatty acids and most saturated fats processed meats and large amounts of red meats and is devoid of all additives and preservatives. Additionally, foods that are rich in protease inhibitors were reduced/avoided and foods were advised to be cooked , since cooking with heat exposure reduces protease inhibitor content of foods. Protease inhibitors naturally occur in plants to neutralize digestive proteases in the intestinal lumen of the consuming person as well as those released by pests of the plant and are a survival/defense mechanism of the plant. However in the GI tract, neutralization of digestive proteases by large amounts of protease inhibitors within the food, also allows for bacterial toxins to survive small bowel transit, and thereby potentially create inflammation in the distal parts of the GI tract. One such example is a disease called pigbel which is a Clostridial bacterial toxin related acute or chronic necrotizing enteritis initially noted in the Papua New Guinea Highlanders who consume large amounts of foods that contain trypsin inhibitors .
Also Check: Colon Cancer Symptoms Vs Ulcerative Colitis
Diet Tips And Preventing Flare
When a person is not going through a flare-up, switching to a high-fiber diet can help with their Crohns disease. This diet promotes digestive regularity and good health.
There is no single food or food group that doctors link with every instance of Crohns disease. Different people may have different foods that might irritate the gut and contribute to inflammation.
Doctors will often recommend that people with Crohns disease keep a food journal of everything they eat and in what amounts. A person will be encouraged to list the symptoms if any they experience after eating certain foods.
Common foods that may worsen symptoms include spicy foods, dairy products, alcohol, and high-fiber grains. However, these are not triggers for all people with Crohns disease.
Additional considerations and diet tips for a person with Crohns include:
- Eating several small meals each day instead of large ones to reduce reflux and gas.
- Drinking plenty of water throughout the day to help digestion.
- Adding fiber sources slowly and drinking plenty of water to help the body adjust.
A person should also ask their doctor if there are any specific recommendations they should follow, regarding their diet.
Food Preparation And Meal Planning

While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Read Also: How To Apply Compression Bandages For Leg Ulcers
What Foods Should I Eat When My Ulcerative Colitis Is In Remission
You should try and maintain a diverse and nutrient-rich diet even when you are in remission and your symptoms have reduced or gone away completely. Keep a food diary and introduce new foods slowly, so you understand which ones trigger your symptoms. Keep well hydrated with water, broth, tomato juice, or rehydration solutions, and avoid making large changes in your diet without your doctors advice. Eat foods such as:
- Fiber-rich foods such as oat bran, beans, barley, nuts, and whole grains, unless your doctor has advised you to stick with a low fiber diet or you have an ostomy or intestinal narrowing
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Fruits and vegetables of all colors remove the peel and the seeds if they trigger your symptoms
- Calcium-rich foods found in collard greens, yogurt, kefir, and milk
- Probiotic foods such as yogurt, kimchi, miso, sauerkraut, or tempeh.
You May Like: Stage Iv Sacral Decubitus Ulcer
Adherence To Gfd And Correlation With Symptom Improvement
In those patients who were still following a gluten free diet , adherence was found to be excellent in 41.5%, average in 34.1%, and fair/poor in 24.4%. Excellent adherence to a GFD was associated with reduced fatigue, as compared to fair/poor adherence . Adherence was not associated with significant differences in other clinical symptoms.
Read Also: Early Symptoms Of Ulcerative Colitis
Recommended Reading: Is Ulcerative Colitis A Gastrointestinal Disease
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
Also Check: Foam Dressings For Pressure Ulcer Prevention
Practical Considerations For Treating & Controlling Ulcerative Colitis
The fact is that there are precious few drug-free tools that can reduce symptoms and improve the inflammatory condition characterized by this disease. Yes, diet and nutrition are critical you should think of them as a combination of medication they are equally important.
Stress is another huge factor. It is important to reduce stress in order to make the symptoms less severe. It is of paramount importance for patients to their treatments regularly and not deviate. Also, while smoking has been shown to reduce some of the inflammation of ulcerative colitis, for obvious health reasons its definitely not a recommended treatment.
There is a link between diet and the day to day health condition of someone living with ulcerative colitis. Once again, a food diary is essential so you can document when certain foods make your symptoms worse eliminate them! Without a food diary this is difficult to do as we dont always have good food memory.
Its possible that people with UC who are sensitive to the sugar in milk, such as Lactose, may be experiencing symptoms similar to those of ulcerative colitis. Despite not being the cause of the ulcerative colitis, eliminating milk may help some people.
Its important to make sure the diet you follow is good for you, and it may require the professional help of a nutritionist or dietician experienced with needs of UC patients.
Probiotics
Traveling With Ulcerative Colitis
Don’t Miss: Best Prebiotic For Ulcerative Colitis
What Is Crohns Disease
Crohns disease is a kind of problem relating to bowel disease. It is briefed as IBD which is inflammatory bowel disease. It results in the inflammation in your digestive tract. Consequently, there may be severe diarrhea, weight loss, abdominal pain, and malnutrition. Actually, inflammation resulted from Crohns disease could involve to various areas of the digestive tract among different individuals. It can exert its effects on all parts of your gastrointestinal tract, including the mouth, anus, etc. This problem is popular among Americans. In addition, IBD tends to affect the people over 60. The inflammation associated with Crohns disease usually spreads deeply into the affected bowel tissues layers.
People with this disease both feel debilitating and painful. Sometimes, it may cause life-threatening complications.
What Are Common Causes And Risk Factors?
Actually, the root cause of Crohns disease is not clear.
In the past, stress and diet were blamed to be the triggers of this condition, yet now doctors know that such factors might worsen yet do not cause Crohns disease.
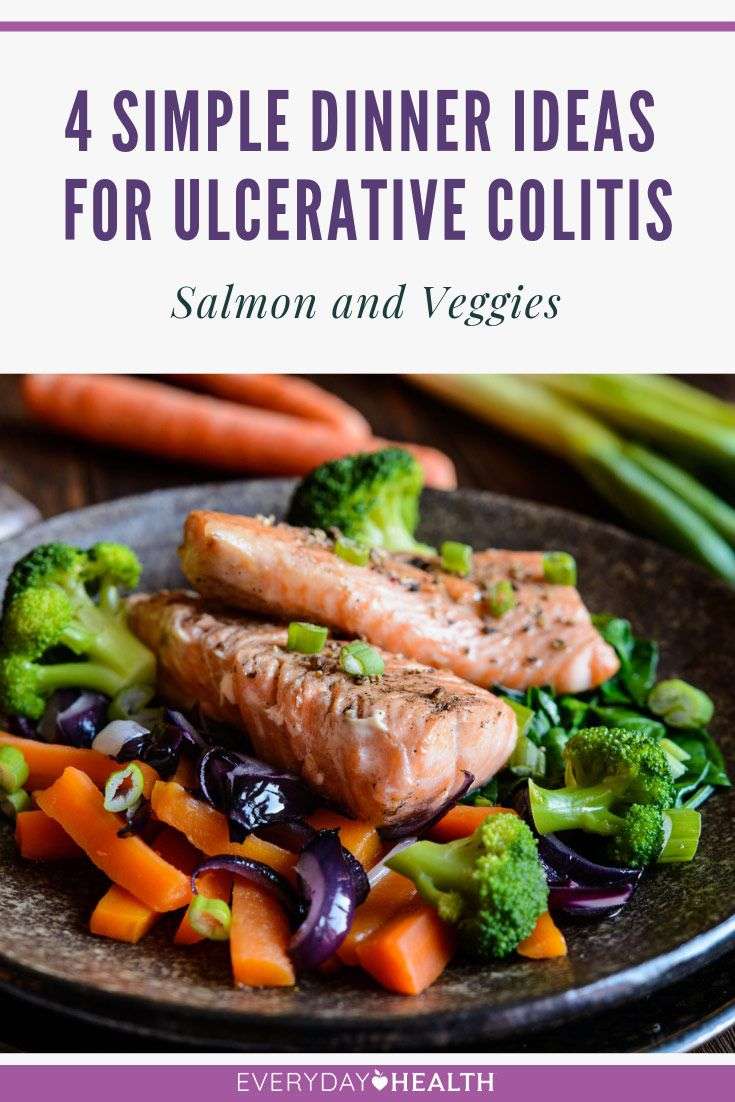
Ditch Unhealthy Fats For A Happier Digestive Tract
A Inflammatory Bowel Diseases found that diets high in trans fats, such as the hydrogenated oils found in processed foods, as well as peanut, canola, sunflower, and safflower oils, were more likely to trigger inflammation and caused a higher risk of ulcerative colitis. In contrast, people who consumed more omega-3 fatty acids, found in fatty fish, had a lower risk of UC. Another International Journal of Molecular Sciences reported that omega-3 fatty acids reduced intestinal inflammation, maintained remission, and improved quality of life.
Dr. Dassopoulos recommends limiting unhealthy fats for overall health. This includes saturated fats found in red meat. My advice to people with ulcerative colitis and Crohns disease is to follow a healthy Mediterranean diet and limit red meat, Dassopoulos says.
Dont Miss: Signs You Have A Stomach Ulcer
Recommended Reading: Remicade Vs Humira Ulcerative Colitis
The Ulcerative Colitis Diet
1. Omega-3 Fatty Acids
Studies have found that an omega-3 fatty acid called eicosapentaenoic acid has the power to fight inflammation. It blocks certain chemicals in your body called leukotrienes. A benefit of fish oil is its a good source of EPA, and in some tests, people benefited from very high doses of it.
A 2010 case report published in the Journal of the Royal Society of Medicine evaluated a 38-year-old woman who had ulcerative colitis and used omega-3 fatty acids as part of her treatment. In 1998, at the age of 27, she went to the emergency department after 10 days of bloody diarrhea and lower abdominal cramping pain. She described up to 15 bowel motions daily with urgency, and she lost approximately six pounds. She was also clinically dehydrated.
After weeks of various treatments that only led to short-term results, the patient turned to omega-3 fatty acid treatments. The EPA and DHA doses were well-tolerated and had no side effects. Her bowel frequency slowly decreased, and within a week all rectal bleeding had resolved. The woman continued to take one gram of omega-3s and 2.4 grams of mesalazine, an anti-inflammatory medication that did not have the same reactions when given alone. The patient went into remission after adding omega-3s into her diet.
2. Probiotics
Is This Diet Safe
Though many health professionals suggest otherwise, its safe to follow a gluten-free diet even for people who dont necessarily need to do so.
Cutting out wheat and other gluten-containing grains or products will not cause adverse health effects as long as these products are replaced with nutritious foods.
All of the nutrients in gluten-containing grains, such as B vitamins, fiber, zinc, iron, and potassium, can easily be replaced by following a well-rounded, whole-foods-based diet consisting of vegetables, fruits, healthy fats, and nutritious protein sources.
Recommended Reading: Can You Develop Ulcerative Colitis Later In Life
Rice For Bowel Problems
Related Articles
Rice is a common staple around the world some people eat it for breakfast, lunch and dinner. Rich in nutrients and widely available, rice can help relieve a variety of bowel conditions, including constipation and diarrhea. There are two types of rices to choose from, refined or unrefined, each of which offers different potential benefits for treating bowel problems.
Seek Out A Professional
Creating a diet plan isn’t easy, which is why it’s always a good idea to get professional help. Meeting, even just once, with a dietitian, can be a revelation in terms of diet and answering that question “what do I eat?” Our understanding of IBD and diet is always evolving, so fine-tuning a flare-up diet plan is an ongoing process, and checking in with a dietitian will be helpful.
Many people with IBD restrict foods when in a flare-up, but more calories are needed to prevent losing too much weight. A physician can help you understand weight loss and how much is too much.
Don’t Miss: Best Diet For Ulcerative Colitis Flare Up
What Is White Rice
White rice is nothing but milled rice with its husk, bran, and germ removed. This process alters the flavor and appearance of the rice, thereby extending its shelf life. After milling, the rice is usually polished, giving you the shiny and bright white rice that you see in the market.
The milling process cleans the rice and removes the husks off the grains, giving us brown rice. This rice is then further polished to enhance appearance and make it more edible by removing the bran and germ as well . This polishing removes the essential nutrients vital for health.
Without the bran and the germ, the grain loses 25% of its protein and 17 other key nutrients . The processors sure add the lost nutrients back to the refined grains. But, you will be consuming processed and refined rice.
Studies show that individuals who consume white rice at least five times a week are 20% more likely to develop type 2 diabetes . One major reason people prefer white rice is that it tastes good. White rice is also quicker to cook compared to other rice varieties .
But, are these reasons justified? How bad is white rice really?
Spices Like Ginger And Turmeric Can Fight Nausea And Joint Pain
Spices such as ginger and turmeric may help fight the nausea and inflammation associated with digestive disorders such as UC, says Kennedy, noting that more research is needed to determine both the amount and best form of delivery for these benefits. As a rule of thumb, stay away from supplements. Concentrated ginger supplements could cause heartburn, diarrhea, or gas. Instead, try incorporating ginger and tumeric into soups or stir-fries. As with all diet changes, its a good idea to check with your doctor before adding ginger and tumeric to your diet.
You May Like: Treatment Of Ulcerative Colitis In Child
Creamy And Greasy Food
Creamy and greasy foods containing loads of mayonnaise, butter, cream cheese, margarine, animal fat, etc. can irritate the inner lining of the colon. This can worsen the ulcers and may cause rectal bleeding. Avoid creamy pasta, macaroni and cheese, and creamy cheese containing foods to pacify your colon.
Welcome To The Crohns & Colitis Community
This website is associated with CCFA.org and is supported by an educational grant from AbbVie.
Please read our Top 12 Rules before posting messages and sharing stories. Always be courteous and sensitive to others!
Thank you! The Crohns & Colitis Community is successful because of members like you!
Don’t Miss: Ulcerative Colitis Flare Up Treatment Guidelines
Make Screening A Priority
While eating right can help keep your colon happy, the most powerful way to prevent colon cancer is through screening. A colonoscopy is a structural examination of the colon that allows physicians to both screen for and prevent colorectal cancer.
“Colonoscopy reduces the risk of developing colon cancer because we can find precancerous polyps during the test and remove them,” Melson says. “This test is unique to most screening tests because we can actually look for precancerous growths and remove them during the procedure, which ultimately reduces a persons risk of developing colon cancer.”
If detected early, up to 95% of colorectal cancers are curable, according to the Colon Cancer Foundation. “Colon cancer is a largely treatable condition,” Melson says. “For colorectal cancer, we have a test, it is not complicated and it is extremely effective in preventing it and catching it early.
Inflammatory Bowel Disease Management

Inflammatory bowel disease is not caused, nor can it be cured, by what you eat. Doctors and dietitians agree, however, that food may play some role in the underlying inflammatory process that causes IBD symptoms.
Certain foods may aggravate symptoms, while others may calm them and promote healing. Therefore, paying attention to what you eat and how your body responds to different foods is an important component of a total treatment plan for IBD.
A diet plan can supplement but should never replace medical treatment for IBD. Always take your medications exactly as prescribed by your doctor.
Don’t Miss: Is Pepcid Good For Ulcers