Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
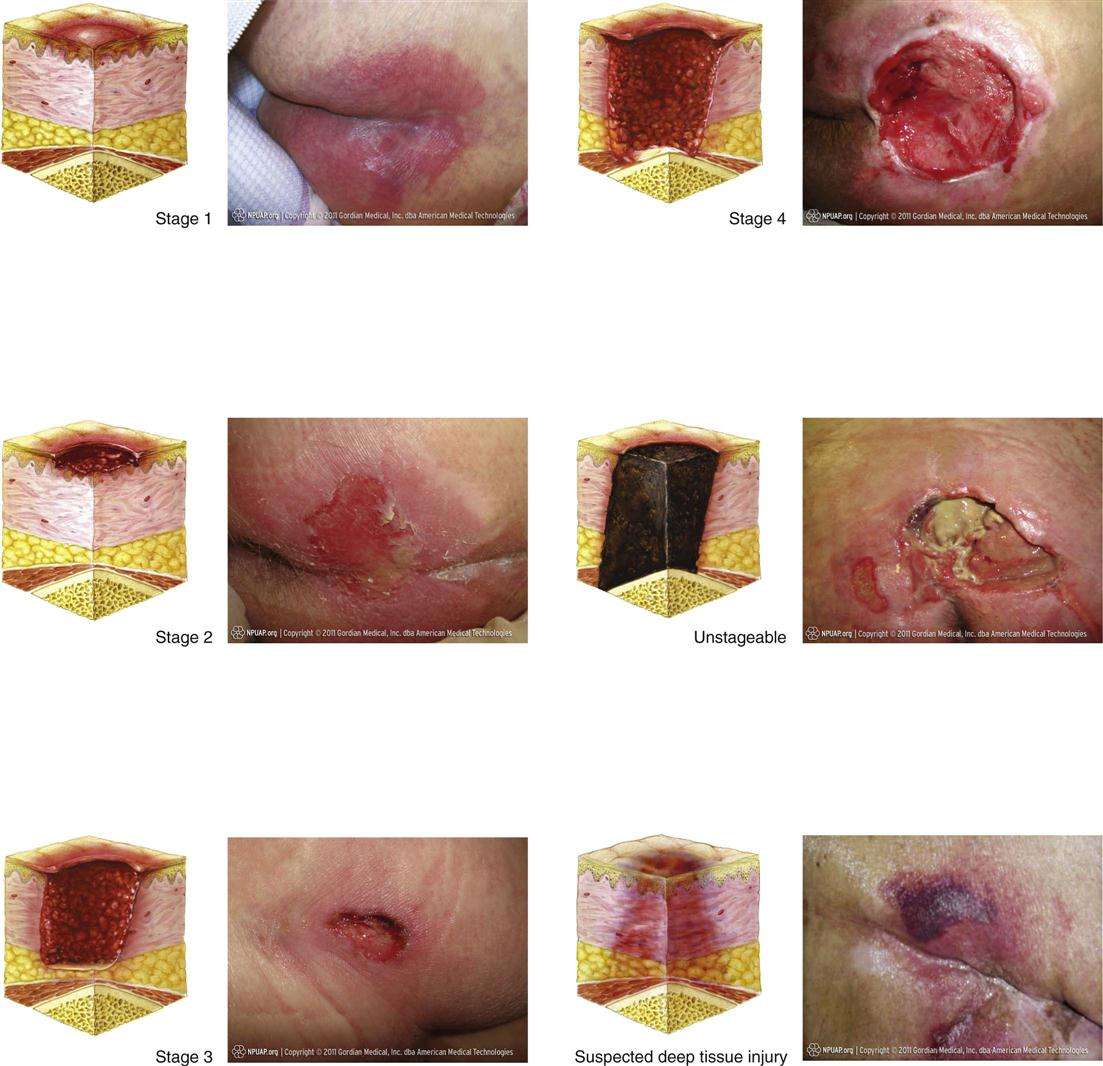
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Read Also: Ulcerative Pancolitis With Rectal Bleeding
Stage 4 Bedsore / Decubitus Ulcer
Stage 4 Bedsore is the last and most serious stage of all bedsores. In a stage 4 bed sore the patient has large-scale destruction of tissue, muscle and skin occurs. Such massive loss of tissue can also include, along with damage to muscle, bone, and even supporting structures such as tendons and joints. Stage 4 bed sores or decubitus ulcers usually require surgery to remove decayed or necrotic tissue. If aggressive treatment of a stage 4 bedsore is not taken, then further necrosis and infection can lead to septacemia, possible needed amputation and even death.
Stage 4 medical treatment include debridement, constant changing of dressing & cleansing for proper wound care, electrical stimulation and surgery. Stage 4 surgery may consist of excising of pressure ulcer, surrounding scar, bursa, soft tissue calcification, and underlying necrotic or infected bone. On deeper stage 4 bedsores and decubitus ulcers a flap surgery is needed to close the wound, fill in the dead space thus enhancing vascularity of the healing wound, and distributing pressure off the bone. All stage 4 bedsore were Stage 3 bedsores at one time, but due to the lack of quality medical and nursing care, the pressure sore continued to get worse and progressed.
Neglect is the Major Cause of a Stage 4 Bedsore
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Read Also: How Do Doctors Test For Ulcerative Colitis
The Icd Code L89 Is Used To Code Pressure Ulcer
Pressure ulcers, also known as pressure sores, bedsores and decubitus ulcers, are localized injuries to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles or the back of the cranium can be affected.
| Specialty: |
What Is A Stage 4 Bedsore
Bedsores, also called pressure sores or pressure injuries, are described in 4 stages. Staging is based on the depth of soft tissue damage. Pressure ulcer stages range from least severe to most severe .
- A stage 1 bedsore is not an open wound but it may be painful.
- At stage 2, the skin breaks open or forms an ulcer that might look like a scrape or shallow crater.
- During stage 3, the bedsore gets worse and may show fatty tissue but not muscle or bone.
- A stage 4 bedsore is very deep and muscle or bone may become exposed, causing significant risk for serious infection.
A bedsore may begin at stage 1 and advance to a stage 4 bedsore if it is not quickly treated.
Also Check: What Foods To Eat With Ulcerative Colitis
Notable Adverse Drug Reactions
- Vancomycin may be oto- and nephrotoxic it may also cause blood dyscrasias, rashes, Steven-Johnsons syndrome, toxic epidermal necrolysis muscle spasm, pain, phlebitis, vasculitis, severe hypotension and flushing of the upper body are otherpossible complications. Its use should be restricted to cases of MRSA).
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a person’s position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, it’s not always possible to prevent pressure ulcers in particularly vulnerable people.
Also Check: Can You Eat Pizza With Ulcerative Colitis
Signs And Symptoms Of Pressure Ulcer
The general clinical manifestations of pressure ulcers include:
- Unusual skin color or texture discrepancies
- Erythema or redness
- Edema or swelling in the affected area or limb
- Discharges foul in odor, can be fluid or pus-filled
- Warm or cold to touch An area of the affected region that feels different to touch than surrounding areas
- Tenderness and pain on site
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- Sepsis may occur when the body overreacts to a serious infection, such as an infection stemming from a stage 4 bedsore. The immune system gets overstimulated and attacks healthy body parts. Severe cases of sepsis can lead to septic shock, which occurs when blood pressure drops due to an infection. Septic shock can be deadly as major organs may shut down.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Also Check: What Do You Do If You Have An Ulcer
Hygiene And Wound Dressings
Practice good hygiene. For stage I ulcers, wash the area with water and mild soap, rinse well and pat the area dry gently and carefully. Do not rub forcefully on the area directly over the wound. Usually Stage I decubitus ulcers will not need to be covered.
For Stage II and III ulcers, use saline solution to clean the wound and dry it carefully. Apply either gauze dampened with saline, a hydrocolloid dressing , or a thin foam dressing such as Allevyn. The latter two dressings can be left on until they loosen or wrinkle for up to five days. If gauze is being used, the dressing should be changed twice each day and should stay damp between the times the dressing is changed. Always check to see if the ulcer is healing every time you change the dressing.
The best treatment for decubitus ulcers that are stage IV is to consult a physician for instructions. Many times these types of wounds require surgery and dressings for this kind of ulcer should be applied by a professional. A surgery called debridement is utilized to remove all dead tissue so that the wound will not become infected. Some minor debridement can be done at the bedside but larger areas need to be done in the operating room. The physician will medicate the patient because this is usually a painful procedure.
Stage 4 Decubitus Ulcers
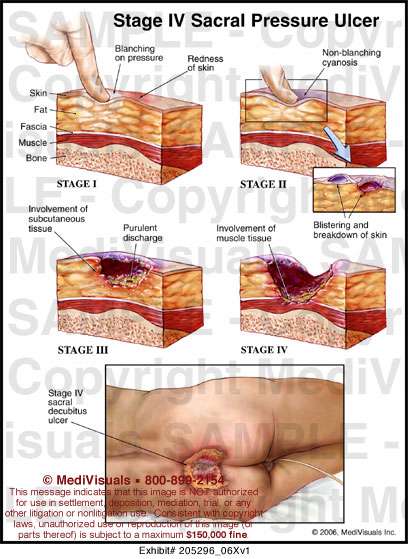
This is the most severe type of decubitus ulcer stage and has the deepest wound. Not only is the skin damaged, but joints, muscles and tendons around the skin can also be damaged and are often exposed. This deep open wound is a problem, because it leads to severe infections and diseases that can ravish the immune system of patients. Once the bone becomes infected during this stage, it can lead to death or the need for amputation.
The stages of decubitus ulcers progress quickly and must be managed before they reach stage 4. These sores are often preventable and measures must be taken to ensure that infection, death and amputation do not occur.
You May Like: Signs You Might Have An Ulcer
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Clinical Case Presentation: Pressure Ulcer Management
Thorough wound assessments and sensible product selections are essential for preventing and treating wound infections, managing exudate and finally restoring skin integrity.
This is the clinical case presentation of Fernanda Cortes from Chile who explains step by step how she treated the stage 3 pressure ulcer of a 60-year-old family father. Through her commitment and the effective combination of Prontosan®, Askina® and Linovera® the patient eventually recovered.
Please note that the pictures in the video may be disturbing to sensitive persons.
You May Like: Ulcerative Colitis Flare Up Treatment Guidelines
Read Also: Diet When You Have An Ulcer
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Stage 1 Decubitus Ulcers
These types of ulcers refer to sores where the skin is still intact, which means that an open wound is not visible. This stage is best identified with a redness color on the skin and pain to the touch. The redness color often only appears when pressure is applied, which is known as blanching. It is important to keep an eye on patients with darker skin coloring, because it is difficult to identify decubitus ulcers in this stage in these types of patients.
Recommended Reading: Arterial Ulcer Vs Venous Ulcer
Potential Biases In The Review Process
This was a sparse network and there may have been smallstudy effects which impacted on the network . The STATA routines have largely been developed for and tested on larger networks, and our work has contributed to modifications for sparse networks in the netweight routine. Other STATA routines can be modified by the user to take into account smallstudy effects, but we did not explore these approaches because there was too much uncertainty in the network for us to be confident of interpreting the results. Instead, we used the standard routines for NMA and adapted the recent approach to GRADE to bring in sparseness when assessing evidence certainty.
A further effect of the sparseness of the network may have been to hide any inconsistencies. The various statistical tests for inconsistency were generally not significant, but this may have been due to a lack of sensitivity of the tests and the wide CIs around the measures. Despite this, we found inconsistencies in the network for contrasts involving phenytoin. We cannot be sure that there are no other inconsistencies, but this may not matter given the already identified large uncertainties.
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the âcontrolâ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
Also Check: What Are The Signs Of An Ulcer In Your Stomach
Nursing Care Plan For Pressure Ulcer 1
Nursing Diagnosis: Impaired Skin Integrity related to skin breakdown secondary to pressure ulcer, as evidenced by pressure sore on the sacrum, discharge from the sores for a couple of days, pain and soreness
Desired Outcome: The patient will have optimal skin integrity by following treatment regimen for decubitus ulcers.