Tips And Tricks For Sticking With Treatment
Its important to build a healthy UC medicine habit. If youre having trouble with your medication, try these three tips to help you stay on track.
Additional reporting byJordan M. Davidson.
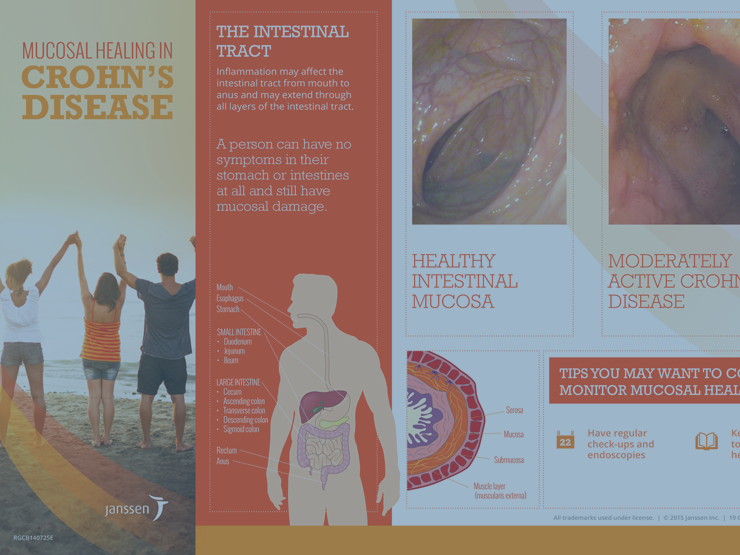
Role Of Surrogate Markers Of Mucosal Healing In Clinical Practice
A high faecal calprotectin in UC has a strong negative predictive value for remission at 6weeks and 3months, but it has yet to be shown that augmenting treatment based on the results alters outcome. In a prospective study of patients with UC who had been in clinical remission for 6months, the probability of relapse was < 10% over the next 12months in those with a basal faecal calprotectin < 150g/g. Similarly, follow-up of patients with UC in clinical remission revealed significantly higher basal faecal calprotectin levels in those who relapsed compared with those who remained in remission, while ESR and C-reactive protein failed to predict disease activity. Even if thresholds of faecal calprotectin have limited predictive value for groups of patients, faecal calprotectin is increasingly popular because it is non-invasive and individual patients can serve as their own control. The use of surrogate markers for periodic monitoring of inflammation could be quite valuable as a sensitive, non-invasive screening tool to identify asymptomatic patients who could benefit from endoscopy, if proven prospectively to have a high sensitivity for subclinical disease. Escalating treatment of patients with a rising calprotectin to prevent clinical relapse is appealing and might improve quality of life, but this is unproven and a long way from current practice.
Why Patients Stop Uc Treatment
People stop taking their ulcerative colitis medications for a number of reasons, says Phanijphand.
One of the leading reasons is the steep cost of the drugs. The out-of-pocket cost for prescription medicines can run over $2,000 per year, while the cost of UC care in general can run from roughly $15,000 to $25,000 per year, according to a study published in Inflammatory Bowel Diseases in January 2020.
The study also found that patients using biologics had the highest costs. Treating UC with corticosteroids had higher costs than with nonsteroidal anti-inflammatory drugs, but the latter groups costs rose more over time.
Also, when a person feels better, they may decide they no longer need UC medicine.
“Some patients think that once their symptoms are gone, they can stop taking their meds,” Phanijphand says. “They believe they’re cured or that they may have been misdiagnosed.”
Also Check: Does Smoking Cause Ulcers After Gastric Bypass
Common Mistakes That Can Make Ulcerative Colitis Worse
The good news: Theyre easy to avoid.
When you live with ulcerative colitis , you know that symptoms can return even if youve been in remissionand even if youre doing everything you can to avoid a flare. Yet there are a number of missteps you might not even realize youre making that can worsen your condition, says Matilda Hagan, M.D., co-director for the Center for Inflammatory Bowel and Colorectal Diseases at Mercy Medical Center in Baltimore.
While so much of how your ulcerative colitis plays out is largely out of your control, there are a handful of mistakes many patients make that can easily be avoided, she says. Here are five of the most commonaccording to Dr. Hagan and gastroenterologist Raj Devarajan, M.D., president of the Massachusetts Gastroenterology Association:
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Read Also: Pressure Ulcer Prevention Care Plan
Clinical Remission Generally Means No Symptoms
When the symptoms of UC are gone , thats considered clinical remission, explains Steve Serrao, Ph.D., the division chief in gastroenterology at Riverside University Health System in Moreno Valley, CA. Gastroenterology societies use guides such as the Simple Clinical Colitis Activity Index to gauge UC activity, and doctors also recommend using a stool/food diary to log symptoms. Check out apps like mySymptoms Food Diary to help you collect this information.
Definitions Of Remission Used In Current Guidelines
All guidelines discuss disease remission, but not all are explicit in their definition, which compromises their utility. The World Gastroenterology Organisation Global Guidelines define remission as a UC-DAI2, which implies modest control of symptoms. By contrast, both the European Crohns and Colitis Organisation , and the International Organisation for the study of IBD define it as complete resolution of symptoms and endoscopic mucosal healing. Nevertheless, neither the Practice Parameters Committee of the American College of Gastroenterology nor British Society of Gastroenterology defines remission.
Recommended Reading: Stage 2 Pressure Ulcer Treatment Cream
Will My Uc Symptoms Come Back
Because UC is a chronic disease, its possible that you could have a flare-up in the future, even after a long period in remission. And even if you stay in remission, you might still have symptoms like diarrhea, abdominal pain, or fatigue from time to time. It can be difficult to tell whether these symptoms are caused by UC, or whether theyre caused by something else, like irritable bowel syndrome , an infection, small intestinal bacterial overgrowth, or even dietary changes, Dr. Chang says. If you do experience any symptoms, you should discuss them with your doctor.
Not Talking To Your Doctor Before Starting A New Diet Or Taking Supplements
Are you considering trying a new way of eating or starting a new regimen of vitamins and minerals? While it may be just fine , Dr. Hagan says its important to run it by your doctor first. I love it when my patients come to me and say, Hey, my girlfriend told me this supplement is great for a healthy immune system and I want to take it, she says. This gives me a chance to take a look at the supplement, along with the other medications that the patient is on, so I can make sure nothing will interact.
As for diet changes, most foods are OK for colitis patients because colitis mainly affects the large intestine. By the time food gets there, youve gotten what you need out of your food and your body is just eliminating the rest, Hagan says. That said, its still a good idea to clue your doctor into any big changes in your go-to diet. For example, if youre taking an immunosuppressant drug, youll want to avoid eating anything unpasteurized, says Dr. Hagan. Think of it as a great opportunity for you and your doctor to touch base and make sure your lifestyle choices are supporting your treatment plan.
Recommended Reading: How Do They Check For Ulcers
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
You May Like: Stage 2 Pressure Ulcer Treatment Dressing
I Remembered What It Was To Have A Life Again
Mary Elizabeth Ulliman, 33, was diagnosed with ulcerative colitis in 2011 and says she was fatigued and made constant trips to the bathroom. But in 2015, Ulliman started taking two new medications that greatly improved her symptoms.
After a few months, I started noticing differences, she tells SELF. By 2016 my quality of life had done a complete 180 from where I’d been since 2011, she says. In the thick of my ulcerative colitis journey, I genuinely forgot how much fun life could be. I was slogging through, day after day, thinking that feeling miserable was how it was going to be forever, willing myself to make it through work days so I wouldn’t lose my job and insurance.
Remission, she says, allowed her to live fully again. Suddenly, life wasn’t made up of sleeping, bathroom trips, forcing myself to eat, and willing myself to not fall asleep at my desk at work, she says. I had some extra energy. I startedhesitant, at firstto exercise. I could eat food without immediately regretting it afterward. I could have a glass of wine now and again. I had the wherewithal to do activities after workcoaching, going to a happy hour, taking my dog to play. I remembered what it was to have a life again.
Ulliman wants other ulcerative colitis patients to have hope. When you’re in the black hole that is trying to find somethinganything that will work to control your it can be easy to forget how much fun and joy life can bring you, she says. Mary Elizabeth Ulliman
Related:
Oral Fecal Microbiota Transplantation Induces Maintains Remission In Ulcerative Colitis
Disclosures: We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Oral lyophilized fecal microbiota transplantation following antibiotic use induced and maintained remission in patients with active ulcerative colitis, according to research published in Lancet Gastroenterology and Hepatology.
FMT delivered via colonoscopic infusion and enemas induces clinical remission in 24% to 47% of patients with active ulcerative colitis. However, this route of administration is invasive, poorly tolerated and logistically difficult due to storage and transport requirements,Craig Haifer, MBBS, FRACP, of the University of Sydneys Concord Clinical School and the departments of gastroenterology at Concord Repatriation General Hospital and St. Vincents Hospital, and colleagues wrote. Orally administered FMT has similar efficacy to FMT delivered via colonoscopy in the treatment of recurrent or refractory Clostridioides difficile colitis although it remains unclear whether it has clinical efficacy in ulcerative colitis.
According to study results, 53% of patients in the FMT group and 15% of patients in the placebo group achieved the primary endpoint . Further, 73% and 25% of patients achieved corticosteroid-free clinical remission and 47% and 15% of patients achieved corticosteroid-free endoscopic remission . Haifer and colleagues noted no significant difference in endoscopic response or clinical response .
Read Also: What Not To Eat With Bleeding Ulcers
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
What Is Remission Exactly
During remission, UC symptoms improve. But remission itself is difficult to define, says Shannon Chang, M.D., a gastroenterologist at NYU Langones Inflammatory Bowel Disease Center in New York City. For starters, there are three different types: clinical, endoscopic, and histologic remission. We’re going to look at each one.
Don’t Miss: L Glutamine Ulcerative Colitis Dosage
Can I Stop Taking My Meds In Deep Remission
In a word: no. The key to remaining in remission is sticking to your recommended treatment plan. A study published in PLoS One found that people in remission who stopped taking their meds were five times more likely to relapse. Treatments that may help achieve or maintain UC remission include aminosalicylates, drugs that reduce inflammation in the lining of the colon, and immunomodulators, meds that modify the immune system in order to decrease the bodys inflammatory response. All treatments come with potential side effects, and it can take time to find the one that works best for you.
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Recommended Reading: How Do You Heal Leg Ulcers
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Different Types Of Remission
There isn’t a consensus about the exact definition of remission in IBD. Different gastroenterologists and IBD centers might use different criteria. There are, however, several scoring tools that your healthcare provider might use to determine if you’ve achieved remission.
Some of the types of remission include:
- Biochemical remission: Laboratory tests done on the blood or the stool don’t show any of the hallmark signs of IBD.
- Clinical remission: When the symptoms of IBD have lessened to the point that they’re mostly absent or gone.
- Endoscopic remission: No inflammation is seen during a colonoscopy or a sigmoidoscopy when your healthcare provider can see the lining of your digestive tract
- Histologic remission: When a biopsy is taken and examined, no inflammation is seen.
- Surgical remission: Surgery can also bring about a time of remission for some people with IBD when it leads to substantially reduced inflammation or symptoms.
Also Check: Support Surfaces For Pressure Ulcer Prevention
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.