Pressure Sore Risk Areas
A pressure ulcer is injury to skin or tissue that occurs when blood circulation is decreased because of pressure to a specific area. At first, a slight reddening of the area can be detected. This is referred to as the initial sign of tissue damage.
The sacrum, heels, elbows and shoulder blades are particularly prone to pressure ulcers. In the current medical environment since the outbreak of COVID-19, the face is also extremely at risk of developing pressure ulcers, because health care professionals need to wear personal protective equipment and critical COVID-19 patients are exposed to medical devices related to non-invasive mechanical ventilation.
Causes And Prevention Of Pressure Sores
Pressure sores are wounds that develop when constant pressure or friction on one area of the body damages the skin. Constant pressure on an area of skin stops blood flowing normally, so the cells die and the skin breaks down.
Other names for pressure sores are bedsores, pressure ulcers and decubitus ulcers.
Get A Proper Seating Evaluation At Least Every Two Years Or Sooner If Your Health Or Skin Condition Changes
- Make sure you have the proper cushion for your wheelchair and your seating tolerance.
- Make sure you have the appropriate wheelchair, one that has been measured specifically for you and is compatible with your level of mobility, activities, work and associated equipment.
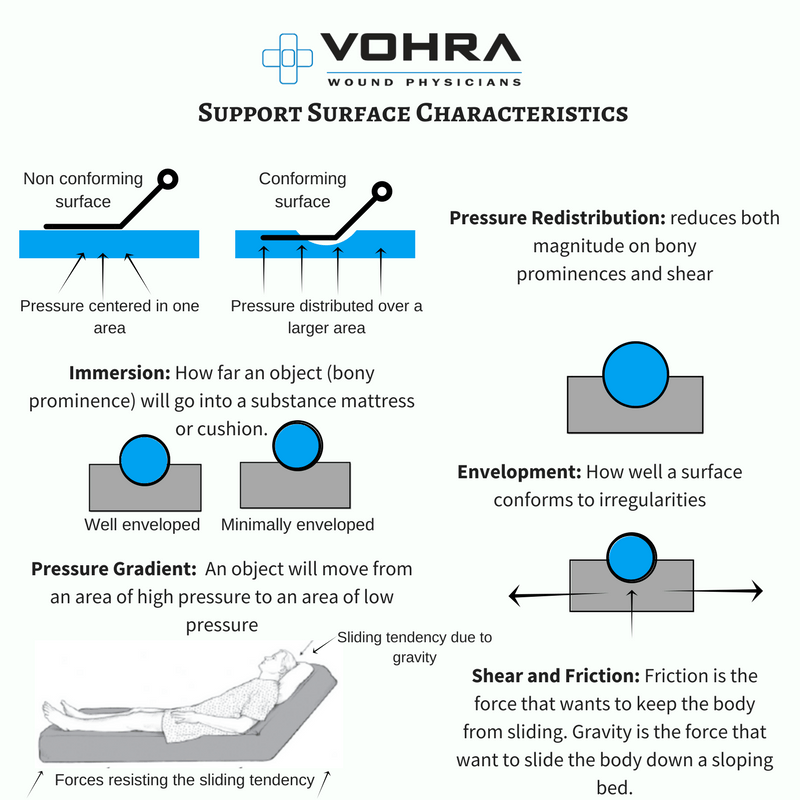
- The therapist doing the seating evaluation should place a pressure map above your cushion and under your buttocks to see where your pressure-sensitive areas are. If at-risk areas on the pressure map are found, then the therapist may try a different cushion alter the wheelchair seat, back or foot rest or show you how to relieve pressure on the vulnerable areas by repositioning your body.
- Pressure mapping is an excellent way to visually demonstrate the effectiveness of weight shifts.
- If pressure mapping is unavailable, work with a seating professional and try several different cushions to see what works best for you.
You May Like: How Long Does An Ulcerative Colitis Flare Up Last
Causes Of Pressure Ulcers
Pressure ulcers are caused by sustained pressure being placed on a particular part of the body.
This pressure interrupts the blood supply to the affected area of skin. Blood contains oxygen and other nutrients that are needed to help keep tissue healthy. Without a constant blood supply, tissue is damaged and will eventually die.
The lack of blood supply also means that the skin no longer receives infection-fighting white blood cells. Once an ulcer has developed, it can become infected by bacteria.
People with normal mobility do not develop pressure ulcers, as their body automatically makes hundreds of regular movements that prevent pressure building up on any part of their body.
For example, you may think that you are lying still when asleep, but you may shift position up to 20 times a night.
Pressure ulcers can be caused by:
- pressure from a hard surface such as a bed or wheelchair
- pressure that is placed on the skin through involuntary muscle movements such as muscle spasms
- moisture which can break down the outer layer of the skin
The time it takes for a pressure ulcer to form will depend on:
- the amount of pressure
- how vulnerable a person’s skin is to damage
Grade 3 or 4 pressure ulcers can develop quickly. For example, in susceptible people, a full-thickness pressure ulcer can sometimes develop in just 1 or 2 hours. However, in some cases, the damage will only become apparent a few days after the injury has occurred.
What Are Skin Ulcers

A skin ulcer is a sore shaped like a crater that appears on the skin. Essentially, skin ulcers are open wounds on your skin that havent healed properly. You can get a skin ulcer from an injury, poor blood circulation, or continuous pressure on the area. The most common area for skin ulcers to develop is on the legs. Its estimated that three out of 1,000 people have active leg ulcers.
Skin ulcers can also show up on your back, hips, and feet. Skin ulcers are most common in older people. Skin ulcer treatment, symptoms, and recovery will depend on the specific cause of your skin ulcer.
Some skin ulcers are painful, but not all are. Someone with a skin ulcer may have a swollen leg and feel an itching or burning sensation.
Additional possible symptoms of skin ulcers include:
- Rash
- Swelling of the skin near the ulcer
- Pain or tenderness near the skin ulcer
- Bloody, clear, or pus-filled discharge from the ulcer
- Hair loss near the skin ulcer
- A bad smell from the area around the ulcer
The most frequent types of foot and leg ulcers include:
- Arterial
- Neurotrophic
- Venous stasis ulcers
Skin ulcers are usually defined by the ulcers location, appearance, and how the skin around the ulcer looks.
Recommended Reading: Foods To Avoid With Peptic Ulcer
Health Care Professional Take Care Of Your Skin
The effectiveness of using personal protective equipment , such as face masks, goggles and gloves, especially in times of COVID-19 is well known and uncontroversial.
But how can you avoid skin lesions, pressure ulcers or friction injuries, that may be painful as well as a dangerous entryway for bacterial infections, too.
We have gathered useful recommendations for you:
What Increases The Risk Of Developing Pressure Ulcers
People who are confined to a bed or chair for example due to stroke, spinal injury or dementia are at greater risk of developing extensive pressure ulcers. Other risk factors include:
- immobility being confined to bed after an illness or surgery, or due to paralysis
- diabetes and other health conditions that can affect blood supply
Also Check: What To Do When You Have A Stomach Ulcer
Use Specialty Bedding Or Materials To Reduce Pressure
Depending on the needs of each senior, specialty beds, such as water or air mattress toppers, or special, cushioned padding, such as heel protectors, may be needed to reduce the amount of pressure placed on sensitive areas of the body. These additional materials should not be limited to mattresses or modifications to footwear. Instead, keep the options open for what may and may not be the most comfortable and beneficial to the needs of seniors.
For example, a memory-foam pillow is great, but it does little good if it is always placed in the same position. Furthermore, soft, pillow-like wedges may be used to help seniors remain on their sides while lying in bed between repositioning times.
Some newer beds may suggest automatic turning is available for use. However, these systems do not completely reposition a person. As a result, it is best to use these systems in conjunction with manually reposition of a person.
What Role Do Diet And Skin Care Play
Some people who are hardly able to move don’t get very hungry or thirsty. In order for them to stay in good physical condition, though, it’s important to make sure they get enough to eat and drink. Eating too little or a very unbalanced diet and hardly having anything to drink may weaken their skin even more. Some people take dietary supplements, but there’s hardly any research on whether these products can help prevent pressure ulcers.
It’s important to keep the skin from getting too dry, but also to prevent it from being exposed to constant moisture either one increases the likelihood of damage to the skin. There’s not yet enough good research to be able to say whether regular use of creams or lotions can prevent pressure ulcers.
You May Like: Indian Diet For Ulcerative Colitis
How Often Is Repositioning Necessary
Even though it’s often recommended that people be repositioned every two hours, there’s no single recommendation that works for everyone. Some people can lie in the same position for quite a long time without getting ulcers, while others need to switch much more often. Research has not yet found out how often someone should change position to get the best preventive effect.
Unnecessarily moving someone too much for no good reason can also have disadvantages. For instance, repositioning every two hours at night may wake the person each time and keep them from getting a good nights sleep. Changing position can also be very painful for people who have wounds or joint conditions. Frequent repositioning is physically demanding for caregivers or family members too. It’s therefore important to observe how often someones position really needs to be shifted. It can then help to make a note every time they are repositioned.
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Also Check: What Foods Can I Eat If I Have An Ulcer
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Home Remedies For Skin Ulcers
Foot and leg ulcers
It is possible to use a home remedy for ulcers. Since skin sores are most commonly found on the legs and feet, treatment for skin ulcers often begins with skin and foot care. Its important to examine your skin and feet often, especially if you have diabetes. Detecting skin ulcers early can help prevent infections and stop the skin sores from getting worse.
If you have a foot or leg ulcer, its essential to wash the affected area around the ulcer every day with lukewarm water and mild soap. By cleaning the area, you loosen and remove dead skin, drainage, and debris from the infected area. After washing, make sure to dry all the areas thoroughly, including between the toes. Avoid rubbing your skin too much.
Inspect your legs and feet every day. Specifically, look for signs of scratches, cracks, cuts, blisters, and other sores. Also watch out for redness, ingrown toenails, corns, increased warmth in the area, or calluses. If necessary, use a mirror to inspect the entire area or ask a loved one to help you look.
Once or twice a day, apply a cream to your legs and the soles and tops of your feet. Make sure its a lanolin-based cream, which helps prevent dryness and cracking skin. Dont apply the lotion to areas where there is an open sore or cut. Additionally, dont apply lotion between your toes. If your skin is extremely dry, use a moisturizing cream more often.
Home remedies for ulcer and wound treatment
You May Like: What Is A Gastric Ulcer And What Is Its Cause
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
Don’t Miss: How To Cure Ulcerative Proctitis
Causes Of Pressure Sores
Pressure sores happen if you cant move around and so stay in one position for a long time. We normally move about constantly, even in our sleep. This stops pressure sores developing.
People who are unable to move around tend to put pressure on the same areas of the body for a long time. If you are ill, bedridden or in a wheelchair, you are at risk of getting pressure sores.
A number of things can increase your risk of pressure sores, including:
- being unable to move around easily due to old age or illness
- weight loss – you may have less padding over bony areas
- sliding down in a bed or chair – pressure on the skin cuts off blood supply because the skin is being pulled in different directions
- friction or rubbing of the skin, for example against sheets
- a poor diet
- moist skin – for example, due to sweating or incontinence
- other medical conditions, such as diabetes
- having a previous pressure ulcer
Pressure Ulcers And Diet: Food Fact Sheet
Pressure ulcers occur when the skin and surrounding tissue is damaged by medical devices or the weight of the body pressing down. This restricts blood flow and the delivery of oxygen and nutrients to the area. They often develop where bones are close to the skin such as on the lower back/spine, hips, heels and elbows. Having a poor nutrient and fluid intake can increase the risk of pressure ulcers.
The risk increases in those who are underweight or overweight. Maintaining a healthy weight and eating a balanced diet can reduce the risk of developing pressure ulcers.
This is because:
- Being overweight can reduce mobility and increase the weight bearing load through pressure areas such as the bottom.
- Being underweight can mean there is less natural padding on bony areas such as the bottom and hips.
- The skin needs a good supply of fluid and nutrients to maintain its circulation and keep it supple.
Don’t Miss: Support Surfaces For Pressure Ulcer Prevention
Symptoms Of Skin Ulcers
Skin ulcers begin with redness, swelling, and tenderness around your skin. Some ulcers may feel painful and have a buildup of fluids in the sores. These may also cause bleeding of the skin and in rare cases, you may have fever.
Other common symptoms include deviation from normal skin structure, discoloured skin, itchiness, pus, and skin irritation. There may also be a foul smell in the affected area.
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Don’t Miss: How To Test For Ulcerative Colitis
Use Devices To Relieve Pressure
- Use a foam, gel, or air cushion or mattress to relieve pressure. Ask your healthcare provider which is best. Avoid donut-shape cushions because they reduce blood flow and cause tissue to swell, which can increase the risk of getting a pressure ulcer.
- The head of the bed should be raised as little and for as short a time as possible depending on the medical condition. When the head of the bed is raised more than 30, skin may slide over the bed surface, damaging skin and tiny blood vessels.
- Use pillows or wedges to keep knees or ankles from touching each other. If completely immobile, put pillows under the legs from mid-calf to ankle to keep the heels off the bed.
When To Call A Healthcare Provider
If the ulcer is large or deep, growing in size, incredibly painful, or if you have any signs of infection , you notice a bad smell coming from your ulcer, or you’re running a fever, call your healthcare provider right away.
You’ll also want to call your healthcare provider if your ulcer, no matter how minor, isn’t showing signs healing after a week to 10 days.
In most cases, the ulcer will be dressed to protect the wound. However, if your ulcer is draining considerably, your healthcare provider may recommend leaving the wound uncovered. Dressing the ulcer if it’s draining considerably can impede healing.
If your ulcer is painful, pain medication can be prescribed. Antibiotics may also be prescribed either prophylactically to prevent infection or to treat an already infected wound.
Debridement is done to remove dead tissue from more serious ulcers. For deep ulcers or those that aren’t healing after a long period of time, skin grafts may be needed. In the most severe cases, part of the foot, leg, or other appendage may have to be amputated.
Restoring good circulation is key in treating and preventing ulcers. This includes elevating the legs, wearing compression stockings, reducing pressure on ulcer-prone areas, superficial vein surgery. Leg ulcers, in particular, are incredibly likely to reoccur, so compression stockings are often needed to be worn for life.
Recommended Reading: History Of Ulcerative Colitis Icd 10