Interaction Between Stress And Ibd
In the 1950s, IBD was considered a psychosomatic disorder , and previous studies have demonstrated a close association between IBD and stress. Specifically, IBD patients are often exposed to stress, which induces mood swings or even leads to mental complications. Meanwhile, increased emotional disorders can exacerbate symptoms such as abdominal pain, and can enhance the severity of IBD in turn.
Where To Get Help
Speaking with your doctor is the first step you should take to get help for anxiety or depression associated with UC.
Treatment may include adjusting your medication to better control inflammation. Your doctor may also prescribe an antidepressant or anti-anxiety medication to improve your mood.
They may also recommend therapy with a mental health professional. These sessions can supply you with coping methods and stress management skills. Youll also learn how to change your thinking patterns and dispel negative thoughts that worsen depression.
In addition to conventional therapy, home remedies and lifestyle changes may help improve your mental health.
Examples of healthy lifestyle changes include:
- avoiding alcohol or drugs
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Don’t Miss: What Causes Venous Stasis Ulcers
How Stress Messes With Your Immune Response
If you are living with UC, stress talk gets elevated to a whole new level. Thats because UC is an inflammatory bowel disease that already causes inflammation in your digestive tract. So when you are experiencing stress, it can trigger even more inflammation in your body, leading to a worsening of UC symptoms. Stress affects UC as it would any chronic illness, says Loren Brook, M.D., a gastroenterologist at the University of Cincinnati College of Medicine in Ohio. Stress may increase your chances of flares and is known to weaken the immune system.
When you are stressed, the increase in cortisol can increase the pro-inflammatory cytokines and therefore cause increases in inflammation of the gut which has a negative effect on UC, says Bottoms. This also means your general immune system is not as effective and may struggle to fight against other illnesses as well.
Fatigue In Children With Ulcerative Colitis
In a 2019 study , researchers looked at how children with ulcerative colitis experienced fatigue.
They found that, like adults, children with the condition can experience high levels of fatigue. They noted the following potential reasons for this:
- disease activity level
According to the Crohns and Colitis Foundation, fatigue is a common issue among people with IBD. It affects 80% of people with active IBD and 50% of people in clinical remission.
Despite the frequency of fatigue in IBD, researchers have indicated that it is often underreported and undertreated. They have noted that doctors often do not treat fatigue because of the subjective nature of the condition.
People with fatigue should talk with a doctor and make sure that they understand how much fatigue affects their life. The more information a person can provide about their symptoms, the more likely the doctor is to understand fatigue as a serious symptom and make recommendations for treatment.
In addition to taking steps to manage and treat ulcerative colitis, a person can make certain lifestyle changes to help reduce fatigue.
Some potential ways for a person to improve fatigue and boost energy levels include:
In one 2020 study , researchers found that the best way to treat fatigue is to treat its underlying causes.
Also Check: What To Take For Stomach Ulcer Pain
The Impact Of Stress On Ibd
Life always includes stresses which change over time. In adulthood, stress mainly originates from family, work, economic status, and major life-threatening events. Early life and childhood exposure to antibiotics, vaccination, diet, smoke, and psychosocial stress seems to lead to a long-term adverse influence throughout life. The stressors of the above different periods may increase adulthood susceptibility to diabetes, cardiovascular disease, autoimmune disease, stroke, and certain cancers .
Stress and the Risk of IBD Onset
A Manitoba IBD cohort study in Canada ascertained the first onset of psychotic symptoms via a structured diagnostic interview. The report showed that approximately two-thirds of patients who had both anxiety disorder and IBD actually developed psychiatric symptoms predating the IBD diagnosis by over 2 years. This more than 2-year time interval for diagnosis was also present in more than half of IBD patients with mood disorders. Moreover, IBD patients with lifelong anxiety or mood disorders displayed an earlier onset of IBD symptoms than those without the above disorders, and there was a tendency for an early diagnosis of IBD . These results reminded us of the potential interactions between IBD and psychiatric diseases. It is possible that the existence of these psychiatric illnesses may increase the susceptibility of individuals to IBD.
Effect of Stress on IBD Course
Effect of Stress on IBD Prognosis
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you havent been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If youve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you cant contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Read Also: How To Treat And Ulcer
Can Stress Cause Ulcerative Colitis
Stress wont cause you to get ulcerative colitis. However, it may bring on a disease flare-up or make existing symptoms worse if you have the disease. When you have a flare-up, it means you have active symptoms.
Research shows a distinct gut-brain connection, meaning how you feel mentally can affect how you feel physically. For people with ulcerative colitis, anxiety and stress may cause more frequent or severe bouts of diarrhea. Stress also can intensify pain signals, making abdominal cramps worse.
Life stressors dont have to be major to bring on ulcerative colitis symptoms. Everyday life stressors can add up, too. Active ulcerative colitis symptoms may add to your stress levels. Thats why its important to strive every day to find healthy ways to manage stress like exercising, journaling, or meditating.
Recommended Reading: Does Stress Increase Blood Sugar
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications arent effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen , or used to create an internal pouch thats connected to your anus .
Read more about:
Also Check: How To Stop Stress Headaches
Recommended Reading: Bleeding Ulcer Blood In Stool
Response To Acute Stress In The Presence Of Chronic Stress
The physiological and immune response to acute experimental stress is exaggerated by the presence of chronic psychological stress . Individuals with high chronic stress levels, such as those caring for a long term dependent or women with a strong family history of breast cancer, showed greater and more prolonged increases in sympathetic activation in response to acute stressors than controls. This was associated with a greater increase in NK cell numbers, albeit with an attenuated increase in their activity, in the chronically stressed subjects than in controls.
Table 1
Summary of the effects of adverse life events and acute experimental stress on systemic immune and inflammatory function in humans
Talk To A Professional
Lawrence S. Gaines, PhD, a clinical psychologist at the Vanderbilt Inflammatory Bowel Disease Clinic in Nashville, Tennessee, says that working with a therapist or other mental health provider is an important part of managing ulcerative colitis. Cleasby agrees.
I think the most important way to deal with anxiety and depression is to speak out about it. It’s easy to feel so alone and that no one will understand you, but actually just voicing your fears takes away some of their power.
Petrik recommends cognitive behavioral therapy , a type of talk therapy that helps patients develop skills to cope with emotional challenges, like those associated with UC. Acceptance and commitment therapy is a type of CBT that helps people who suffer from a chronic illness manage their symptom-related anxiety. One study, published online in March 2019 in the journal Gastroenterology, found that two months of ACT reduced stress and anxiety levels in people who suffer from IBD by 45 percent after 20 weeks.
Petrik says to ask your doctor if there is a mental health provider on staff, or if your doctor can recommend a therapist that specializes in chronic illness or IBD. Psychology Today also maintains a searchable database of verified mental health providers across the United States. A therapist can help determine whether or not anxiety medication is a good fit for you.
Don’t Miss: How To Lose Weight With Stomach Ulcers
Gut Microbiota Is Responsible For The Susceptibility Of Dss Colitis To Chronic Stress
To probe if the changed gut microbiota triggered the deleterious effect of stress, we took advantage of the transmissible nature of the gut microbiota to determine whether susceptibility to DSS could be enhanced in normal mice by cohousing them with stressed mice. PCoA revealed an equilibrated colon microbial landscape in cohoused mice . The abundance of some inflammation-promoting OTUs related to Streptococcus and E. faecalis were increased in the DSS group after cohousing . The composition of microbiota at the phyla and genus levels after cohousing are shown in Fig. S5. Interestingly, even though the weight of mice in the separately housed stress group was significantly lower than in the normal separately housed group, no appreciable differences were seen in mouse weights between normal cohoused and stressed cohoused groups . We also observed significant decrease in colon length and body weight and significant increase of bleeding score in DSS cohoused mice compared with DSS separately housed mice, indicating that the transferred gut microbiota from stressed mice to nonstressed mice by cohousing contributes to more severe colitis. Consistent with these findings, the effect of stress on the immune system was compromised by cohousing, as differences in thymus coefficient, MLN coefficient, WBC count, and proportion of MLN-associated immune cells disappeared between cohoused groups.
Coffee Enemas To Clear The Colon
Compared to colonics, enemas are done at your home in private. They are inexpensive compared to a more costly visit to your colon hydrotherapist. You can buy kits at any drugs store or online. Here is a great stainless steel kit that I recommend.
Enemas also work by cleansing your colons with water. In some cases, coffee, wheatgrass, herbs, or apple cider vinegar is added for extra cleansing. While colonics target your entire intestine, enemas are targeting your descending colon only. Here is a helpful article on how to do a coffee enema.
If you choose to get a colonic or try an enema yourself, it is important that you take probiotics to support your healthy gut flora. Colonics clean your colon from waste, toxins, bacteria, fungi, and parasites. However, they also clean out good bacteria in the process.
Taking high-quality probiotics and eating a nutrient-dense, gut-supporting diet is important to achieve long-term results. Continue reading for further tips on how to reset your microbiome after a colon cleanse.
Also Check: Stage 4 Decubitus Ulcer Treatment
Recommended Reading: How Does Ulcerative Colitis Affect The Digestive System
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
What Causes Ulcerative Colitis Plus How To Treat It
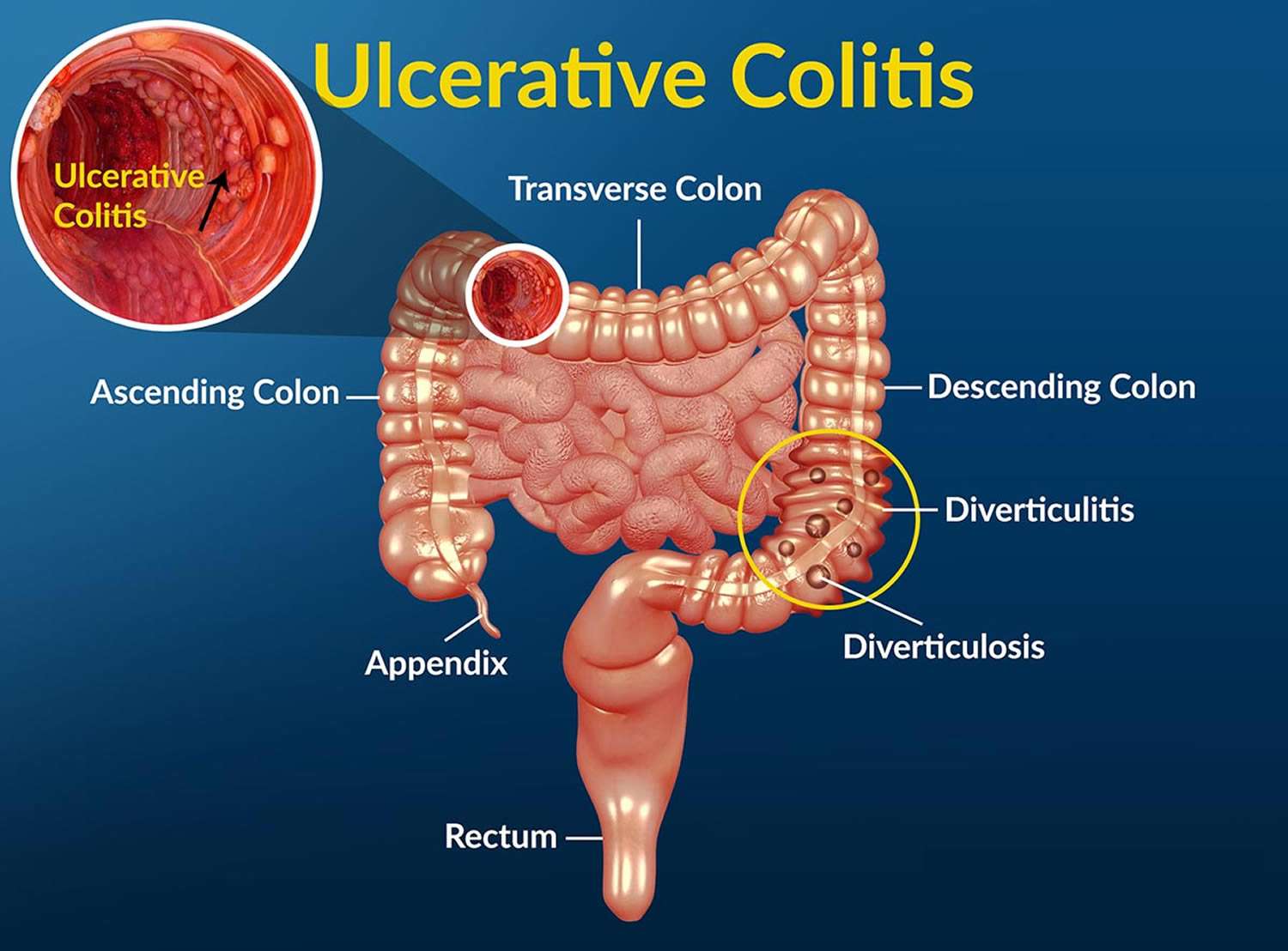
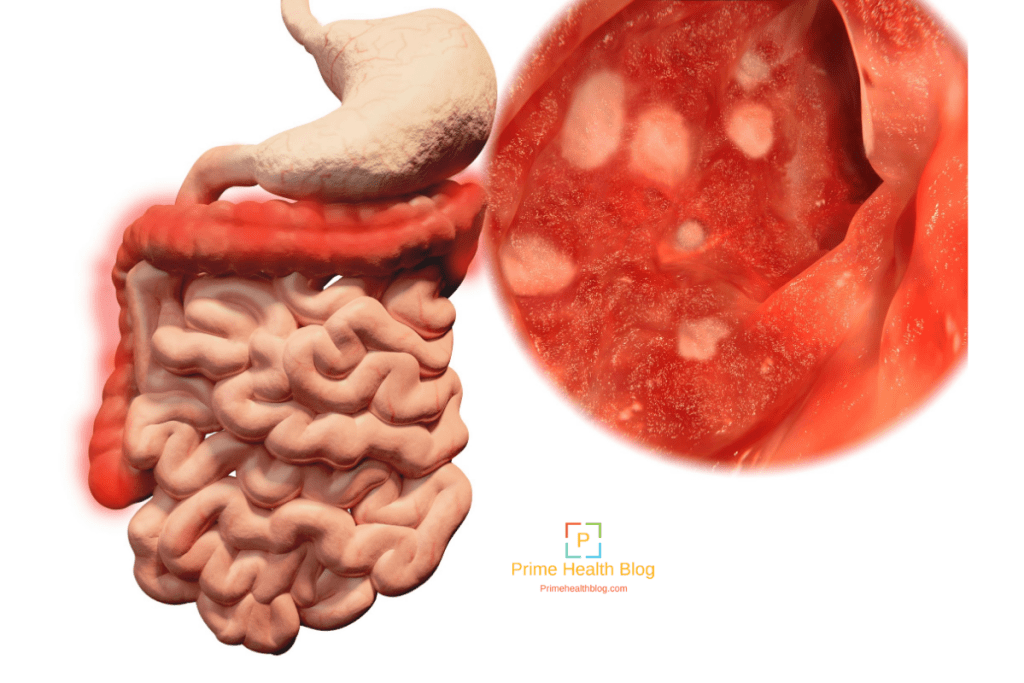
- Ulcerative colitis is a type of inflammatory bowel disease that develops when your colon or rectum become inflamed.
- UC affects about 900,000 individuals in the U.S.
- The exact cause of ulcerative colitis is complex but experts believe it could be caused by an overactive immune system.
- Even though there is no cure, there are treatment options available that can help you manage the disease.
Do you need to take frequent trips to the bathroom? Perhaps youre suddenly feeling overly tired every day or experiencing unusual abdominal pain or cramping. If thats the case, you might be suffering from a type of inflammatory bowel disease known as ulcerative colitis.
Related Topics :
Roughly 900,000 individuals are living with ulcerative colitis in the United States. And while it often develops between the ages of 15 and 30, anyone can develop it at any age. Theres a lot more to know about it too. So, lets take a look at what ulcerative colitis is, what causes it, the signs to look out for, plus how to treat it.
Read Also: What’s Good For An Ulcer In Stomach
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
What To Feed A Dog With Diarrhea From Colitis
If your veterinarian has confirmed the diarrhea is from colitis, he or she will likely recommend an easy-on-the-gut diet for a period of time.
Drugs that suppress diarrhea dont solve long-term problems, so its in your dogs best interest to figure out what caused the problem.
Knowing what caused your Cocker Spaniels colitis will help prevent it in the future. However, if food is the culprit, an acute condition can become chronic. Think about a new car that you fill up with the wrong type of gasoline. Sooner or later, things will break down.
I fed Dexter boiled lean organic ground beef and gave it in small quantities several times a day with boiled white rice, again in small quantities.
As we eased back into regular food, I added Dr. Harveys Canine Health to his lean organic ground beef, which I continued to boil for a week. A lot of dogs develop hypersensitivity to dog food, so I took great comfort in feeding Dexter his normal food as his gut healed.
Dogs who relapse after antibiotics stop may find themselves in a vicious cycle. I know because my first Cocker Spaniel succumbed to complications of IBD. If the colitis returns, your dog may need further testing like x-rays, a scan, or even a colonoscopy.
Read Also: Wheatgrass Spray For Leg Ulcers
Psychological Stress And Gastrointestinal Motility And Water And Ion Secretion
As in humans, acute stress in the form of restraint stress, loud noise, inescapable foot shock, or water avoidance all increase colonic motility and defecation in the rodent. The mechanisms for these changes involve CRF and its receptors .
Similar alterations in ion and water transport to those seen in humans are also well described in animals in response to psychological stress. Increases in gastrointestinal water and chloride ion secretion occur in response to restraint stress in the rat. It is now recognised that, as with changes in intestinal permeability, this secretory response is related to both cholinergic nerves and mast cells as it was increased in cholinesterase deficient Wistar-Kyoto rats, blocked by pretreatment with atropine, and absent in mast cell deficient rats. Restraint stress also increased colonic mucus secretion in ex vivo colonic segments and in vivo, as measured by histological goblet cell depletion. This effect could also be reproduced by peripheral CRF administration and inhibited by mast cell stabilisers.
Manage Your Anxiety Manage Your Colitis
Managing symptoms of psychological stress and anxiety, unfortunately, won’t cure your ulcerative colitis, but it may help alleviate some of its symptoms and reduce the frequency of ulcerative colitis incidents. Put simply, reduce your stress levels, reduce your discomfort caused by colitis.
It’s virtually impossible to avoid psychological stress and stressful situations at all times completely, so it’s unreasonable and unrealistic to think that you can manage your ulcerative colitis by keeping stress and anxiety out of your life. You can, however, realistically keep stress levels down by eating well and avoiding foods that trigger your ulcerative colitis, like whole grains, nuts, seeds, and fibrous fruits. It is also helpful to take any prescribed medications as directed, sleep well, exercise, have a strong support system, and commit to taking time to relax, through meditation, or just a few dedicated minutes each day for self-care. Yoga can be especially effective because, in addition to relieving symptoms of stress and anxiety, yoga has also been shown to relieve symptoms of ulcerative colitis.
Cognitive behavioral therapy can also be extremely helpful. Using CBT techniques, a psychologist or therapist can help you learn to observe your negative thoughts and then change or reframe them. Instead of “Oh no, here we go againâ¦,” you might think, “I’m going to face this flare-up more calmly, so it will be less severe than last time.”
Read Also: What Are The Symptoms Of Having An Ulcer