Surgery Can Truly Help
While surgery is always a major step and not without risks and complications, UC is principally surgically curable when the large intestine is removed because its limited to the colon and rectum, according to a study in Viszeralmedizin. While chronic pouchitis is one of the main factors limiting surgical success in curing UC, theres still a long-term pouch success rate of > 90%, 10 and 20 years later, researchers found. For most patients, when they get the surgery, there is actually a sense of relief, says Dr. Bedford. No more bloody stools. And typically no more abdominal pain and steroids.
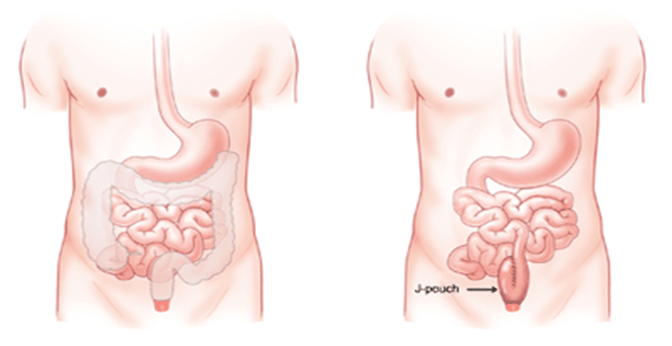
Total Proctocolectomy With End Ileostomy
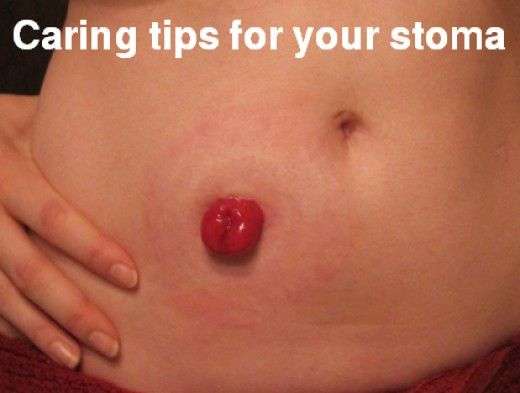
This proctocolectomy surgical procedure removes the colon, rectum, and anus, and creates an end ileostomy so that waste can exit your body into an ostomy bag.
-
This procedure is similar to the temporary ileostomy in the IPAA surgery, except the ileostomy will be permanent.
-
The stoma, or small hole created in the abdomen for the ileum, is about the size of a quarter, pinkish in color, and will appear moist and shiny. The stoma will protrude slightly outside of the abdomen.
-
After this surgery, you will wear an external ostomy pouch at all times to collect waste. The pouch must be emptied several times a day.
-
The ileostomy is usually placed in your lower abdomen to the right of your navel, just below the belt line.
Notify your doctor or other healthcare provider immediately if you experience these symptoms:
-
Infection from the surgery or at the site of the stoma
-
If no waste material exits the stoma for four to six hours and is accompanied by cramps and/or nausea, which could indicate a blockage
-
If your stoma is protruding more than normal outside of your abdominal wall, called prolapse, or retracting further inside your body, called retraction.
Whats The Recovery Like For A J
Each stage of J-pouch surgery is done 8 to 12 weeks apart. If you have a temporary ostomy, youll need to follow your doctors care instructions for emptying it and keeping it clean.
After your surgery is done, you may experience an increase in bowel movements. You may eliminate stool 12 times in one day. These bowel movements will gradually decrease in number after several months, as your anal sphincter muscles become stronger.
Your doctor may advise you to wait at least 6 weeks before resuming any physical activity. The exact timeline depends on how well your GI tract heals after surgery, as well as whether any complications arise.
Don’t Miss: Best Treatment For Diabetic Foot Ulcer
When Is Ulcerative Colitis Surgery Needed
Your doctor may suggest surgery if you can’t control inflammation and ulcers with medication or other treatments. You may also need an operation if you get emergency complications of ulcerative colitis such as severe bleeding or tears in the colon. Some people choose to have surgery if their symptoms affect their ability to work and stay active.
Treatment Of Ulcerative Colitis
Treatments for ulcerative colitis can control your symptoms and prevent flare-ups. The treatment you have will depend on several things. These include how severe your ulcerative colitis is and how much of your large bowel is affected. Youll be cared for by a team of healthcare professionals with specialist knowledge of inflammatory bowel diseases .
Also Check: How To Heal Mouth Ulcers Fast
What To Expect After Your Surgery
Most people do very well after their surgery and are able to return to work and their normal daily activities after they recover.
-
You should expect an adjustment period of up to one year to get used to the changes in your body after your proctocolectomy.
-
You will likely be on liquid or soft food diet for the first few days after surgery. Your doctor will then have you slowly introduce bland solid foods. You should chew your food thoroughly and avoid any foods that may cause gas, diarrhea or anal irritation. Its also important to drink plenty of water. We recommend six to eight glasses a day.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantomrectum and it completely normal. It does not require any treatment and often subsides over time.
-
Your doctor may recommend a physical activity restriction for a minimum of six weeks, depending on what type of surgery you had.
-
Talk to your doctor about resuming normal sexual activity after your surgery. Some people find their sex life improves some time after surgery due to improvements in pain, inflammation, and other ulcerative colitis symptoms.
In Ibd Patients Discussion Of Surgery Provides Valuable Education
We were unable to process your request. Please try again later. If you continue to have this issue please contact .Amy L. Lightner
In inflammatory bowel disease, as in most areas of medicine, surgery is reserved as a later option for cases that are unresponsive to less invasive treatments. However, for many patients, the conversation about surgery is best initiated earlier in their management instead of as a last resort.
When these patients get admitted with a severe flare, surgeons should be consulted sooner rather than later,Amy L. Lightner, MD, colon and rectal surgeon at the Mayo Clinic, said, referring specifically to ulcerative colitis . Even if the patient doesnt need surgery at admission, and they improve and respond to medical therapy, they are still overall at a higher risk of eventually needing surgery. I think, at least, that the education up front doesnt hurt.
The timeline for discussing surgery with an IBD patient often depends on whether the patient has UC or Crohns disease. Another factor is whether a patient presents electively in an outpatient setting, or whether the patient is admitted to the hospital in an emergent or urgent situation. In these situations, the goal is to arm the patient with knowledge of available options without causing undue alarm.
Healio: The conversation about surgery differs between patients with UC and those with Crohns. Can you discuss each condition?
Healio: Overall, do these surgeries turn out well?
Don’t Miss: How To Check A Horse For Ulcers
How To Take Tablets And Granules
You will either take the tablets or granules once a day, or as 2 or 3 smaller doses throughout the day.
Swallow the tablets whole with a drink of water or juice. Do not break, chew or crush them. This is because some tablets have a special coating to delay when they start to work, or to protect the medicine from the acids in your stomach.
For granules, open the sachet and tip the granules onto your tongue. Swallow them whole with a drink of water or juice. Do not chew them, as some granules have a special coating.
You can take some brands with food. Check the leaflet that comes with your medicine.
If you’re also taking indigestion medicines or remedies, leave a 2 hour gap before and after taking mesalazine. Indigestion treatments can affect how well the medicine works.
What Can Be Expected After Ileal Pouch Surgery
In most cases after ileal pouch surgery, quality of life improves over time. Patients can usually resume normal work and activities about 4-8 weeks after surgery. What ulcerative colitis patients like most about having any kind of pouch is that they no longer have the severe urgency or need to run to the bathroom.
After ileal pouch surgery, the patient must have an examination of the inside of the pouch with an instrument called an endoscope every year or every other year for the rest of his or her life to watch for the development of precancerous cells. In addition, all types of pouches can develop pouchitis, an irritation and inflammation of the inner lining of the pouch. Pouchitis is very common, but usually responds to oral antibiotics within 24 hours.
Overall, the long-term success rate of the pouch procedure is approximately 95%. However, there is a 5-10% chance of failure after pouch surgery. Most failures are due to the wrong diagnosis , persistent severe pouchitis, or complications of surgery.
In some cases, the pouch may need to be repaired or removed and replaced with a new pouch. Another option is to convert the pouch to a permanent ileostomy .
You May Like: L Glutamine Ulcerative Colitis Dosage
Proctocolectomy And Ileoanal Pouch
Proctocolectomy and ileoanal pouch-anal anastomosis is a newer procedure that allows a person to have bowel movements out of their natural anal opening. This procedure is sometimes called ileoanal pouch reservoir surgery or J-pouch surgery.
IPAA preserves the anus, rather than removing it. This procedure involves the following steps:
Stool gradually collects in the internal pouch and exits the body via the anus, making it more like a standard bowel movement.
If a persons anal muscles are in good condition, they will be able to feel stool coming out and will be able to use the toilet for bowel movements, as usual.
Although a surgeon preserves the anus with this procedure, the bowel movements are often more frequent and may be very soft or watery because the colon is missing.
Fecal incontinence may occur in some people, but medications are available that can help control bowel movements. A person should have good functioning of the anal muscles to help reduce the risk of incontinence.
Sometimes, surgeons perform IPAA in stages. The first stage involves making the pouch and connecting it to the anus. Then, the surgeon will leave the pouch alone to heal for several weeks.
Baseline Serological Fecal And Genetic Markers
Elevated C-reactive protein, elevated fecal calprotectin, and decreased albumin levels have been associated with colectomy. Other serological markers, such as perinuclear antineutrophilic cytoplasmic and anti Saccharomyces cerevisiae antibodies have not been associated with long-term colectomy risk.
Genetic variations in HLA, MDR1 and MEKK1 have also been associated with colectomy risk in UC, but are lacking confirmation.
You May Like: What Foods Should I Avoid With A Stomach Ulcer
The Advantages Of Biologics For Ulcerative Colitis
Biologics can improve gut symptoms, bringing about and maintaining remission in people with moderate to severe ulcerative colitis. They can also reduce the need for hospitalization and surgery, says the British organization Crohn’s & Colitis UK.
One key advantage of biologic therapies over other types of treatment for ulcerative colitis is that their mechanisms of action are more precisely targeted to the factors responsible for the condition, notes the Crohns & Colitis Foundation.
Unlike corticosteroids, for example, which affect the whole body and may produce major side effects, biologic agents act more selectively. These therapies are targeted to particular proteins that have already been proven to be involved in ulcerative colitis.
Patients are often nervous about biologics, says Laura Raffals, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota. But theyre not as scared about taking a corticosteroid, and thats an important conversation to have because the data shows that patients on biologics are much safer and stay in remission longer. The serious side effects we see are from steroids or narcotics, not biologics.
What Ulcerative Colitis Surgery Involves
A surgeon usually removes your colon and rectum. Next they’ll attach the lowest part of your small intestine to a hole they make in your torso to let waste leave your body and empty into an external bag. Another procedure creates an internal waste pouch that allows stool to be passed through the anus.
Read Also: How To Cure Gastritis And Ulcers Naturally
Perforation Of The Bowel
Chronic inflammation may weaken the wall of the intestine and cause a hole called a perforation. This can also happen if a portion of the bowel expands and weakens near a stricture. Once the intestinal wall has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
What Is An Ileal Pouch
In some cases of colorectal disease, such as chronic ulcerative colitis, familial adenomatous polyposis , or colorectal cancer, all of the colon and rectum must be removed using a surgery called a total proctocolectomy.
After surgical removal of the large bowel, which absorb liquids and then stores and eliminates solid wastes, patients may be candidates for an ileal pouch-anal anastomosis procedure to provide a new way to store and pass stools the normal way, without a permanent bag.
The term anastomosis means a joining together of disconnected parts, like joining two pipes. In the case of an IPAA, the ileum is formed into a new reservoir to store solid wastes. This reservoir or pouch is connected to the anus to provide for elimination the normal way. The pouch enables the patient to store and pass stool through the bodys usual route, so that the patient doesnt need an external bag to collect waste.
There are three different types of ileal pouches: J-pouch , S-pouch, and the K-pouch. The J-pouch and S-pouch resemble the letters in the their names.
In order to have an ileal pouch procedure, the patients intestines, anus, anal sphincter muscles, and pelvic nerves must still be able to function normally. This will allow the person to maintain control of bowel movements once a pouch is constructed, and avoid bowel accidents.
Read Also: How Do I Know If I Have A Peptic Ulcer
Proctocolectomy: Removal Of Colon And Rectum
In this operation, also called a permanent or Brooke Ileostomy, your surgeon removes the colon and rectum and closes off the anus. They then make a hole in your belly, called a stoma. After surgery, waste will move from your small intestine, out the stoma, and into a plastic ostomy bag. While wearing a bag you’ll still be able to work, be intimate, and play sports.
What Are The Benefits Of Ulcerative Colitis Surgeries
If the entire colon and rectum are removed, ulcerative colitis is cured. This should put an end to the diarrhea, abdominal pain, anemia, and other symptoms.
In addition, this surgery prevents colon cancer. Overall, an estimated 5% of ulcerative colitis patients will get cancer. Removing the colon cancer threat is especially significant for people who have ulcerative colitis that affects the entire colon. In these cases, as opposed to cases of ulcerative colitis that affect only the lower colon and the rectum, the cancer risk without surgery could be up to 32 times the normal rate.
Also Check: Does Smoking Cause Ulcers After Gastric Bypass
Who Can And Cannot Take Mesalazine
Adults and children aged 5 years and older can take mesalazine.
Mesalazine may not be suitable for some people. To make sure it’s safe for you, tell a pharmacist or doctor before taking or using it if you:
- have ever had an allergic reaction to mesalazine, aspirin, or any other salicylates such as methylsalicylate or choline salicylate
- have ever had an allergic reaction to any other medicine
- have any problems with your kidneys or liver
- have a rare blood condition called porphyria
- are trying to get pregnant, already pregnant, or breastfeeding
Taking Care Of Yourself
Its natural that living with ulcerative colitis can make you feel stressed at times. Stress can sometimes trigger flare-ups so you may find it helpful to try some relaxation techniques. These may include deep breathing, meditation, yoga and mindfulness.
Regular exercise can also help to give you a boost and make you feel better. It can also improve your general health and help to keep your bones and muscles strong. This is important because some medicines for ulcerative colitis may affect your bone health.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
What Types Of Surgery Can Treat Ulcerative Colitis
There are different procedures. All are major surgery on your digestive system. Talk with your doctor about which one they recommend for you.
Hemicolectomy. This is an operation that removes part of your colon. There are two types, depending on where your problem area is:
- Right hemicolectomy: Removes the right, or ascending, part of your colon. The surgeon may also take out some other areas, like your appendix and part or all of your middle large intestine. They’ll connect what’s left of your colon to your small intestine.
- Left hemicolectomy: Removes the left, or descending, part of your colon. The surgeon will attach the right and middle parts to your rectum. This is the last place your bowel movements pass through on their way out.
Colectomy. This is surgery to remove the entire colon.
Proctocolectomy. This procedure removes both the colon and rectum.
Proctocolectomy is considered the standard treatment when surgery for ulcerative colitis is needed.
If the entire colon is removed, the surgeon may create an opening, or stoma, in the abdominal wall. The tip of the lower small intestine is brought through the stoma. An external bag, or pouch, is attached to the stoma. This is called a permanent ileostomy. Stools pass through this opening and collect in the pouch. The pouch must be worn at all times.
Are There Any Risks Or Complications To Be Aware Of

Despite the potential benefits, the J-pouch procedure is still considered major surgery. As with any major surgery, you may be at risk for infections, bleeding, and side effects from general anesthesia.
Sometimes its possible for the newly formed J-pouch to become infected. However, such risks are higher in one-stage procedures.
Other potential complications from this procedure include:
Overall, the outlook for J-pouch surgery is positive, with few people experiencing pouch failure.
However, one study published in 2015 reported a J-pouch failure rate of between 3.5 and 15 percent. Pouch failures have also been found to be more common in men than women.
If you do develop pouch failure, your doctor may recommend either an ostomy or another type of colorectal procedure called a K-pouch surgery.
Pouchitis is the most common problem following J-pouch surgery and other pouch surgeries. This is a treatable condition and does not necessarily mean youll develop pouch failure. However, chronic pouchitis has been linked to possible failure of the J-pouch.
Also Check: Wound Vac For Pressure Ulcers