Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
Constipation Associated With Cow Milk Allergy
In contrast to the bloody diarrhea associated withallergic proctitis of infancy or food protein-induced enterocolitis syndrome, several studies suggest that cow milk protein allergy may be associated with constipation through an immunologically mediated response. Children typically present during the first few years of life with symptoms of constipation or partial obstruction soon after beginning cow milk. In the initial report of this condition, over three-quarters of the subjects showed evidence of IgE sensitization to cow milk. Endoscopic evaluation of the distal rectal mucosa revealed mild eosinophilic inflammation without crypt invasion. Removal of cow milk increased the number of stools and reintroduction led to a decline in the number of stools per day.
Aldo A.M. Lima, … Richard L. Guerrant, in, 2015
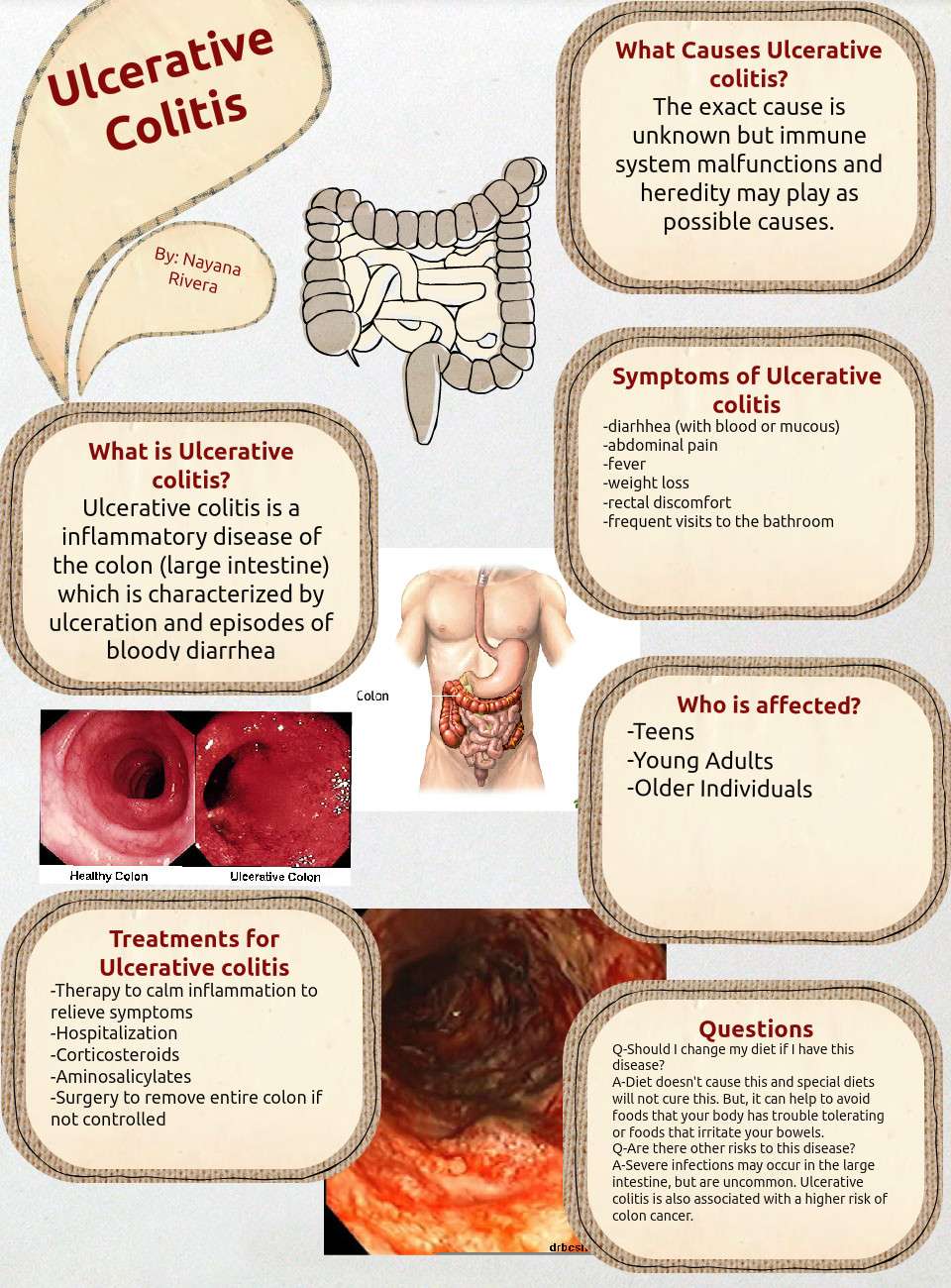
What Causes Ulcerative Colitis
In some cases, bleeding from ulcerative colitis can lead to significant blood loss. The ultimate goal of treatment will be to calm the inflammation and stop the bleeding, but treating the loss of blood may also be necessary.
In milder cases of anemia from ulcerative colitis, supplementing with iron, folic acid, and vitamin B12 may help to form new blood cells. In more serious cases of blood loss, a blood transfusion might be needed.
The most severe bleeding caused by ulcerative colitis could be life-threatening. This is not common, but if the bleeding can’t be stopped, surgery to remove the colon and create an ileostomy may be needed.
During ileostomy surgery the large intestine is removed and a stoma is created to allow waste to pass outside the body and into a collection bag that is worn on the abdomen.
Another surgery might be done at a later date to create a j-pouch, which creates a way to go to the bathroom through the rectum instead of through the stoma.
Read Also: Natural Remedies For Mouth Ulcers
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Will Surgery Cure A Peptic Ulcer
Medical therapy works in most people with peptic ulcers. Sometimes, medical therapy does not work, or a person cant take the therapy for some reason. Surgery is an alternative to medical therapy for these people.
Surgical operations often used in peptic ulcers include the following:
- Vagotomy: Cutting the vagus nerve, which transmits messages from the brain to the stomach, can reduce acid secretion. However, this can also interfere with other functions of the stomach. A newer operation cuts only the part of the nerve that affects acid secretion.
- Antrectomy: This is often done in conjunction with a vagotomy. It involves removing the lower part of the stomach . This part of the stomach produces a hormone that increases production of stomach acid. Adjacent parts of the stomach may also be removed.
- Pyloroplasty: This procedure also is sometimes done with vagotomy. It enlarges the opening between the stomach and duodenum to encourage passage of partially digested food. Once the food has passed, acid production normally stops.
- Tying off an artery: If bleeding is a problem, cutting off the blood supply to the ulcer can stop the bleeding.
Don’t Miss: What Is The Difference Between Colitis And Ulcerative Colitis
Treatment For Anal Fissure
You can treat an anal tear at home in several ways:
- Eat a high-fiber diet and take over-the-counter supplements to bulk up and soften your stools.
- Take sitz baths â aka soak your bottom in a warm tub â several times a day. This will relax your anal sphincter muscles and soothe the painful area. Your sphincter is the ring-like muscle at the opening of your anus. It works to let stools pass.
- Drink more water.
- Use topical ointments or other meds your doctor prescribes.
You likely wonât need surgery for an anal fissure, unless itâs ongoing. In that case, your surgeon might inject Botox into your anal sphincter, or cut a small part of the muscle to relax it and lessen spasms and pain.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Recommended Reading: How To Heal Venous Stasis Ulcers
What Does Blood In Stools Look Like
Blood from your stool could look bright red, or it might be dark red or black.
How the blood looks depends on where it is coming from.
Spots of red blood on the toilet paper, drops in the toilet bowl, blood on the surface of your stool or in your underwear indicate the bleeding is coming from the anus or lower rectum.
If the blood is mixed in with your stool, this suggests bleeding might be from higher up in the bowel.
If your stools are black and like tar, and they smell bad, this is also probably because the blood is coming from higher up in the bowel.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Recommended Reading: What Is Refractory Ulcerative Colitis
What Is The Cause Of Peptic Ulcers
When you eat, your stomach produces hydrochloric acid and an enzyme called pepsin to digest the food.
- The food is partially digested in the stomach and then moves on to the duodenum to continue the process.
- Peptic ulcers occur when the acid and enzyme overcome the defense mechanisms of the gastrointestinal tract and erode the mucosal wall.
In the past it was thought that ulcers were caused by lifestyle factors such as eating habits, cigarettesmoking, and stress.
- Now it is understood that people with ulcers have an imbalance between acid and pepsin coupled with the digestive tracts inability to protect itself from these harsh substances.
- Research done in the 1980s showed that some ulcers are caused by infection with a bacterium named Helicobacter pylori, usually called H pylori.
- Not everyone who gets an ulcer is infected with H pylori. Aspirin and nonsteroidal anti-inflammatory drugs can cause ulcers if taken regularly.
Some types of medical therapy can contribute to ulcer formation. The following factors can weaken the protective mucosal barrier of the stomach increasing the chances of getting an ulcer and slow the healing of existing ulcers.
- Aspirin, nonsteroidal anti-inflammatory drugs , and newer anti-inflammatory medications
- Alcohol
- Cigarettesmoking
- Radiation therapy:-used for diseases such as cancer
People who take aspirin or other anti-inflammatory medications are at an increased risk even if they do not have H pylori infection.
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Recommended Reading: Best Grain For Horses With Ulcers
Treatment For Rectal Bleeding
The kind of treatment you require depends on your diagnosis and location of the bleeding.
You should notify your doctor at first sight of the blood, as causes of rectal bleeding can be as harmless as a hemorrhoid and as severe as cancer. You will also want to monitor the accompanying symptoms to help you narrow down on the cause of your blood in stool. Once you run the necessary tests, your doctor will be able to confirm your diagnosis and put you on a treatment plan.
Rectal bleeding treatment may involve managing hemorrhoids, replenishing blood loss, supplementing vitamins and minerals, using ointments or suppositories, staying well hydrated, preventing constipation and diarrhea, increasing your fiber intake, avoiding sitting on the toilet for prolonged periods of time, and applying ice packs in case of pain.
Mohan Garikiparithi got his degree in medicine from Osmania University . He practiced clinical medicine for over a decade before he shifted his focus to the field of health communications. During his active practice he served as the head of the Dept. of Microbiology in a diagnostic centre in India. On a three-year communications program in Germany, Mohan developed a keen interest in German Medicine , and other alternative systems of medicine. He now advocates treating different medical conditions without the use of traditional drugs. An ardent squash player, Mohan believes in the importance of fitness and wellness.
Rectal Bleeding And Inflammatory Bowel Disease
One of the many symptoms of inflammatory bowel disease is bleeding. Blood might appear in or on the stool or some people may pass no stool at all at times, and just pass blood.
Bleeding from the rectum and large intestine from IBD is typically red or bright red, while blood coming from higher up in the digestive tract could appear as darker or black stools. In most cases this bleeding is slow and steady.
However, you should get emergency attention if:
- Bleeding is severe
- You’re vomiting blood
- You faint or feel like you’re going to
Blood in or on the stool can be frightening but it doesn’t always mean that there’s an emergency. It’s sometimes part of an IBD flare-up and it should be discussed with a physician as soon as possible, especially if it hasn’t happened in a while.
Bleeding means that there is some inflammation somewhere, and a change in treatment might be needed. Many treatments are available for IBD that can help stop the inflammation and the bleeding.
Read Also: Best Probiotic Brand For Ulcerative Colitis
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: Ulcerative Colitis And Lactose Intolerance
What Are Causes To Bleeding Ulcers In The Stomach
Causes Use of NSAIDs. High doses of common NSAIDs such as ibuprofen and aspirin may cause peptic or bleeding ulcers. H. pylori infection. Zollinger-Ellison syndrome Zollinger-Ellison syndrome is an uncommon condition that causes tumors in the stomach, duodenum, or pancreas. Ulcers with other causes.
Read Also: Can Ulcerative Colitis Cause Blood In Urine
Common Causes Of Proctitis Include:
- Dysentery .
- sexiuallyitransmitted diseases of the irectumi and analiicanali.
- rectalii ulcers.
- Severe forms of food allergy or intolerance.
- Anorectali cancers.
- A continuous feeling that you need to have a bowel movement .
- rectalii bleeding.
- Passage of mucus, alone or with blood and stool.
- abdominal pain .
- Diarrhea.
Analysis Of Focus Group Data
Each focus group meeting was audiotaped and fully transcribed. Each transcript was entered into NVivo version 2.0. Two members of the study team independently reviewed each transcript with a holistic view of symptoms and themes from each of the five focus group meetings and generated a list of symptom domains and common themes discussed by participants of each focus group . These lists were compared for agreement and consensus was reached . This list served as a template for a coding scheme used to analyze each transcript. The transcripts were independently coded by symptom domain and theme by J.C.J. and A.K.W. and codes were compared for agreement.
Recommended Reading: What’s The Signs Of An Ulcer
How Is Acute Bacterial Dysentery Differentiated From Acute Onset Of Ischemic Colitis
The degree of bloody diarrhea is variable in patients with ischemic colitis, and it may be difficult to distinguish between the two diseases. Clinically, the patient with ischemic colitis complains of sudden-onset abdominal pain, and an acute abdominal series may show thumbprinting of the colonic mucosa.
Flexible sigmoidoscopy is the mainstay of diagnosis for ischemic colitis. The rectum is usually spared because of its collateral blood flow. Above the rectum, the mucosa becomes friable and edematous, and there may be hemorrhagic areas and ulcerations resembling those of Crohn’s disease. Angiography is not generally helpful in the evaluation of ischemic colitis ischemic colitis is a small-vessel disease compared with mesenteric midgut ischemia of the small bowel, which involves thrombosis or embolism in the superior mesenteric artery . A barium enema is contraindicated in patients with suspected ischemic colitis, because colonic expansion during barium instillation may promote further ischemia.
Glenn T. Furuta, in, 2004
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
You May Like: Will Ulcers Cause Blood In Stool
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Burning Pain In Your Abdomen
This may seem like a no-brainer but the most common sign that people experience when they have a stomach ulcer is a persistent burning pain in their abdomen. This sensation occurs when juices in the stomach used for digestion come into contact with the open sore. For the most part, the pain is felt from the breastbone to navel and is often worse at night than during the day. On the other hand, if you are someone who frequently skips meals, you may find that you experience this pain much throughout the daytime.
Dont Miss: How Long Does A Ulcerative Colitis Flare Up Last
Recommended Reading: Diabetic Foot Ulcer Treatment Guidelines
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
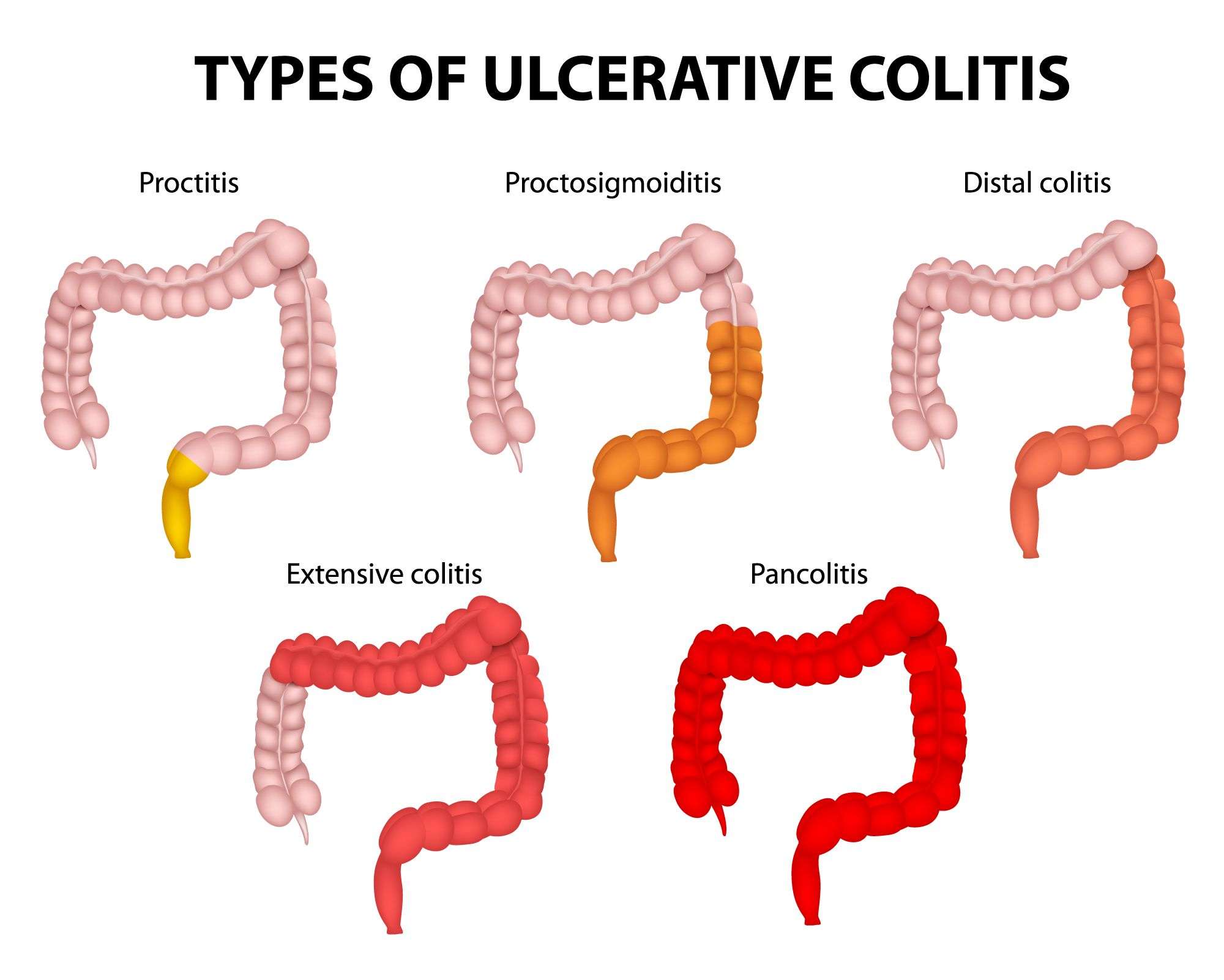
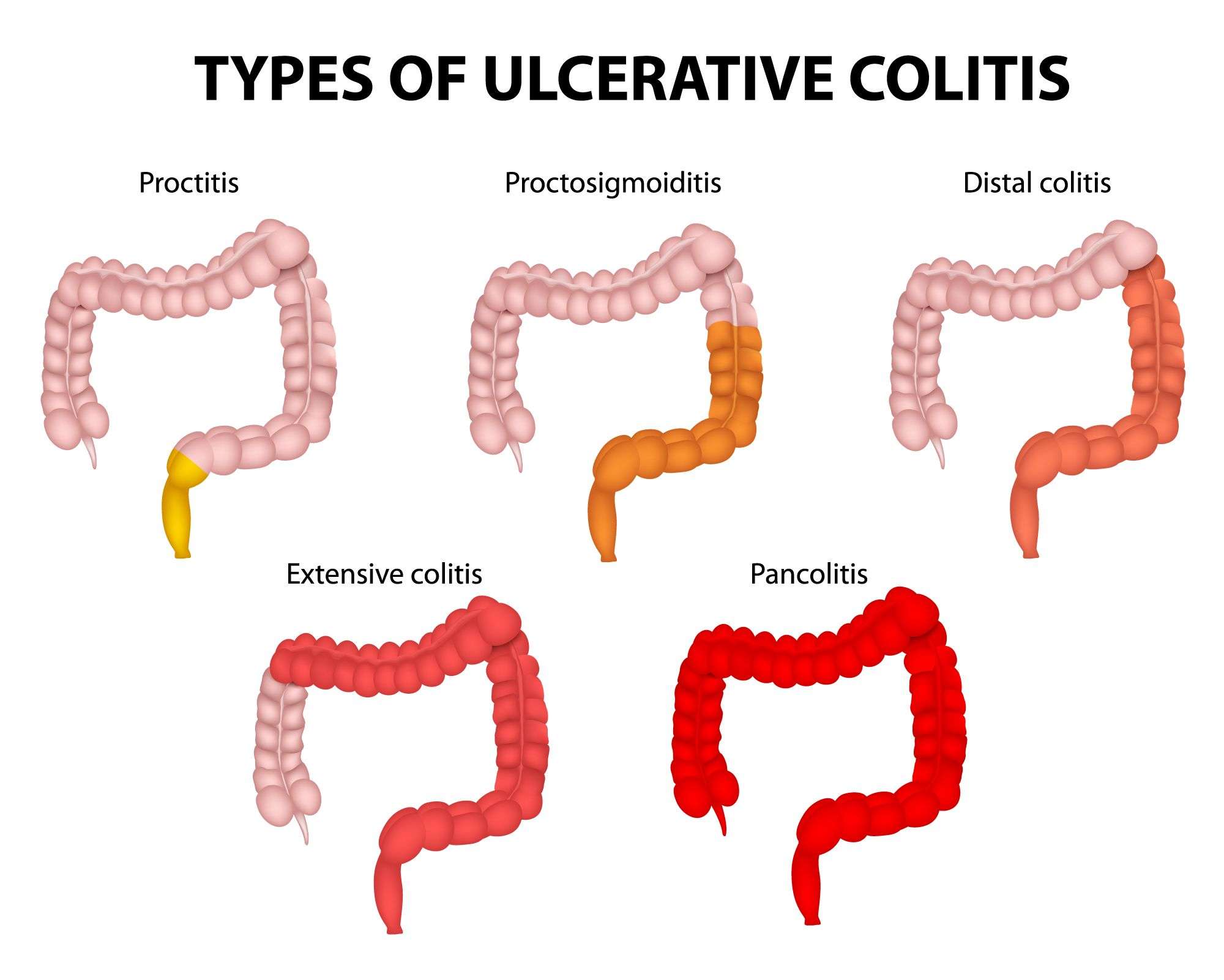
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
What Does Your Stool Look Like With Ulcerative Colitis
Ulcerative colitis is a disease that involves the inner lining of the large bowel. It causes abdominal pain and bleeds due to erosions and ulcers all over the large intestine and rectum. Inflammatory bowel disease is a lifelong illness with no specific cause or cure. Patients have repeated cycles of flare-ups and remission with potential extraintestinal manifestations. Flare-ups may last days to a few weeks. Remission might last for months or even years.
UC is a lifelong disease with constant periods of flare-ups and remission. Several treatment options and lifestyle modifications reduce the symptoms and prevent flare-ups. Stool-related symptoms of UC include
- Diarrhea or loose stools more than four episodes a day
- Bloody stools, which may be bright red, pink or tarry
- Ribbon-like stools in case of narrowed intestines due to a long-standing disease
Diarrhea may be associated with cramps and abdominal pain. There may also be a constant feeling of the need to evacuate the bowels .
Recommended Reading: What To Take For An Ulcer Over The Counter