If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
Stage 2 Pressure Ulcers
Partial epithelial deficiency may appear both above and below the skins surface. The painful area is largening, the skin is hot and epithelial. Decubitus is starting to look like a bruise.
At this stage, pressure ulcers can be effectively treated, thus preventing the development of deep, ulcersative decubitus. If there is no serious intervention, decubitus enters stage 3 in just a couple of hours.
Where To Get Help
- Hospital staff
- Domiciliary care staff
- Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries, Plast Reconstr Surg. 2017 Jan 139:275e-286e
- Walia GS, Wong AL, Lo AY, Mackert GA, Carl HM, Pedreira RA, et al. Efficacy of Monitoring Devices in Support of Prevention of Pressure Injuries: Systematic Review and Meta-analysis. Adv Skin Wound Care, 2016 Dec 29:567-574
- Wound, Ostomy and Continence Nurses Society-Wound Guidelines Task Force, WOCN 2016 Guideline for Prevention and Management of Pressure Injuries : An Executive Summary. J Wound Ostomy Continence Nurs. 2017 May/Jun 44:241-246
- Scafide KN, Narayan MC, Arundel L. Bedside Technologies to Enhance the Early Detection of Pressure Injuries: A Systematic Review, J Wound Ostomy Continence Nurs. 2020 Feb 13.
- Munoz N, Posthauer ME, Cereda E, Schols JMGA, Haesler E. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Adv Skin Wound Care, 2020 Mar 33:123-136.
- Qigui X, Qinling Y, Huapeng L. Meta-analysis of effect of foam dressing and hydrocolloid dressing on bedsore management. Chinese Nurs Res. 2017 31:3397-3400.
- Westby MJ, Dumville JC, Soares MO, Stubbs N, Norman G. Dressings and topical agents for treating pressure ulcers. Cochrane Database Syst Rev. 2017 6.
Don’t Miss: How To Stop Ulcers From Hurting
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
Recommended Reading: Food Not Good For Stomach Ulcer
Diagnosis Of A Decubitus Ulcer
Wound care physicians and nurses experienced in pressure ulcers are often consulted for decubitus ulcer diagnosis. Medical personnel may take samples of the pressure ulcer tissue and fluid to look for bacteria or cancer. They may also do blood cultures, bone scans or other tests depending on the seriousness of the ulcer. In addition, they will evaluate the condition of the ulcer according to:
- The size of the decubitus ulcer and depth of the crater
- What kind of tissue is affected by the ulcer: skin, bone, or muscle
- The color of the ulcer and skin around it
- The tissue death caused by the ulcer
- The presence of infection, bleeding or foul odor
Stage 2 Pressure Sores
When you get into stage 2 of a pressure sore it is when there is top tissue damage. or underlying tissue damage the dermis layer. This is when a small or wound that can be open might start to form. It may also look like a blister. This is when medical assistance should be sought because there are chances if its not dealt with properly it can form into a higher risk pressure sore.
You May Like: Ulcerative Colitis Rectal Pain Relief
What Complications Might Come With Pressure Ulcers
Pressure ulcers can be painful and become infected, and infection may spread from the skin , to blood , muscle or bone. Treatment may require antibiotics, usually at home but sometimes in hospital. In very rare cases, chronic pressure ulcers can cause skin cancer. It’s important to recognise pressure ulcers early and to act quickly to prevent complications.
Keep The Skin Dry And Clean
Incontinence is one of the biggest factors associated with the development of pressure sores. When bowel movement or urine stays in contact with the skin, acids and enzymes in them will begin to cause excoriation and degradation of the skin faster than usual. When combined with limited ability to reposition oneself, a senior may develop a pressure sore in the perineal area faster.
If the area appears to become reddened, the senior may have developed a Stage I pressure sore. When this occurs, it is best to assume the area has been subject to more intense pressures and proceed with an appropriate treatment, such as the use of a barrier cream to help prevent further excoriation due to bodily substances. However, the use of a barrier cream does not negate the need for continued repositioning and movement to help prevent worsening of the area.
Read Also: How To Eat With A Stomach Ulcer
Description Of The Intervention
The aim of pressure ulcer prevention strategies is to reduce either the magnitude, or duration, of pressure between a patient and his support surface , or both. This may be achieved by regular manual repositioning , or by using pressurerelieving support surfaces such as cushions, mattress overlays, replacement mattresses or whole bed replacements, which are widely used in both institutional and noninstitutional settings. Often a combination of repositioning and support surface enhancement may be used. Support surfaces are used with the aim of redistributing pressure, reducing shearing forces and controlling the local microclimate. The cost of these interventions varies widely from over GBP 30,000 for some bed replacements, to less than GBP 100 for some foam overlays. Information on the relative costeffectiveness of this equipment is needed to inform use.
Symptoms Of Pressure Sores
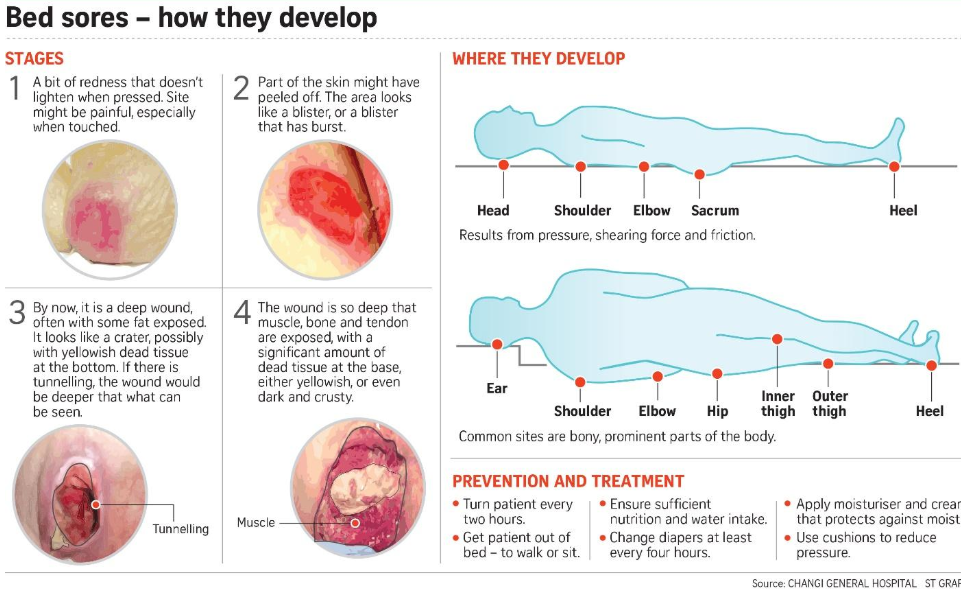
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
- Fever
- Weakness
Recommended Reading: What To Do For Ulcerative Colitis Flare Up
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
What Are Pressure Sores

Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
Recommended Reading: Can Food Allergies Cause Ulcerative Colitis
Treatment Of Pressure Ulcers On The Buttocks
Pressure ulcers are a complex health problem whether they are on the buttocks or another area of the body. They can arise as a result many interrelated factors and they can be painful, debilitating and life threatening. Care and treatment of pressure ulcers may be provided by a multidisciplinary team made up of different disciplines of healthcare professionals.
This MDT may include:
- a dietician
- experienced medical and surgical experts
The specific treatment of a pressure ulcer can depend on the stage a pressure ulcer has reached.
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
You May Like: How To Stop An Ulcerative Colitis Flare
Don’t Miss: Foods To Eat If You Have A Stomach Ulcer
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
How Can I Prevent Pressure Ulcers
Pressure ulcers can be avoided, but often you may need help. If you have difficulty moving, preventing pressure ulcers might require a team effort, involving your health team, carer or a family member.
To protect your skin and prevent pressure ulcers, the following will help:
- Keep active and move as much as you can .
- Eat a variety of nutritious foods, including plenty of fruits and vegetables.
- Drink plenty of fluids to make sure you are hydrated.
- Avoid smoking because this reduces blood flow to your skin.
- Avoid firm massage, especially over bony areas.
- Keep your skin dry as far as possible.
- If you feel any skin pain or a feeling of burning, tell your doctor.
There are several things that will help you care for your skin:
- Instead of soap, use a mild cleanser and dry the skin gently afterwards.
- Apply moisturisers if the skin is dry, flaky or seems to crack easily.
- Use barrier cream in skin folds.
- Use warm water when having a bath or shower.
It is important to move around as often as you are able. Continuous pressure on the same areas can lead to a pressure ulcer developing very quickly. The following may help you avoid this:
- Change positions in bed at least every 30 minutes and, if you can, stand up and walk around.
- If you cant stand, move as much as you are able for example, lean forward or move side to side in your chair for 2 minutes to take the pressure off your bottom and hips.
- Try to avoid slumping or sliding forward in your chair.
Also Check: Ulcer Signs Symptoms And Treatment
Signs And Symptoms Of Pressure Ulcers
What are the signs of pressure ulcers?
Firstly you can only recognize the redness of the skin, which is slightly inflamed. It quickly turns to be itchy and burning, followed by increasing pain. The feel of discomfort depends on how advanced the decubitus is.
In the following, we describe the stages of pressure ulcers and the symptoms of them.
What Increases The Risk Of Developing Pressure Ulcers
People who are confined to a bed or chair for example due to stroke, spinal injury or dementia are at greater risk of developing extensive pressure ulcers. Other risk factors include:
- immobility being confined to bed after an illness or surgery, or due to paralysis
- diabetes and other health conditions that can affect blood supply
You May Like: How To Prevent Pressure Ulcers In The Hospital
Also Check: Icd 10 Venous Stasis Ulcer
Encourage Seniors To Maintain A Healthy Diet
The benefits of a well-functioning circulatory system are only as good as the nutrients it delivers. Seniors should strive to eat a well-balanced, healthy diet, explains Medscape. In fact, optimizing the nutritional status of a senior living with a pressure sore is key to ensuring successful treatment. For seniors living with metabolic disorders, such as diabetes, a healthy diet can go much further than simply preventing or encouraging the healing of pressure sores.
Try To Maintain Nutrition
There is a strong correlation between nutrition deficits and pressure ulcer risk. If your loved one has an appetite, try to maintain adequate nutrition with nutrient-rich foods . If his appetite is waning, offer supplements such as Ensure or Boost to help bolster nutrition.
Nutrition is often a problem in palliative care patients and its important to note here that you should never try to force your loved one to eat.
Also Check: How To Find Out If You Have Ulcerative Colitis
How Often Is Repositioning Necessary
Even though it’s often recommended that people be repositioned every two hours, there’s no single recommendation that works for everyone. Some people can lie in the same position for quite a long time without getting ulcers, while others need to switch much more often. Research has not yet found out how often someone should change position to get the best preventive effect.
Unnecessarily moving someone too much for no good reason can also have disadvantages. For instance, repositioning every two hours at night may wake the person each time and keep them from getting a good nights sleep. Changing position can also be very painful for people who have wounds or joint conditions. Frequent repositioning is physically demanding for caregivers or family members too. It’s therefore important to observe how often someones position really needs to be shifted. It can then help to make a note every time they are repositioned.
Students Who Viewed This Also Studied
eduaction quality of life 214.pdf
St. Johns University
PHD212 Powders Calculation discussion .pdf
St. Johns University
Introduction to semi solid dosage forms C.pdf
St. Johns University
Dashboard and Health Care Benchmark Evaluation.docx
St. Johns University
St. Johns University HSA NURSING RE
eduaction quality of life 214.pdf
St. Johns University HSA NURSING RE
PHD212 Powders Calculation discussion .pdf
St. Johns University HSA NURSING RE
Introduction to semi solid dosage forms C.pdf
St. Johns University HSA NURSING RE
Dashboard and Health Care Benchmark Evaluation.docx
St. Johns University HSA NURSING RE
Case 1.docx
St. Johns University HSA NURSING RE
Dashboard Benchmark Evaluation.docx
Upload your study docs or become a
Course Hero member to access this document
Upload your study docs or become a
Course Hero member to access this document
You May Like: How To Get Remission In Ulcerative Colitis
Read Also: What To Take For Stomach Ulcer Pain