Why Does Decubitus Ulcer Occur
Asked by: Prof. Malcolm Cummerata IV
What causes a decubitus ulcer? Prolonged pressure is essentially the main cause of a decubitus ulcer with other factors such as moisture, poor circulation, and poor nutrition contributing. Lying on a certain part of your body for long periods may cause your skin to break down.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
How Can I Prevent Pressure Ulcers
Pressure ulcers can be avoided, but often you may need help. If you have difficulty moving, preventing pressure ulcers might require a team effort, involving your health team, carer or a family member.
To protect your skin and prevent pressure ulcers, the following will help:
- Keep active and move as much as you can .
- Eat a variety of nutritious foods, including plenty of fruits and vegetables.
- Drink plenty of fluids to make sure you are hydrated.
- Avoid smoking because this reduces blood flow to your skin.
- Avoid firm massage, especially over bony areas.
- Keep your skin dry as far as possible.
- If you feel any skin pain or a feeling of burning, tell your doctor.
There are several things that will help you care for your skin:
- Instead of soap, use a mild cleanser and dry the skin gently afterwards.
- Apply moisturisers if the skin is dry, flaky or seems to crack easily.
- Use barrier cream in skin folds.
- Use warm water when having a bath or shower.
It is important to move around as often as you are able. Continuous pressure on the same areas can lead to a pressure ulcer developing very quickly. The following may help you avoid this:
- Change positions in bed at least every 30 minutes and, if you can, stand up and walk around.
- If you cant stand, move as much as you are able for example, lean forward or move side to side in your chair for 2 minutes to take the pressure off your bottom and hips.
- Try to avoid slumping or sliding forward in your chair.
You May Like: Best Medicine For Ulcerative Colitis
Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to “NHLC attorneys” or “our attorneys” are references to attorneys within NHLC’s network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered ‘attorney advertising’ and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Don’t Miss: Holistic Cure For Ulcerative Colitis
Where Does The Word Decubitus Come From In Medicine
Commonly used in medicine, the word decubitus is used to mean lying down. It is derived from the Latin verb decumbere meaning to lie down. When medical professionals use this term to describe the position of a patient, they first state the part of the body on which the patient is resting followed by
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
You May Like: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
What Is The Dermis Made Up Of
The dermis has connective tissue, blood vessels, oil and sweat glands, nerves, hair follicles, and other structures. It is made up of a thin upper layer called the papillary dermis, and a thick lower layer called the reticular dermis. Anatomy of the skin, showing the epidermis, dermis, and subcutaneous tissue.
You May Like: Food To Avoid For Ulcer Patient
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Can Bedsores Be Prevented
Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas. Other methods of preventing bedsores and preventing existing sores from getting worse include:
- Turning and repositioning every 2 hours
- Sitting upright and straight in a wheelchair, changing position every 15 minutes
- Providing soft padding in wheelchairs and beds to reduce pressure
- Providing good skin care by keeping the skin clean and dry
- Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores cant heal, no matter how well you care for the sore
Read Also: Pressure Ulcers Are Most Likely To Develop
Spotlight On Aging: Pressure Sores
|
Aging itself does not cause pressure sores. But it causes changes in tissues that make pressure sores more likely to develop. As people age, the outer layers of the skin thin. Many older people have less fat and muscle, which help absorb pressure. The number of blood vessels decreases, and blood vessels rupture more easily. All wounds, including pressure sores, heal more slowly. Certain risk factors make pressure sores more likely to develop in older people: |
Causes that contribute to the development of pressure sores include
-
Pressure
-
Friction
-
Moisture
Pressure on skin, especially when over or between bony areas, reduces or cuts off blood flow to the skin. If blood flow is cut off for more than a few hours, the skin dies, beginning with its outer layer . The dead skin breaks down and an open sore develops. Most people do not develop pressure sores because they constantly shift position without thinking, even when they are asleep. However, some people cannot move normally and are therefore at greater risk of developing pressure sores. They include people who are paralyzed, comatose, very weak, sedated, or restrained. Paralyzed and comatose people are at particular risk because they also may be unable to move or feel pain .
Friction can lead to or worsen pressure sores. Repeated friction may wear away the top layers of skin. Such skin friction may occur, for example, if people are pulled repeatedly across a bed.
-
Meticulous hygiene and care of skin
-
Maintaining movement
What Are The Four Stages Of Decubitus Ulcers
Stages of decubitus ulcers
- Stage 1. The skin isn’t broken, but it’s discolored. …
- Stage 2. There is breakage in the skin revealing a shallow ulcer or erosion. …
- Stage 3. The ulcer is much deeper within the skin. …
- Stage 4. Many layers are affected in this stage, including your muscle and bone.
- Unstageable.
Don’t Miss: List Of Foods To Eat When You Have An Ulcer
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Read Also: What Foods Irritate An Ulcer
What Causes A Decubitus Ulcer To Develop
By Nursing Home Law Center
Originating from the Latin term meaning to lay down decubitus ulcers are perhaps most accurately categorized as an open wound on the skin that can penetrate to the surrounding tissues, muscle and bone in the area. Decubitus ulcers are most prevalent on people with limited mobility or who may be immobile and bedridden for prolonged periods of time particularly during admissions to nursing homes, assisted living facilities or hospitals.
Remaining in one position for extended periods without any pressure relief can gradually reduce the blood supply and circulation to the area and cause a decubitus ulcer to develop. If the resulting decubitus ulcer is not identifided and treated by attending staff in its early stages, a small decubitus ulcer can rapidly progress resulting in large, open-wounds and serious medical complications or even death can ensue.
Though decubitus ulcers may affect any person with compromised mobility, the development of decubitus ulcers in patients in nursing homes, hospitals and assisted living facilities has become an perceived part of the aging process.
As opposed to simply being an emblem of old age, decubitus ulcers commonly arise with the convergence of several risk factors including: immobility, unrelieved pressure, malnourishment, dehydration and inadequate staffing levels impact the patient on their own or in concert with one another.
Related Information
Is A Decubitus Ulcer A Diabetic Ulcer
Skin necrosis and gangrene are also included in the current system as ulcers. This definition is similar to that of the EPUAP, all-inclusive and, as such, any pressure ulcer on the foot of a person with diabetes is a diabetic foot ulcer as is any traumatic wound, including a thermal or chemical injury.
You May Like: Bleeding Ulcer Treatment At Home
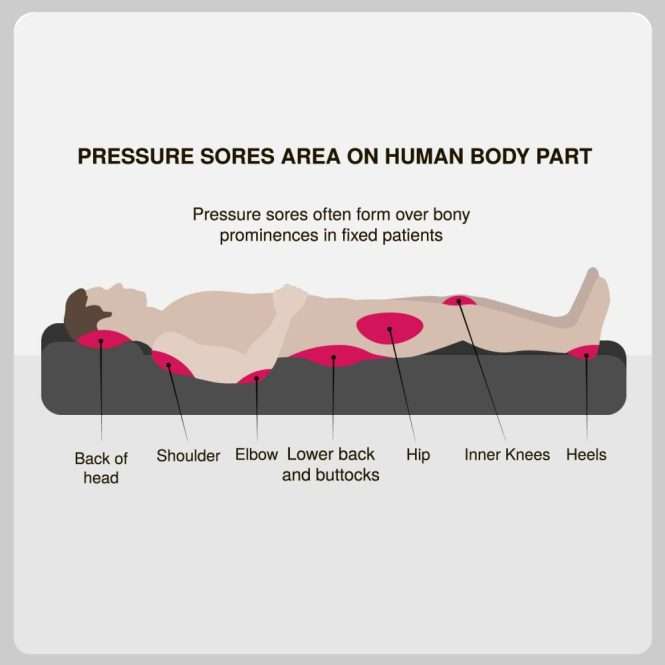
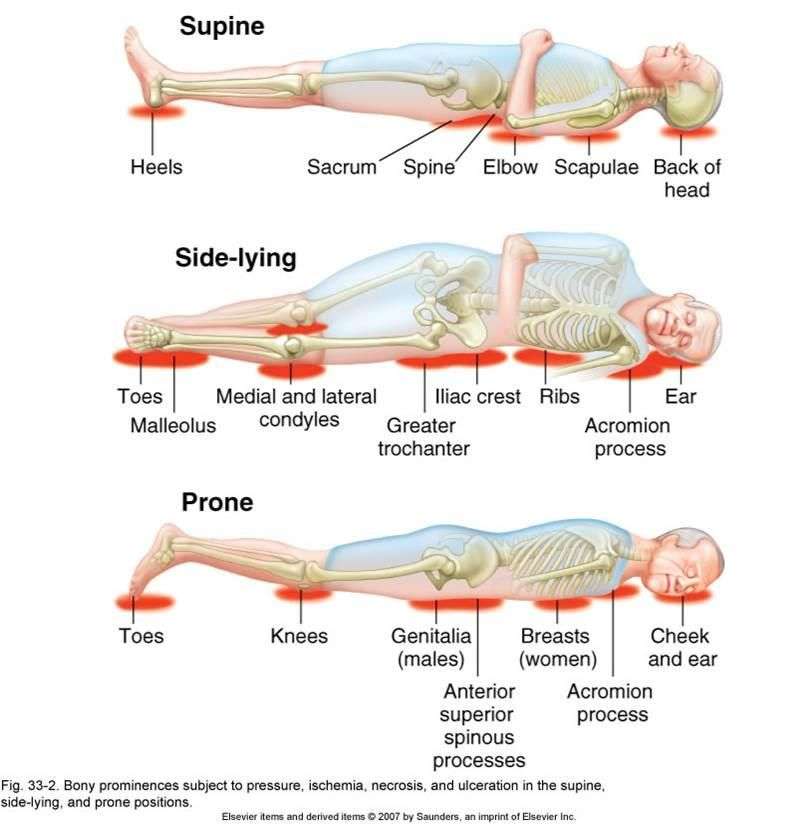
What Are Pressure Ulcers Or Sores
Pressure ulcers also known as bed sores, pressure sores or decubitus ulcers develop when the skin or tissue beneath the skin is damaged due to constant pressure or friction. Pressure ulcers often occur on bony areas, such as the heels and elbows. However, they can appear on any part of the body that is under pressure for a long time.
Pressure ulcers can be painful and uncomfortable and can take a long time to heal. They can also create sleep and mood disturbances, get infected and affect rehabilitation, mobility and long-term quality of life.
You should try to prevent pressure ulcers from forming if you are immobile or if you care for someone who is confined to a bed or chair.
Questions From The Doctor
Your doctor might ask questions such as:
- When did the pressure sore first appear?
- What is the degree of pain?
- Have you had pressure ulcer in the past?
- How were they managed, and what was the outcome of treatment?
- What kind of care assistance is available to you?
- What is your routine for changing positions?
- What medical conditions have you been diagnosed with, and what is your current treatment?
- What is your normal daily diet and fluid intake?
Don’t Miss: Wound Care Treatment For Diabetic Foot Ulcer
Treatment Of Decubitus Ulcers
Depending on the stage of the ulcer, treatment can include some or all of the following:
- Cleaning the ulcer and putting a dressing on the wound
- Meticulous wound care with frequent dressing changes
- Reducing pressure on the area by repositioning and using supporting surfaces
- Antibacterial drugs to treat infection
- Pain medications to relieve discomfort
- Debridement surgery to remove dead tissue from the ulcer
- Diet changes and increased fluid intake for faster recovery
What Is A Lateral Decubitus Radiograph

The term means lying down. Without qualification, the term is meaningless. A decub is obtained with the patient lying with his or her left or right side down. A right lateral decubitus radiograph is an image obtained with the patient lying with his or her right side down, the x-ray tube oriented in a horizontal position on one side of the patient, and the image capture device oriented perpendicular to the tube on the other side of the patient. To prevent any confusion, the best terms are right-side-down decubitus and left-side-down decubitus views, referring to the position of the patient.
Joshua Broder MD, FACEP, in, 2011
Recommended Reading: What Causes A Bleeding Ulcer In Stomach
What Causes Decubitus Ulcers
The main cause of decubitus ulcers is consistent pressure on the same area of the skin. This occurs for several reasons. In those who have been bed-ridden for a long period of time, the skin can break down from the constant pressure. Those with neurological and blood vessel diseases have an increased risk for this breakdown in skin tissue. Use of a wheelchair or a bedside chair also increases the risk for these ulcers, as the user remains in the same position for long periods of time.
No discussion of what causes decubitus ulcers would be complete without a discussion of the other risk factors for this condition. Those who have urinary incontinence or bowel incontinence have a greater risk for decubitus ulcers because of the moisture caused by incontinence. This moisture makes it easier for the skin to break down. Malnourishment may also lead to this type of ulcer because the patient does not get enough nutrients to build and maintain healthy skin tissue.
Enhancing Healthcare Team Outcomes
The main goal is to prevent a decubitus ulcer by decreasing the pressure acting on the affected site. This goal requires an interprofessional team, including primary care providers, wound care specialists, surgeons, specialty-trained wound nurses, physical therapists, and nurses aides. Nurses provide care, monitor patients, and notify the team of issues. Nurses aides are often responsible for turning and repositioning patients. Air-fluidized or foam mattresses should be used, frequent postural changes, provision of adequate nutrition, and treatment of any underlying systemic illnesses. Debridement should take place to remove dead tissue that serves as the optimum medium for the growth of bacteria. Hydrogels or hydrocolloid dressing should be used, which aid in wound healing. Tissue cultures are necessary, so the most directed antibiotic can be administered, which can involve the pharmacist and the latest antibiogram data. The patient should be kept pain free by giving analgesics. They should try to increase physical activity if possible, which a nurse’s aid, medical assistant, or rehab nurse can facilitate. Frequent follow-ups are an absolute necessity and a team approach to patient education and management involving the wound care nurse and wound care clinician will lead to the best results. These interprofessional activities can help drive better outcomes for patients with decubitus ulcers.
Also Check: How Can You Tell You Have An Ulcer