Tips For Preparing Nutritious Foods For Uc
Its one thing to know which foods are nutritious for you, but another to safely consume them. As one MyCrohnsAndColitisTeam member put it, The hard part is getting your nutritional requirements in with limited choices. Practicing meal planning and preparation techniques can be helpful to ensure adequate nutrition.
Members often share creative ways theyve found to incorporate nutritious foods into their diet safely. I made some pureed green sauce with greens, anchovies, garlic, and EVOO to add to roasted veggies and soups, said one. I have a Nutri Ninja. It purees my fruits and veggies, so I eat lots of smoothies with almond milk and Activia yogurt added, shared another.
It may also be helpful to purchase meal replacements, such as protein shakes, to keep your weight up. One member had a tip for weight gain: I increase the recipes that use lots of natural fats olive oil, coconut oil, coconut cream, avocado and I might increase my red meat. All of those make me feel super healthy.
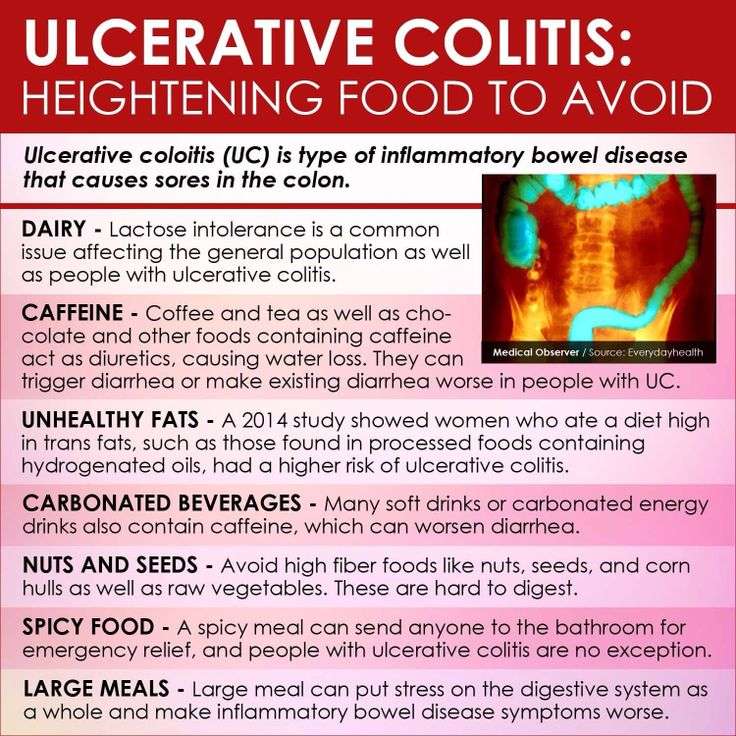
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
Pita Chips And Hummus
Hummus is made with mashed chickpeas, olive oil, and other seasonings.
The Crohns and Colitis Foundation recommend 1/4 cup of hummus and 2 ounces of pita chips as a snack.
To make hummus at home, a person can blend chickpeas, tahini, and a little olive oil together. They can add seasoning to taste but should avoid adding too much salt.
Even though it is high in fiber, pita chips and hummus can be a generally well-tolerated snack or small meal. The chickpeas in hummus may help symptoms in a person experiencing gas or bloating.
Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
Recommended Reading: What Is A Venous Ulcer
What Foods Should I Eat During An Ulcerative Colitis Flare
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut. Some of these include:
- White rice, bread, and pasta
- Crackers and cereals made with refined white flour
- Cooked veggies without the skin
- Tender, soft meats and fish
- Olive and coconut oil
- Lots and lots of fluids, since an ulcerative colitis flare-up can lead to diarrhea and thus dehydration
These foods have been found to be easily digestible in some ulcerative colitis patients, but be cautious when adding them to your diet since they can be triggers in other patients:
- Plain instant oatmeal
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut.
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
You May Like: Can Tylenol Cause Stomach Ulcers
Can Ulcerative Colitis Cause Rash And Skin Irritation
Swollen and painful areas of skin are common and affect up to 15 percent of individuals with UC. In general, skin irritation and rashes will get worse during a flare and resolve during periods of remission. These rashes oftentimes fluctuate in-line with the inflammation throughout your entire body. While most skin irritation and rashes are caused by Ulcerative Colitis inflammation, general UC symptoms do not always cause the irritation and rashes.
There are numerous skin conditions associated with Ulcerative Colitis, many of which are caused by auto-immune functions:
- Erythema nodosum
Learn more about these conditions and how to treat them in our full discussion on Ulcerative Colitis and skin irritation / rash.
Is Ulcerative Colitis And Autoimmune Condition
We are frequently asked whether Ulcerative Colitis it is an autoimmune condition. The short answer is yes, but its most important to understand what that means for your treatment plan.
With Ulcerative Colitis, the body recognizes harmless gut bacteria as an enemy and attacks the tissues in the colon. In a typical immune response, the body will send white blood cells to the area of illness or infection to help protect the body. After the body has combated the illness or infection, the inflammation will resolve.
However, in a colon affected by UC, the body continues to send white blood cells to the inner layer of the large intestine, which accumulate and continue to attack. This process causes a buildup of inflammation and can lead to sores, or ulcers, in the affected area. Because UC is recognized as an autoimmune condition, the treatment methods generally target the immune response within your body.
Medical Treatments for Ulcerative Colitis include:
Read our full discussion of Ulcerative Colitis autoimmune treatment options here.
Also Check: Bland Food Diet For Ulcers
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Read Also: Can You Donate Blood If You Have Ulcerative Colitis
Read Also: Calcium Alginate For Pressure Ulcers
What To Eat To Beat Ulcerative Colitis
by Executive EditorLouis Hansel
If you’re dealing with ulcerative colitis, you don’t need anyone to tell you how painful it is. Inflamed walls of the large intestine riddled with raw sores known as ulcers is no one’s idea of a picnic. Its no wonder that 70% of people suffering from UC, a type of inflammatory bowel disease , have tried elimination diets in an attempt to figure out how to ease the discomfort during flares. In fact, research suggests that the removal of certain foods from your daily repertoire, combined with the addition of beneficial ones, can play a big role in helping combat symptoms.
That approach is likely your best one, since the actual cause of UC remains elusive. “It is believed that a combination of factors may precipitate the onset, including genes, environmental factors like diet, stress, and smoking, immune system dysfunction, and imbalances in the gut microbiota,” says Ryan Warren, R.D.N. a clinical nutritionist at the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell Medicine and New York-Presbyterian. “Diet can play an important role in managing symptoms as well as maintaining adequate nutrition.” Heres what to eat to stay one step ahead of this painful disease.
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Recommended Reading: Home Remedies For Dog Mouth Ulcers
Finding The Right Uc Diet For You
For those living with ulcerative colitis, choosing the right foods to eat may feel overwhelming. If you are worried you may not be getting enough of one or more nutrients, speak with your gastroenterologist. They may test your blood for nutrient levels to find out whether you are deficient. If you are deficient in any nutrient, your doctor may recommend a safe and effective dietary supplement.
You can also request a referral to a registered dietitian who can work with you to get the most out of the nutrients in the foods youre able to eat. Working with a registered dietitian or nutritionist can also help you navigate life events, such as parties, dining out, vacations, and more. Understanding what triggers your flare-ups life stress or specific foods is important information that a food journal can help you decipher.
The good news is that for people with UC who establish a healthy and safe diet plan, sticking to it often helps them feel better and manage symptoms. Feeling pretty good today, wrote one MyCrohnsAndColitisTeam member. Ive gone lactose- and gluten-free, and symptoms have reduced a lot. Also gave up caffeine. Living on avocado!
You are not alone in your path to finding a safe and healthy diet with ulcerative colitis. When you join MyCrohnsAndColitisTeam, you gain a supportive community of more than 138,000 people living with IBD.
Recommended Reading: Compression Therapy For Venous Leg Ulcers
Can Certain Foods Really Cause Inflammation
The link between what we eat and chronic inflammation in the body isnt fully understood. What is known is that there does seem to be some connection.
Lets jump into the science: The liver produces something called C-reactive protein as a response to inflammation in the body. In short, higher levels of CRP mean more inflammation, and certain foods have been shown to increase levels of CRP in the blood.
Now, the specifics of what foods cause this increase is somewhat up for debate, but its possible that things like processed sugar can trigger the release of inflammatory messengerslike CRPa sign that they may potentially be contributing to an inflammatory state.
On the other hand, foods like fruits and vegetables may help fight oxidative stress, which is a trigger for inflammation. Certain diets, like the Mediterranean diet, already include many foods that are considered to be anti-inflammatory such as whole grains, legumes, a rainbow assortment of fruits and vegetables, and fish.
Also Check: Ulcerative Colitis Lower Back Pain
Do Grapes Trigger Ibs
Fruits contain the sugar fructose, which can cause issues for IBS sufferers. Fructose is particularly high in apples and pears, and somewhat high in watermelon, stone fruits, concentrated fruit, dried fruit and fruit juice. Fruits with lower levels of fructose include bananas, citrus, grapes and berries.
Dont Miss: Can Stress Give You An Ulcer
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
Don’t Miss: What Is Good For Ulcerative Colitis
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
Recommended Reading: Can Ulcerative Colitis Cause Body Aches
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
Also Check: Stage 3 Pressure Ulcer Treatment
Can You Eat White Bread With Ulcerative Colitis
Low-residue diet
Temporarily eating a low-residue or low-fibre diet can sometimes help improve symptoms of ulcerative colitis during a flare-up. These diets are designed to reduce the amount and frequency of the stools you pass. Examples of foods that can be eaten as part of a low-residue diet include: white bread.
You May Like: What Foods Should Be Avoided With Stomach Ulcers
What If Youve Had Surgery For Uc
If youve had surgery for UC, such as an ileostomy , your GI may give you specific guidelines regarding your diet and nutrition. For example, they may recommend you eat extra foods with vitamin B12 or take a supplement since removal of the ileum can make it hard for you to absorb the B12 you need. A lack of this vitamin can affect the health of your nerve and blood cells.
Its also extra important to stay hydrated if youve had surgery for UC, so make sure youre drinking lots of water and eating foods with a high-water content. Talk with your health care team and registered dietitian to understand how your surgery may affect your dietary needs.
Read Also: Whey Protein And Ulcerative Colitis
Read Also: What Can Help Stomach Ulcers
Choose Fish With Omega
Scientists have not yet come to a consensus about whether or not eating red meat has any effect on people with UC, but the nutrients in fish could be beneficial. Consuming foods like fatty fish, which are rich in omega-3 fatty acids, may help with UC-related inflammation, says Diekman.
Omega-3 fatty acids are a crucial nutrient your body uses to make cells and hormones that regulate blood clotting. While some studies have shown that omega-3 fatty acids are anti-inflammatory, more research still needs to be done to prove theyre beneficial. According to the National Institutes of Health , omega-3 fatty acids, like probiotics, also support the immune system.
Unlike other fats, the body cant make this good fat on its own from other raw materials. Instead, you must get it from food sources, including fish like salmon, herring, sardines, rainbow trout, and mackerel just refrain from frying fillets, since fatty or greasy foods can exacerbate UC symptoms.
What Is An Ulcerative Colitis Diet
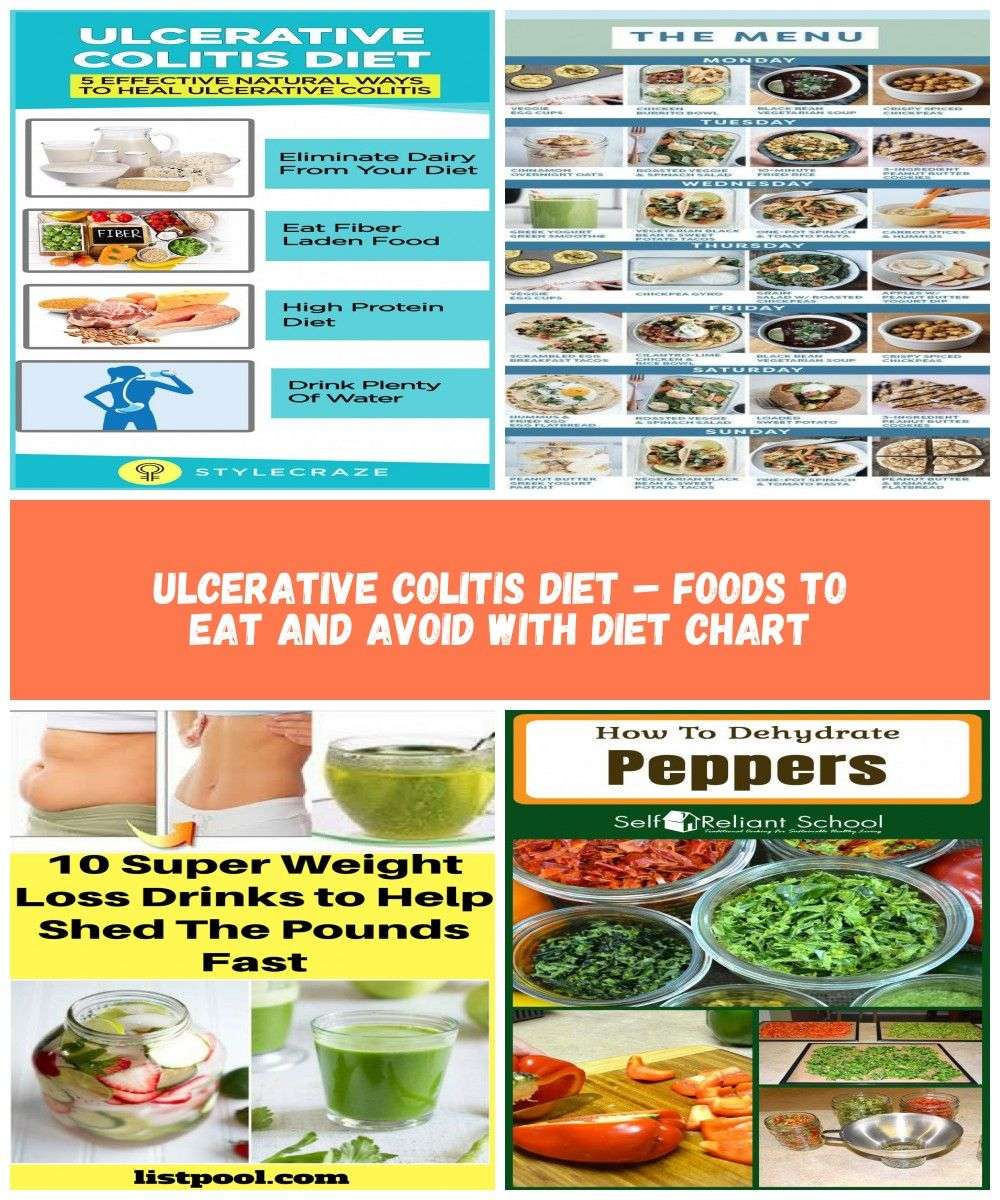
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Recommended Reading: Does Aloe Vera Help Ulcerative Colitis