Protect The Periwound Skinexpand: More
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or bodily fluids, to protect sensitive, fragile skin and severely dry skin, including peri-wound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab and Askina® Barrier Film Spray are sterile liquid dressings intended to form a uniform, transparent film when applied to the skin. The film can provide oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Description
- Manage bacterial load and odor
- Manage exudate and promote moist healing
- Protect the periwound skin
The Challenge To Manage Pressure Ulcers
We all want to avoid pressure ulcers. Considerable progress has been made in this area the past few years. Nevertheless, pressure ulcers remain a challenge. B. Braun offers different solutions including products for skin care, wound bed preparation and infection management, as well as exudate management. Taking action right from the start helps you to prevent the aggravation of existing pressure ulcers and to support the healing process.
Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The OMeara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Read Also: How To Treat Gum Ulcers
Also Check: Mouth Ulcers Treatment Home Remedies
Failure Of Reactive Hyperaemia Cycle
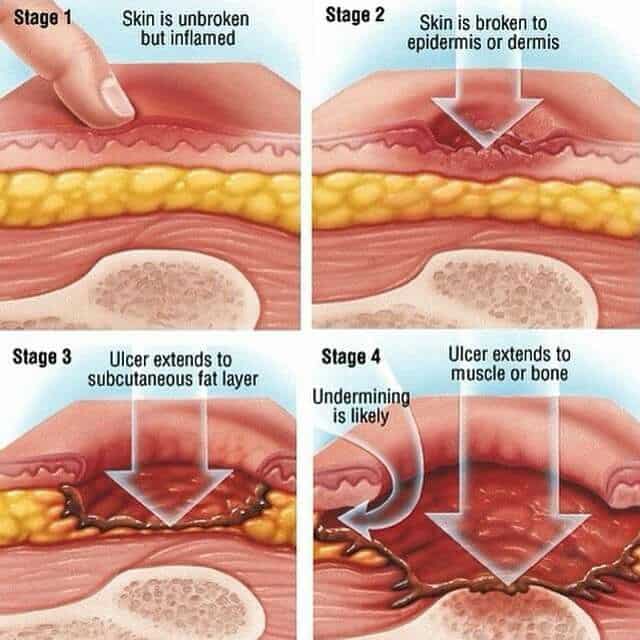
It is a known fact that tissue distortion causes ischaemia that in turn stimulates protective movements to relieve pressure and circulatory activity to restore normal blood flow in the affected areas. These protective movements are often reflexes as the person is unaware of making them. However, if these prompt actions prove insufficient to relieve ischaemia, the central nervous system is stimulated by constant signals of discomfort and pain to make sure that the pressure is relieved before any permanent damage occurs. Once the pressure is relieved, and the circulation restored, local capillaries begin to dilate and increased blood flow takes place, referred to as reactive hyperaemia. As a result, a bright pink transitory patch appears on the skin, often called blanching erythema because it blanches on pressure unlike the dull red non-blanching erythema that indicates tissue damage . Reactive hyperaemia ensures a rapid restoration of oxygen and carbon dioxide balance it also flushes out waste products. Erythema subsides as soon as tissues are restored to their resting state.
Various grading of pressure ulcer . A very severe trochanteric pressure ulcer where destruction is so severe that the femoral head dislocated and came out
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Recommended Reading: How Do You Know If You Have A Stomach Ulcer
Diagnosing A Stage 3 Bedsore
A medical professional relies on a bedsores appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patients skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough or eschar in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
You May Like: What Foods Not To Eat If You Have An Ulcer
What Kind Of Dressings Are Used For Pressure Ulcers
Foam Dressings . Stage III Pressure Ulcer. Open wound that breaks through all skin levels Visible fat layer, but not bone, tendon or muscle Wound may begin expanding under adjacent intact skin Foam Dressings . Hydrogels . Hydrocolloids. Alginate Dressings. Stage IV Pressure Ulcer. Open wound that exposes bone, tendon or muscle
Don’t Miss: What Are The Warning Signs Of Ulcerative Colitis
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
Searching other resources
What Are The Complications From Stage 2 Pressure Ulcers
Stage 2 pressure ulcers, when left untreated, can advance into deeper skin tissues, resulting in stage 3 and 4 ulcers which are harder to treat and may be fatal. Infection in pressure ulcers can spread to the blood and bones, resulting in sepsis and osteomyelitis. When deeper tissues are involved, it may cause permanent tissue damage that may never heal completely even with treatment. Pressure ulcers increase the risk of urinary tract infections , amputations, and autonomic dysreflexia.
Stage 2 pressure ulcers are open wounds on the epidermis of the skin. Proper care given when the stage 1 pressure ulcer is diagnosed can prevent progressing to stage 2 pressure ulcers. Frontline caregivers play an essential role in screening, assessing, and managing pressure ulcers. Healing and prevention of pressure ulcers in critically ill patients are crucial. Early referral and treatment improve the outcome of the risk of pressure ulcers.
Query:Hello doctor,I have general head pressure and I suspect brain problem. GP seems to treat my symptoms as we struggle to find the root cause. My concentration level seems impaired, though not severely. I get feelings like I would pass out at times.I get weak joints at times (hands, kn… Read Full »
Most Popular Articles
Also Check: Ulcerative Colitis And Lung Disease
One To Four Out Of 10 Hospitalized Patients May Develop Pressure Ulcers
Defloor T, De Bacquer D, Grypdonck MH ‘The effect of various combinations of turning and pressure reducing devices on the incidence of pressure ulcers.’
Thorough wound assessments and sensible product selections are essential to help prevent and treat wound infections, manage exudate and finally restore skin integrity. This is the clinical case presentation of Fernanda Cortes from Chile who explains step by step how she treated the stage 3 pressure ulcer of a 60-year-old family father. Through her commitment and the effective combination of Prontosan®, Askina®and Linovera®the patient eventually recovered.
Please note that the pictures in the video may be disturbing to sensitive persons.
In the following video, Miguel Cuevas shares his joy of his recovery. He is happy to be able to do all the things again that most people take for granted.
How Do I Use Medihoney
Before applying a MEDIHONEY product to your loved ones wound, carefully read the instructions on the packaging. Once you do, follow these simple steps:
-
Thoroughly clean the wound with a saline solution. . Then, if necessary, apply a barrier cream around the edges of the wound. Barrier cream prevents skin breakdown and infection.
-
Apply the MEDIHONEY gel or paste directly to the wound. If youre using a calcium alginate dressing, use sterile scissors to resize it, and then gently apply the dressing to the wound bed.
-
Cover the MEDIHONEY gel, paste, or alginate dressing with an absorbent sterile, secondary bandage or a compression garment.
-
When its time to change the dressing, thoroughly clean the wound with a saline solution. Once you do, repeat the same steps.
This video by YouTuber Alyssa McTavish demonstrates the entire process:
Keep in mind that its best that MEDIHONEY be on the skin for 12-24 hours at a time for maximum effectiveness. If you or your loved one is having a hard time keeping the dressing intact, soak a gauze dressing in the MEDIHONEY and apply it directly on the wound, then top with an abdominal pad dressing.
Also Check: Does Ulcerative Colitis Increased Risk Of Colon Cancer
Also Check: Over The Counter Medicine For Ulcerative Colitis
What Is A Stage 4 Bedsore
Stage 4 bedsores are the most severe form of , also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
A stage 4 bedsore may be an unfortunate sign of . Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
Thankfully, financial compensation may be available if your loved one develops a stage 4 bedsore while living in a nursing home. Get a free case review to see if you can pursue compensation to help pay for medical treatment.
Victims of stage 4 bedsores can take legal action.
to learn if you can access financial aid and hold abusive nursing homes accountable.
What Are The Stages Of A Pressure Injury
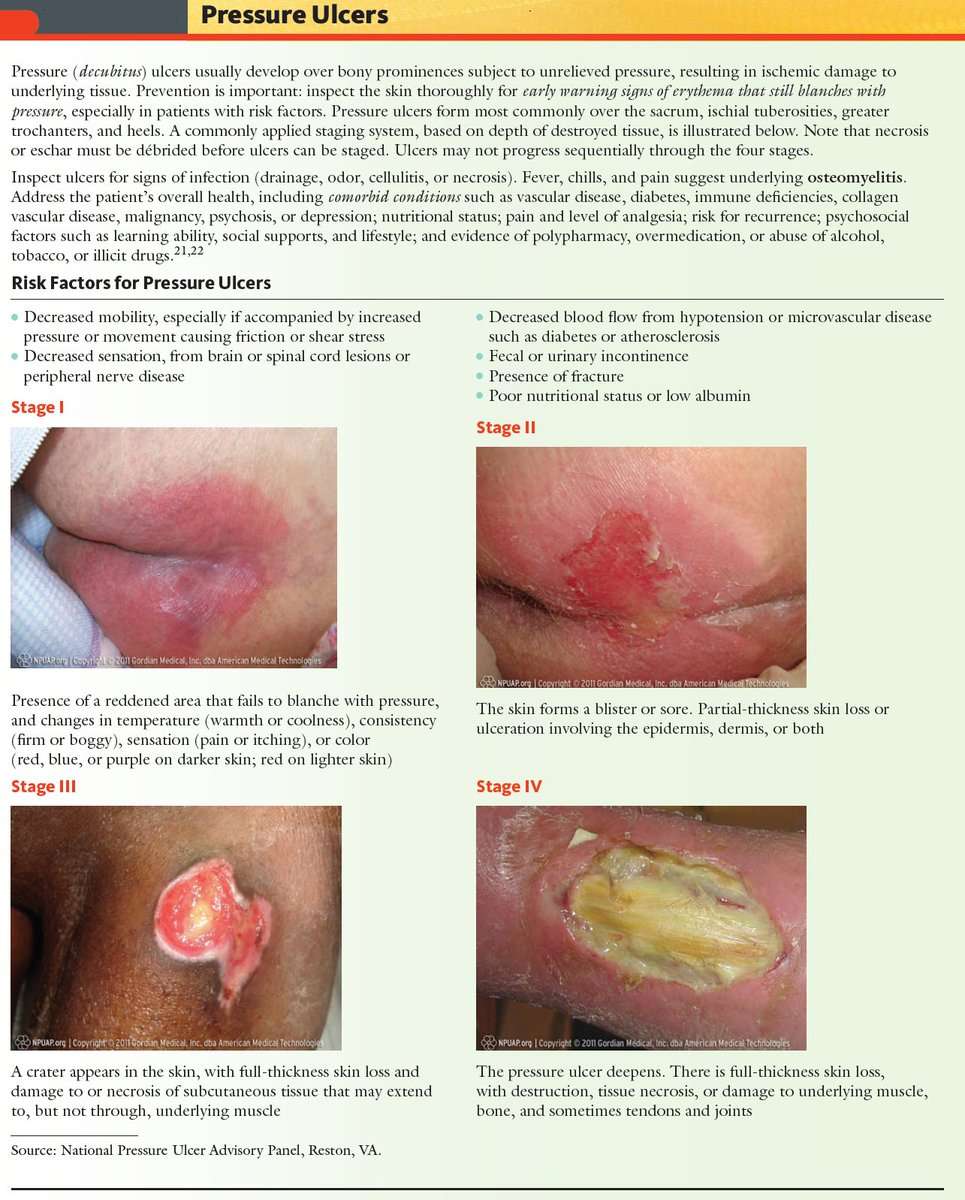
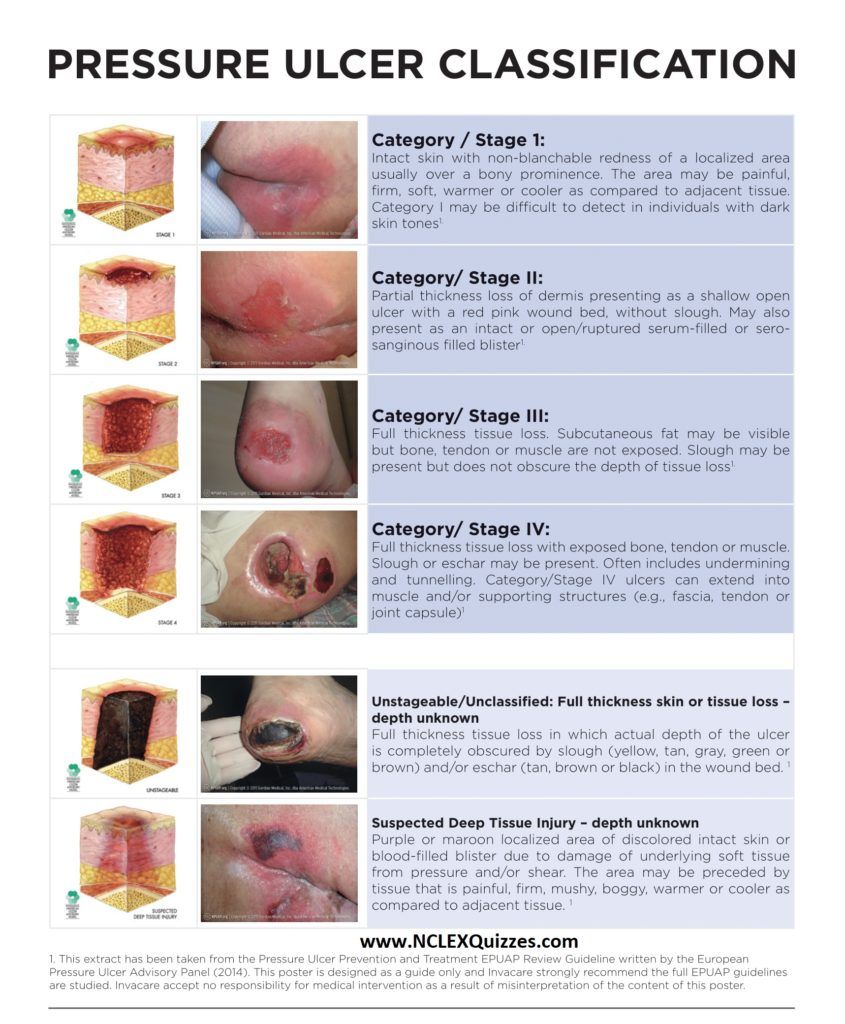
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Recommended Reading: Vulvar Ulcers Not Std Pictures
Treatments Your Physician May Prescribe
In addition to self-care, your doctor might prescribe special pads or mattresses. Special dressings may be used, and whirlpool baths or surgery may be recommended to remove dead tissue. Infection requires antibiotic treatment. Sometimes deep wounds may require surgery to restore the tissue. Experimental work is now being done using honey preparations, high-pressure oxygen, and application of chemicals that stimulate cell growth .
Recommended Reading: Can You Drink Ensure With Ulcerative Colitis
What Are The Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are open, shallow, broken wounds with a red base. Intact or incompletely ruptured blisters may also be present with clear fluid or pus seeping from the affected area, and the skin to it adjacent may be discolored. It may involve both the dermis and epidermis of the skin.
Stage 2 bedsores are common in ankles and heels, back of the head, hip, shoulder blades, and tailbone. However, it can develop in any part of the body under constant pressure. Still, areas near bones are at a higher risk.
There is more significant pain in stage 2 bedsores than in stage 1 bedsores. The pain decreases as the sore worsens but becomes harder to treat, leading to fatal complications.
Also Check: Best Smoothies For Ulcerative Colitis
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Posthoc Sensitivity Analysis Dressings Only
For the individual network, we also investigated, posthoc, our original assumption that topical agents could be used in place of dressings, by examining only the network of studies involving two or more dressings . There were no threearm trials remaining and the 30 studies compared 12 interventions in a total of 1627 participants experiencing 641 events, with 16 direct contrasts and 66 mixed treatment contrasts. The NMA rankings were similarly imprecise .
For the group network, 17 studies compared five interventions in a total of 798 participants experiencing 304 events, with five direct contrasts and 10 mixed treatment contrasts. This network was still sparse in terms of total participants, but, on average, there were more events per contrast. The posthoc sensitivity analysis had less overlap of rankograms than the full group network, and the mean rank was closer to a whole number one SUCRA value was 0 and another was 0.9. The mean ranks were: proteasemodulating 1.4 advanced 1.9 basic 3.1 antimicrobial 3.7: advancedantimicrobial 4.9. For the comparisons with basic dressing, effect estimates were similar to those in Table 4 but CIs were still wide.
Read Also: Can You Take Tylenol With A Stomach Ulcer
What Are The Benefits Of This Treatment
It can take several months of bedrest for a severe wound to heal on its own. All pressure must be off the area while in bed, which can be very hard to do on an ongoing basis. If pressure is put on the area while in bed, it can delay healing or make the wound worse. Plus, there is an increased risk of infection with any open wound. The longer the wound is open, the longer the higher risk continues. If an infection develops, there is a risk that it can spread and become life-threatening.
The obvious benefit of this treatment is that the wound can heal much quicker than it would without the treatment. Your doctor can explain all your benefits, but here are a few of the benefits:
- Much less time needed for bedrest
- Lowered risk for infection
- Increased independence to enjoy meaningful activities
- Lowered healthcare costs
Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
You May Like: Does Ulcerative Colitis Make You Tired
The Efficacy Of Duoderm
A study by Michel Hermans treating small partial-thickness burns found that HydroColloid Dressings provide an optimum wound environment for more rapid re-epithelialization than either allografts or SSD. The cosmetic and functional results were also excellent.1 A meta-analysis of pressure ulcers performed by Matthew Bradley comparing a hydrocolloid dressing with a traditional treatment suggested that treatment with the hydrocolloid resulted in a statistically significant improvement in the rate of healing compared to wet-to-dry dressings.2
How Do You Treat Pressure Sores On The Buttocks
Pressure sores on the buttocks are treated by proper wound care and by repositioning to remove the pressure source, states ClinicalKey. Pressure sores on the buttocks are due to long periods of uninterrupted pressure on the skin, soft tissue, muscle and bone.
There are four stages of pressure sores, according to ClinicalKey. The first stage is redness of the skin, and the second stage is partial thickness skin loss involving the epidermis and dermis. The third stage is full thickness skin loss involving the subcutaneous tissue. The fourth stage involves muscle and bone.
Prevention is the most important factor in managing pressure sores, explains ClinicalKey. For necrotic, deep and poorly healing wounds, surgical debridement may be necessary. If infection of the soft tissue or bone is present, antibiotics are needed.
Pressure sore develop in people who are chair- or bed-bound, elderly patients, hospital inpatients and people with spinal cord injuries, notes ClinicalKey. Those who are more predisposed to developing pressure sores are patients with conditions causing poor wound healing, such as diabetes and nutritional insufficiency, and those with conditions causing low tissue oxygen tension. People with fecal or urinary incontinence are also more prone to developing pressure sores, as urine and feces act as skin irritants to break down skin.
Dont Miss: Best Nsaid For Stomach Ulcers
Read Also: Foods Not To Eat With Ulcerative Colitis