Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Mixing Tolterodine With Herbal Remedies And Supplements
There might be a problem using herbal remedies and supplements while taking tolterodine.
Some herbal medicines can make you feel sleepy, cause a dry mouth, or make it difficult to pee. Their effect is similar to tolterodine. This can increase your risk of getting side effects or make your side effects worse.
Surgery For Ulcerative Colitis
Despite drug therapies, approximately one-third of people with ulcerative colitis will need surgery to treat the inflammation, prevent or treat cancer, or to treat a complication such as rupture of the colon. Surgery in which the entire colon is removed cures the person of their ulcerative colitis. In the past they were left with ileostomies, external bags into which the small intestine emptied. Surgical techniques have been developed, however, that now allow the colon to be removed without the need for an ileostomy.
Recommended Reading: Best Pain Relief For Leg Ulcers
Can Ibs Cause Blood In Urine
Symptoms of IBS may be present in many illnesses, such as infections. However, noticing blood in the urine is often a sign of an infection in the urinary tract.
If any blood is noticed in urine or stool, it often best to inform a GP who may like to investigate further.
Other possible causes of blood appearing in urine include kidney stones and an enlarged prostate.
Dosage For Tolterodine Slow

The usual dose for adults taking slow-release tolterodine capsules is 4mg once a day.
Children will usually take between 1mg and 4mg a day.
If you have kidney or liver disease, or you’re affected by side effects, your doctor may reduce your dose to 2mg once a day taken as tablets.
Take the capsule at the same time each day. This will help you to remember to take them.
Read Also: Is Burping A Sign Of An Ulcer
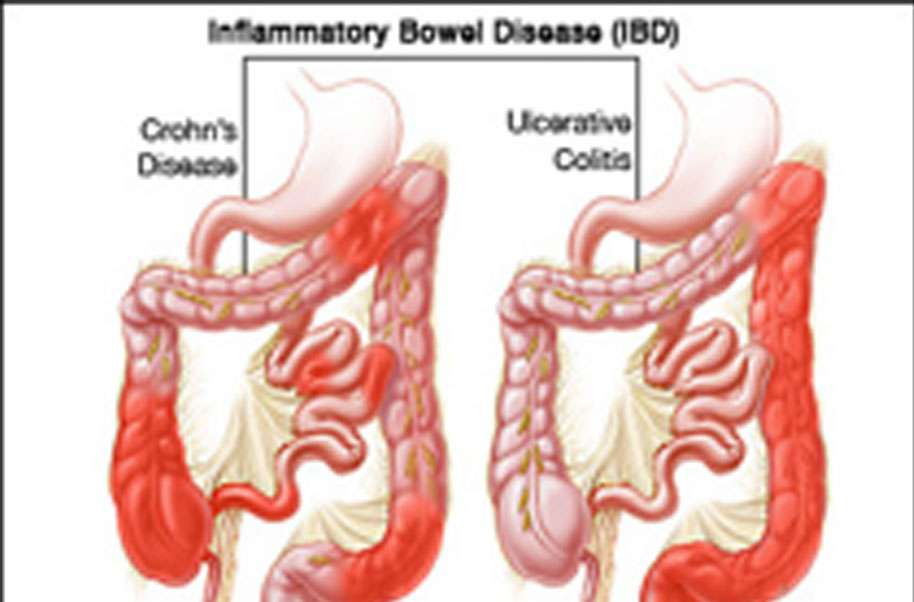
Colitis And Crohns Disease And Constipation
Constipation can sometimes occur in those with Colitis and Crohns Disease.
Generally, increasing fibre intake is a good self-help method to relieve the symptoms of constipation, however this is not always the case for people with Colitis and Crohns Disease. For some, fibre could be the cause of constipation and can even make the symptoms worse. Moderating or even reducing fibre intake until symptoms improve or disappear could help. For others dairy foods could be the problem, everyone is different so its always best to find out what triggers it for you.
Keeping a bowel diary is an effective way to see which foods and beverages set off your symptoms. If you keep the diary for a couple of weeks you will get a good idea of which foods and drinks youll need to avoid and then you can start to use this information when planning your meals.
If your symptoms persist, its always best to speak to your GP for advise as they should be able to recommend other methods which you can use to help ease your symptoms.
What Are The Symptoms Of Urinary Retention
- Difficulty starting a urine stream
- Weak flow of urine
- Feel the need to urinate after voiding
- Small amount of leakage
For acute bladder retention, initial treatment will involve catheterization, a small tube inserted into the bladder through the urethra to drain the urine and relieve immediate pain and distention. Long-term treatment will depend on the cause.
You May Like: How Can You Prevent Pressure Ulcers
Years Before My Diagnosis
Ive suffered from what were thought to be recurrent bladder infections since my late teens, often needing several courses of antibiotics in a space of a month. I was both working and attending college at the same time, and was very conscious of being unreliable, so my flares were both a worry and an inconvenience.
If an infection flared while I was actually at work, Id go and get antibiotics, drink as much water as I could, lie down in the tearoom for a while and then return a few hours later when I started to get some relief.
I adapted, wearing loose clothing, drinking a lot of water and making sure I had always had a bottle of Potassium Citrate solution to hand. These things all helped, but nothing stopped the seemingly regular flares.
At one point, my GP referred me to the local hospital to have scans on my bladder to check that it was emptying properly, but when those scans showed nothing abnormal, I carried on the same as before. The infections just became part of my normal way of life.
Taking Care Of Your Mind
Taking care of your mind, as well as your body shouldnt be a luxury or an afterthought. Unless burning out or feeling a lot worse is what youre shooting for, its important and necessary.
We now live in a world where were always switched on but try your hardest to slow down and set some time aside for yourself at least semi-regularly. It makes the biggest difference. A small amount of time each day is perfect , but anything is better than nothing.
See Lucilles work here:
If you would like to share your story on BBUKs blog please send an email to: bbuk@disabledliving.co.uk
Don’t Miss: How Would You Know If You Had A Bleeding Ulcer
How To Treat A Uti While On A Biologic
Most women are familiar with the telltale signs of a UTI, like the burning sensation while urinating, and the urge to go more often.
If youre experiencing these UTI symptoms, be sure to call your doctor. Its important to work with your care team to determine the underlying cause of the infection as it may not necessarily be related to your IBD treatment. The risk of UTI may not be the same for all biologics, says Dr. Aberra. However, if someone is having an infection that they didnt previously have, and theyre noticing that its recurring often or they cant really clear the infection, it could be related to immunosuppression.
UTIs are commonly treated with antibiotics, and symptoms often improve within a few days of treatment. However, if UTIs keep coming back, be sure to talk to your gastroenterologist. Your primary care physician is the one that will treat the UTI, but if its becoming recurring, also be sure to tell your gastroenterologist so they can help figure out what to do with your IBD treatment, adds Aberra. You may need to lower your dose or change the interval to give your body a break.
Uc Treatments And Urinary Changes
Sometimes, UC treatments can affect urinary habits. Corticosteroids such as prednisolone may cause urinary changes in people with UC. This medication usually causes someone to pee less, but it can also cause someone to pee more often.
Several members have noticed this effect. Has anybody ever experienced frequent, urgent urination whilst on prednisolone? asked one member. I am definitely peeing more often, but the urgency at which I need to get to the bathroom to have a pee is a bit worrying. Another member mentioned that they had experienced this effect. When I take prednisone or budesonide, I urinate much more frequently, which is a known side effect of steroids.
Using high doses of steroids or using steroids for a long time can sometimes lead to problems with the adrenal glands small organs that make hormones to regulate many body processes. Frequent urination can be a sign of this issue. Other symptoms include dizziness, a fast heart rate, irregular heartbeats, blurry vision, or feelings of weakness. Tell your doctor if you notice these symptoms while taking steroids.
Several other health conditions unrelated to UC could also lead to increased urination. They include:
- Bladder stones
- Prostate problems, including prostatitis or benign prostatic hyperplasia
- An overactive bladder
- Interstitial cystitis, also known as painful bladder syndrome
Also Check: Easy To Digest Foods For Ulcerative Colitis
Bladder Symptoms And Ibs
IBS is a group of symptoms, notably abdominal pain and changes in bowel habits. The condition doesn’t damage your digestive system, but it often affects your quality of life.
IBS doesn’t cause urinary problems directly. But many of the same triggers for IBS, including stress and infection, are believed to play a role in urinary problems.
The bladder symptoms often experienced by people with IBS include:
- Frequent urination
- Incomplete emptying of the bladder
- Nocturia
- Urinary urgency
Women with IBS may be more likely to experience urinary incontinence and overactive bladder than women without IBS.
A 2012 study from Asahikawa Medical University in Japan reported that 33.3% of people who had IBS had overactive bladder as well. Women were affected slightly more frequently than men.
It isn’t known for sure why people who have IBS are at higher risk for urinary problems and vice versa. Sometimes improving one of the two problems may lead to an improvement in the other.
Since the bladder and bowel are close together, there could be interaction between some of the nerves and muscles.
Other possible reasons could be inflammation around the bladder and bowel, or a nervous system issue affecting the whole region.
Are Bladder Problems Common In People With Ibs
When someone is suffering from IBS, in addition to the symptoms of bloating, cramping and changes in bowel patterns, symptoms can also start appearing outside of the digestive system.
Its been indicated that issues such as migraines, depression, fibromyalgia and bladder issues can also co-exist with IBS.
Don’t Miss: Ulcerative Colitis And Lung Disease
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Dont Miss: What To Do When Ulcerative Colitis Flares
Does Drinking Water Help Uc
Its important to drink water when you have UC. Having enough fluids will replenish what you lose through diarrhea.
Water alone may not be enough. Your body also loses electrolytes like salt, potassium, and magnesium when you have diarrhea.
Drinking water plus electrolytes can help you stay hydrated. You can find that combination in the form of an oral rehydration solution at your local pharmacy. Sports drinks such as Gatorade and Powerade also contain electrolytes and fluid.
Read Also: How To Get Rid Of Corneal Ulcer
Living With Uc: Supplements
The bleeding caused by ulcerative colitis may lead to iron deficiency anemia due to the loss of the body’s store of iron in the red blood cells that are lost into the colon. Iron supplementation may be necessary. Medications used to treat ulcerative colitis may reduce the absorption of nutrients such as folic acid and calcium. Supplements of vitamins and minerals may be necessary.
Retrograde Labeling Of Bladder Afferent Neurons
Bladder afferent neurons were specifically labeled by conventional neuronal tracing dye Fast Blue in live animals through surgery as described previously . Briefly, the rat urinary bladder was exposed with a lower abdominal incision under anesthesia . FB was injected into 10 sites in the muscular wall of the bladder to label bladder afferent neurons in the DRG. Sterilized Hamilton syringe was used for injection. To prevent leakage and labeling of adjacent tissues, a cotton swab was used, close to the injection site, to wipe off any excess dye that might leak during needle withdrawal after each injection. We also avoided to inject dyes into the lumen, major blood vessels, or overlying fascial layers. The incision was closed with 40 sutures. The surgeries were done 7 days prior to harvest of tissues. We also checked the leakage of the dyes by examining the bladder and surrounding tissues after euthanasia of the rats. No contamination was found.
Read Also: Medihoney For Stage 1 Pressure Ulcer
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Dont Miss: Treating Hindgut Ulcers In Horses
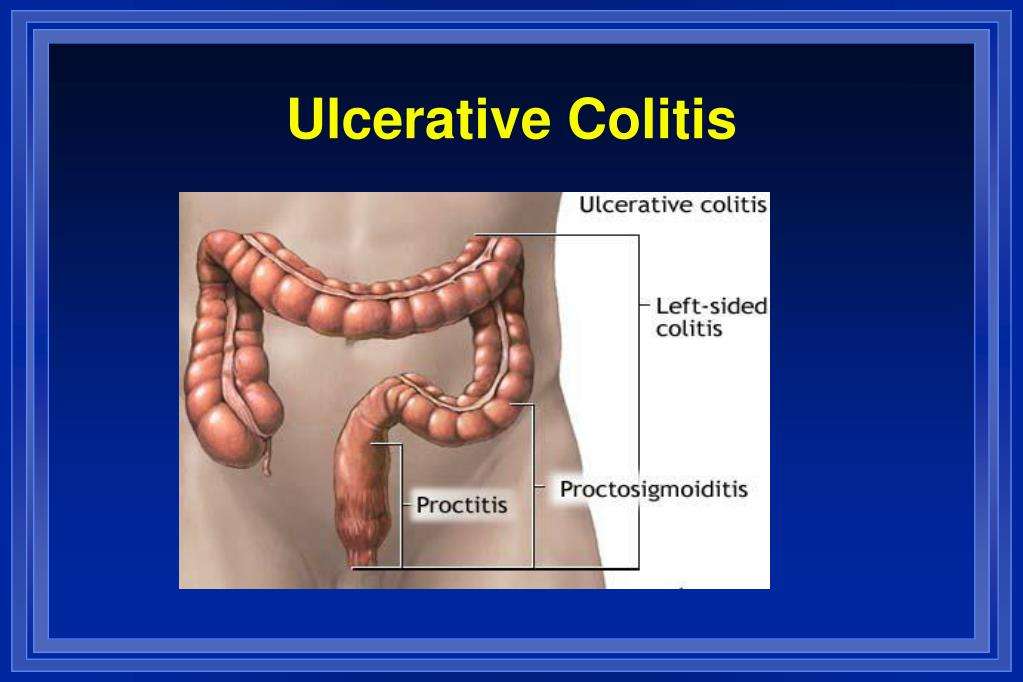
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Read Also: What Does A Ulcer On The Leg Look Like
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Who Is At Risk For Ulcerative Colitis
Some things may make you at higher risk for ulcerative colitis. These include your:
- Age. The disease most often starts when you are between the ages of 15 and 30 years old.
- Family history. Having a family member or close blood relative with ulcerative colitis raises your risk of the disease.
- Race and ethnicity. It happens more often in white people and people of Jewish descent.
Recommended Reading: Foods To Avoid With Peptic Ulcer
Read Also: Ulcerative Colitis And Anxiety Attacks
T Cell Isolation And Stimulation
Peripheral venous blood was obtained from healthy volunteers in compliance with the AIIMS Institutional ethics committee protocols. Peripheral blood mononuclear cells were separated by Ficoll-Paque plus gradient centrifugation. The PBMCs were stained with CD4- Allophycocyanin , CD25-phycoerythrin-Cy7 and CD45 RA- Phycoerithrin . Naive T cells were sorted by high speed flow cytometry with FACS AriaIII to > 95% post sort purity. Cells were cultured at 105 cells/well in a 96 well U bottom plate for 6 days in serum free X vivo medium and stimulated with plate bound anti CD3 and soluble anti CD28 . In Th polarization assay, at the start of the culture, cells were differentiated with recombinant IL-2 for Th0, TGF1 , IL-1 , IL-6, IL-21 and IL-23 for Th17 in the presence and absence of potassium chloride.