What Are Ulcerative Colitis Treatment Options
Depending on the location and severity of your case of ulcerative colitis, there are different treatments that can help you feel better. For a long time, corticosteroids were the main form of medical treatment for IBD, but they can potentially have adverse effects when used long-term. With more research, options like immunosuppressants arrived. According to the Centers for Disease Control and Prevention , the newest type of medication approved for the treatment of IBD is biologics. These medications are made from living thingsrather than chemical compoundsand work to target proteins made by the immune system to reduce inflammation. If medication isnt effective, surgery is also an option.
Dr. Sinha emphasizes that keeping your health care team informed is key to managing ulcerative colitis. Having this regular communication helps facilitate labs, imaging, or endoscopy that may be necessary, he says. It also allows the providers to understand many other facets of the disease’s impact on the patient, such as the psychosocial impact.
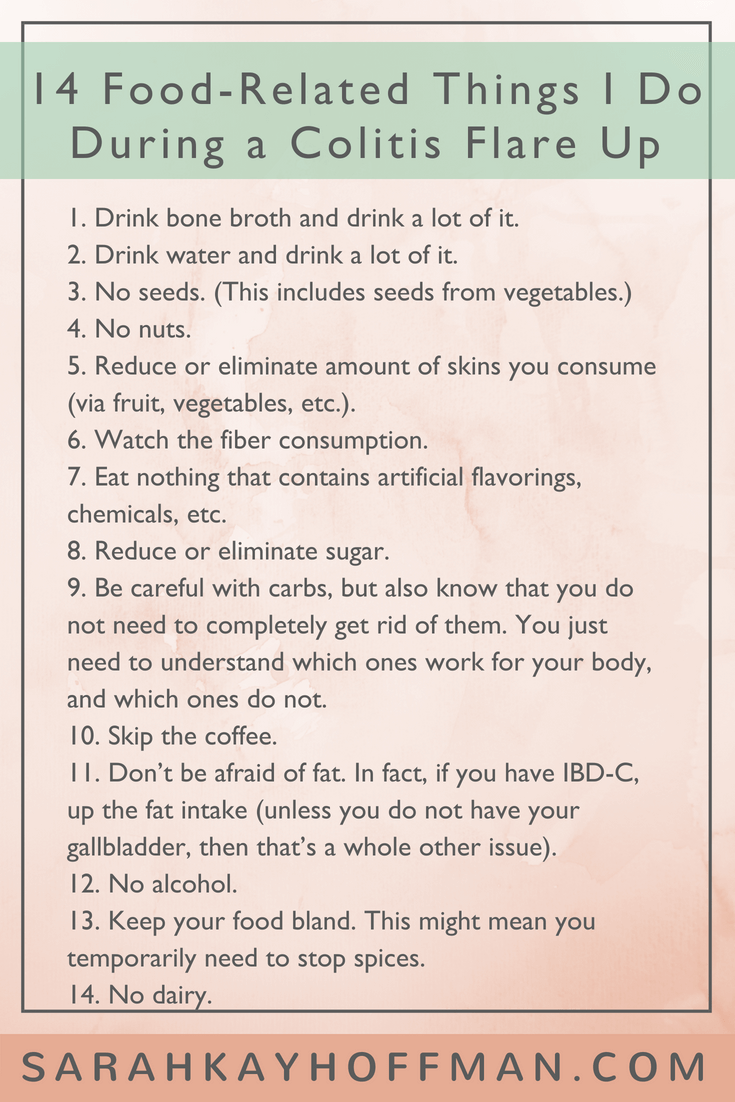
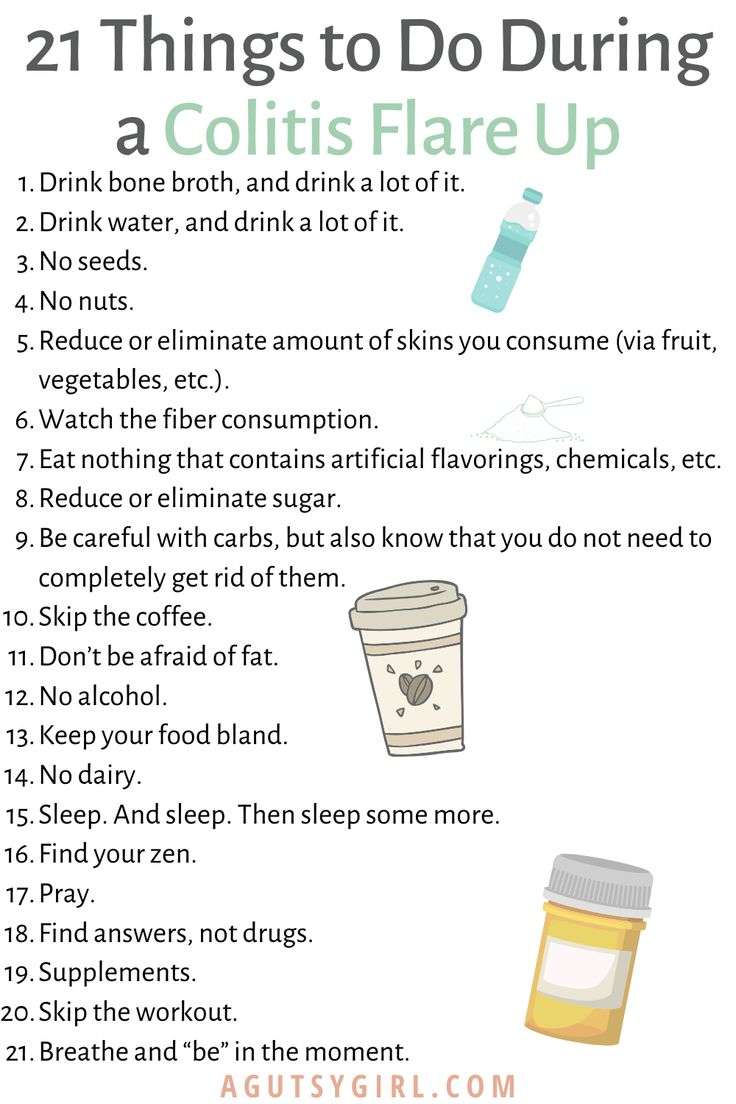
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Don’t Miss: Pressure Ulcers Are Most Likely To Develop
Experimenting To Find Out What Can Or Cannot Work For Me
Ive had IBD for five years now and Im slowly learning that I need to adapt and work with my body each day rather than oppose blanket rules. So if youre reading this article, Id encourage you towork with your body too and slowly experiment to see what you can tolerate.
Of course, chronic illness or not, alcohol daily is not great for any of us. But its important that we also try to live our lives and not beat ourselves up about our decisions and indulging occasionally
Of course, I should add as a final note, working with yourself is great but working with your doctor is just as important. With some of the medications we take, we must make sure no alcohol passes our lips at all. And, if we are in a flare, than any kind of alcohol is likely to make it worse.
Id love to hear about your experiences with IBD and drinking.
Have you managed to find a solution that works for you or have you just given it up altogether? Is it just me who finds some types of alcohol can impact me much more than others? And finally, does anyone else just really miss wine? Do let me know below!
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
- Monosaccharides
- Polyols
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Recommended Reading: How Long Does Ulcerative Colitis Flare Up Last
Find Your Support System
MyCrohnsAndColitisTeam is a community of more than 138,000 members who understand living with inflammatory bowel disease. Members share tips for managing flares and offer each other support and encouragement.
Do you struggle with UC flares? What has worked for you? Share your tips in the comments below, or on MyCrohnsAndColitisTeam.
Ulcerative Colitis In Children
Without proper care, pediatric ulcerative colitis will result in slower than normal growth and/or stunted growth.Intestinal inflammation lowers a childs appetite, which mean less food is eaten resulting in fewer nutrients to support healthy growth. Supplements are often a good idea as is making sure that enough calories are consumed, which sometimes requires a high-calorie diet for some kids. Additionally, a therapy or counseling may be sought to help a child develop the tools to cope with their disease.
Recommended Reading: Wound Care Treatment For Diabetic Foot Ulcer
What Is Ulcerative Colitis Exactly
Ulcerative colitis is one of the two main forms of inflammatory bowel disease . The other is Crohns disease. U.C. occurs when the immune system malfunctions, causing inflammation and ulcers to appear on the inner lining of the large intestine, according to the National Institute of Diabetes and Digestive and Kidney Diseases . Its not comfortable, to put it mildly, and not something that will clear up quickly.
Ulcerative colitis is a chronic illness that does not yet have a medical cure. That doesnt mean nothing can be done though, so dont despair if youre experiencing symptoms. Sidhartha Sinha, M.D., a gastroenterologist, assistant professor at Stanford Medicine, and researcher who specializes in IBD, tells SELF that while there arent medical cures for ulcerative colitis, there are medical treatments. And we have made great advancements in these treatments, he says. The last resort is a surgical option called colectomythe removal of the entire colonwhich can eliminate U.C. entirely.
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Read Also: How Is Ulcerative Colitis Caused
Youre Drinking Caffeine Or Alcohol
Coffee, tea, and sodas can make UC flare-ups worse, says Yun, because caffeine is a stimulant that can get your intestines going not what you need when you have diarrhea. The same goes for beer, wine, and liquor. People with active UC symptoms should consider skipping caffeinated and alcoholic drinks.
Stress Anxiety And Depression
As with many chronic health conditions, UC can take a toll on mental health. This stress can, in turn, worsen UC symptoms and lead to flares. Studies have found that stress triggers a series of reactions in the body that suppress the immune system, causing inflammation of the intestines. Additionally, stressful emotions, such as anxiety and depression, have been found to cause abdominal pain in people with IBD.
Flare-ups can be exacerbated in the setting of recent life stressors, such as the loss of a job, Dr. Kinnucan said. Anxiety and depression can contribute to an increase in clinical symptoms in people with IBD, and may worsen quality of life, she added. It is important to address symptoms of anxiety or depression with your health care provider.
Recommended Reading: Foods Bad For Ulcerative Colitis
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
To Avoid: Milk Products
Foods made with cow’s milk can cause problems for some people, which is why it’s often recommended that people with IBD avoid them. A gastroenterologist can help in diagnosing lactose intolerance, and for those who do have an intolerance and find milk products cause gas and pain or other symptoms, avoiding those foods is the best idea. This includes foods like a glass of milk, cheeses, ice cream, pudding, and yogurt. Some foods will have a lower lactose content, or may even contain only traces of lactose, such as yogurt and aged cheeses .
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Also Check: How To Fix A Stomach Ulcer
Are There Positive Effects Of Drinking Alcohol
To complicate matters further, while drinking alcohol clearly has some very negative effects on health, and on the GI tract, in particular, there are potential positive effects. In addition to the psychological and social benefits of the occasional drink at parties, moderate amounts of alcohol may have some health benefits. Studies have indicated that moderate drinking may have a positive effect on the coronary system and help prevent coronary artery disease.
To Drink: Liquid Nutrition
There are a variety of nutritional supplements on the market that can be found in grocery and drug stores. They do tend to be pricey, but they can add much-needed nutrients to the diet during a flare-up. A gastroenterologist can recommend a particular brand and offer advice on how often they should be used. Liquid nutritional supplements shouldn’t be used as the sole source of calories, however, as they are only meant to augment the diet until more foods can be added.
Don’t Miss: Classic Features Of Ulcerative Colitis
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
How To Eat During An Ibd Flare
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
People with inflammatory bowel disease often face an uphill battle when it comes to diet, especially when the disease is active. Many people with IBD dont know what food to eat when the Crohns disease or ulcerative colitis is flaring. Everyone with IBD is different, and one persons flare-up diet isnt going to work for another, but there are some broad ideas that may work for many.
-
Milk, cheese, ice cream, and yogurt
-
Brown rice, popcorn, oats, and barley
-
Fried food
Also Check: How Do I Get Rid Of A Stomach Ulcer
Don’t Miss: Stomach Ulcer And Chest Pain
How To Manage Ulcerative Colitis Flares
Although there isnt a cure for ulcerative colitis, there are plenty of treatment options to reduce inflammation and help you return to your daily routine. Depending on the severity of your flare-up and your individual needs, your healthcare provider can recommend treatment to help you manage ulcerative colitis flares.
The end goal of treatments for ulcerative colitis flare-ups is to maintain remission. You might always have ulcerative colitis, but if you care for yourself you can avoid intense flare-ups. Your healthcare provider might recommend a medication to reduce swelling, heal tissue, relieve symptoms, reduce pain, and avoid diarrhea:
You cant completely avoid flare-ups. If you eat well and take your medicine as prescribed, its likely that your disease will stay in remission. See your healthcare provider regularly to make sure that youre always doing whats best for your body, even when its been a while since you had a flare-up.
Ulcerative colitis flares can affect how you travel, your personal relationships, your professional life, and more. The most important thing you can do is to face your fears and worries instead of letting them control your life.