Diagnosing A Stage 4 Bedsore
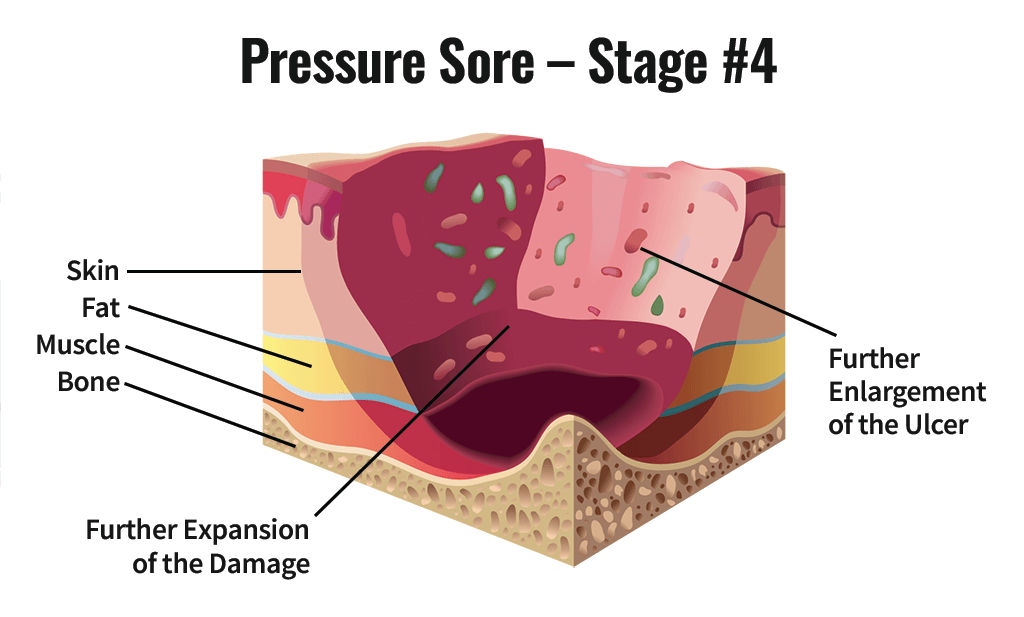
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
You May Like: How Do They Treat Ulcerative Colitis
Preparing To Go Home After Surgery
Your discharge recovery plan will be made before surgery. Your care plan will focus on doing everything possible to promote healing and prevent problems.
- You will need to be taught wound care, or your family will need to be taught if they are going to help manage your care. Normally, not much wound care is needed other than cleaning, keeping the area dry, and managing any wound drains.
- Home health care or a stay in a skilled nursing facility may be set up if needed.
- Follow-ups with your doctor as needed.
- You must have the proper equipment to promote healing and help prevent future skin problems.
- A pressure-reducing mattress . You will lie on this air or fluid bed to reduce pressure on the healing wound.
- A pressure-reducing seat cushion. Pressure mapping should be done for wheelchair users to ensure that the best cushion is used. Pressure mapping uses a thin, sensor mat on the wheelchair seat. A computer screen displays how well your weight is spread across the seat surface. Spreading weight out help reduce pressure points that are more likely to damage the skin.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
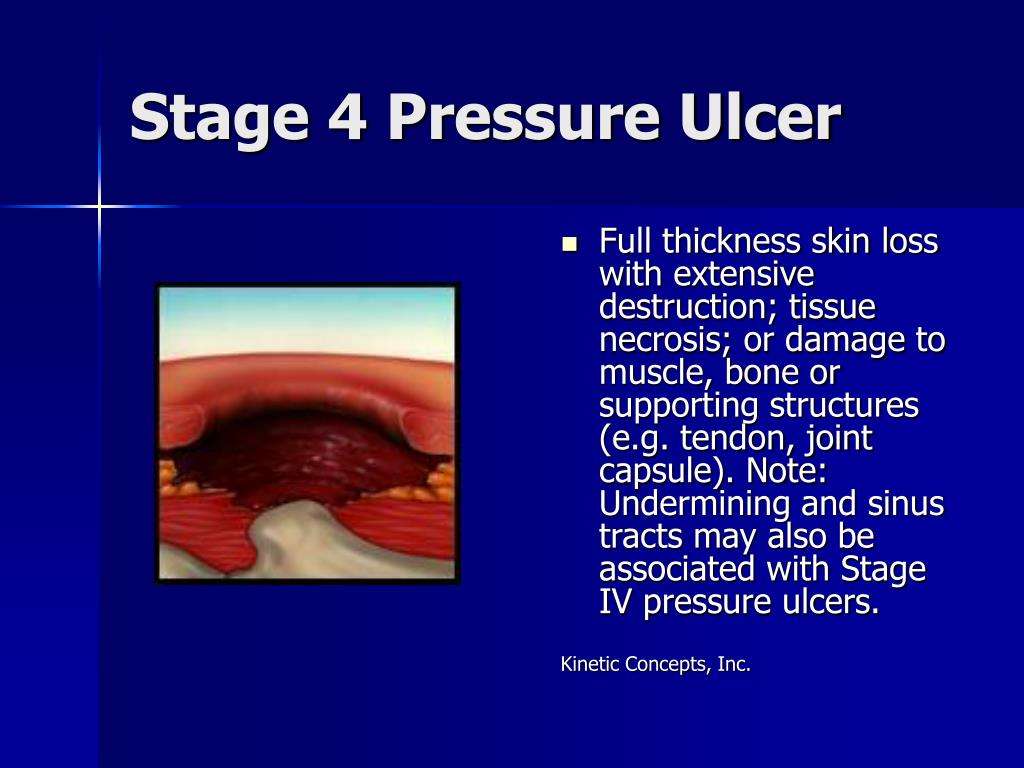
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Recommended Reading: Herbal Medicine For Ulcerative Colitis
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
- Consider specialty wheelchairs that can be tilted to relieve pressure
- Elevate bed to no more than 30 degrees at the head
- Have the resident perform wheelchair pushups if possible
- Keep skin clean and dry
- Purchase special mattresses or cushions to position the body properly
- Shift weight about once an hour
- Use moisturizing skin care to protect the skin
Also Check: How To Get Remission In Ulcerative Colitis
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
How Can Pressure Injuries Be Prevented
The development of pressure injuries can be prevented through careful observation of the skin and frequent repositioning in those who canât turn themselves. Tips to prevent pressure injuries include:
- Keeping the skin clean and clear of bodily fluids.
- Moving and repositioning the body frequently to avoid constant pressure on bony parts of the body.
- Using foam wedges and pillows to help relieve pressure on bony parts of the body when turned in bed.
- Maintaining a healthy diet to avoid malnutrition and to assist in wound healing.
Don’t Miss: Ulcerative Colitis And Hip Pain
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the ‘control’ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
These Are The Signs Of Stage Four Ulcer Development
In hospitals and healthcare institutions worldwide, the topic of pressure injuries comes up frequently when discussing patient care and risk management. This makes sense. Pressure injuries have the potential to cause significant problems for both patients and healthcare professionals. In the United States, 2.5 million people experience pressure injuries each year, and 60,000 of those die annually. These particular injuries, also known as hospital acquired pressure injuries , can develop in hospital beds or in operating rooms. In fact, up to 45% originate on operating tables. When left untreated, pressure sores can result in severe tissue damage and even death. These statistics offer a stark reminder that comprehensive treatment for pressure injuries is vital. And beyond thatprevention methods should be integrated at the beginning of patient care.
Over the last year, weve watched and learned as hospitals have undergone serious strain due to COVID-19. With staffing efforts redirected to address the virus, inefficiencies in routine patient care have become more obviousparticularly care that tends to be manual and labour-intensive, such as monitoring for pressure injuries. In a world grappling with this global pandemic, we have a responsibility to help alleviate pressure on our valued healthcare workers by integrating smart, sustainable technology that prevents injuries efficiently, with far less work required.
What are the stages of a pressure sore?
Don’t Miss: Tofacitinib Acute Severe Ulcerative Colitis
What Is A Stage 4 Bedsore
Stage 4 bedsores are the most severe form of , also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
A stage 4 bedsore may be an unfortunate sign of . Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
Thankfully, financial compensation may be available if your loved one develops a stage 4 bedsore while living in a nursing home. Get a free case review to see if you can pursue compensation to help pay for medical treatment.
Victims of stage 4 bedsores can take legal action.
to learn if you can access financial aid and hold abusive nursing homes accountable.
Stage 4 Bedsore Causes
Stage 4 bedsores typically form if earlier-stage pressure injuries are not properly treated.
All when factors like pressure, shear, and friction cut off blood supply to the skin. Without proper treatment, the loss of blood can cause the skin to die and a wound to form.
Did You Know
A stage 4 bedsore is the worst-case scenario: the blood loss is so severe that the wound tunnels down through all layers of the skin and exposes bone.
Nursing home bedsores are often the result of improper care from staff.
Residents may develop bedsores if staff members:
- Cannot adequately care for every resident due to understaffing
- Dont treat dehydration or malnutrition, which can prevent healing or worsen sores
- Fail to notice or treat earlier stage sores due to skipped or rushed care
- Leave residents with mobility issues lying in beds or wheelchairs for hours on end
Read Also: What Happens When You Have A Bleeding Ulcer
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
-
Ovid MEDILINE
-
Ovid MEDLINE
-
Ovid Embase
-
EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
-
ClinicalTrials.gov
-
WHO International Clinical Trials Registry Platform
-
EU Clinical Trials Register .
Searching other resources
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
Don’t Miss: Stomach Ulcer Treatment In Homeopathy
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Stages Of Pressure Ulcer
Pressure ulcer wound is a concentrated area where the soft tissues of the body is damaged due to the compression of a bony surface and an external surface for a prolonged period of time.
Source: HealthSaver
Stage 1 | Redness
There is a concentrated area of redness on a pigmented/discoloured skin. The skin might appear as blue or black.
Stage 2 | Partial Thickness Skin Loss
There is partial skin loss on the surface of the wound usually involves the epidermis layer . The ulcer is considered as superficial and looks like a abrasion, crater or blister type of wound.
Stage 3 | Full Thickness Skin Loss
Full thickness skin loss usually consists of damage to the subcutaneous tissues . The subcutaneous tissues act as a protective layer for our muscles and bones.
Stage 4 | Cavity
At this stage, patient will suffer from full thickness skin loss with tissue necrosis to the underlying bone, tendons and joint capsules.
Also Check: Holistic Cure For Ulcerative Colitis