Symptoms Of Ulcerative Colitis
The symptoms of Ulcerative Colitis vary from minor to debilitating and can significantly affect your quality of life. The diagnoses is made once a patient presents with a flare. Flares can last weeks to months. The acute symptoms include multiple bowel moements per day with or without blood and mucus. Chronic abdominal pain with cramping and nausea, extreme fatigue and anemia are also common. Patients with irritable bowel disease are extremely malnourished due to the inability to absorb nutrients from their food. For this reason, they get sick often, lose hair, and have overall weakness.
Inhibition Of Immune Cell Trafficking
Inhibition of immune cell trafficking has emerged as a major therapeutic principle in IBD. Immune cells circulate within the blood stream and lymphoid organs, and specific mechanisms ensure homing of leukocytes into specific organs. Integrin-47 is specifically expressed on lymphocytes activated in gut lymphatic structures. This integrin interacts with mucosal addressin cell adhesion molecule-1 , expressed on blood vessels of the intestinal tract and intestinal lymphatic structures . Therapeutic interference with gut homing offers the promise of a gut-specific mode of action with potentially low systemic immunosuppression.
Natalizumab, a monoclonal antibody targeting the integrin-4 subunit, is an effective treatment of IBD . However, since the integrin-4 subunit is also critical for 41-dependent central nervous system homing of lymphocytes, natalizumab treatment can be complicated by progressive multifocal leukoencephalopathy due to JC virus reactivation . Therefore, natalizumab is only rarely, if ever, used for IBD treatment and only in patients with JC-negative serology or with a very strict surveillance framework .
Expert Opinion
Current Treatment At Other Clinics
Current treatment involves using medications and at times injection. These treatments are considered a patch up of the problem without treating the root cause of the problem. Medications & steroids have many side effects including weight gain & increased blood sugar from steroids, damage to kidneys, heart, stroke & gastric ulcer. Surgery can be very debilitating with prolong downtime during recovery requiring at times prolonged bed rest & even residing in nursing home for recovery. It also entails a lot of risk including risk of infection, bleeding, poor surgical outcome to name a few. Stem cells however, reduce the inflammation and pain that are typical of these conditions.Current ongoing research on the effect of stem cells has shown positive results.
We are different from many other clinics who offer stem cell or PRP. Other may also not offer option of bone marrow derived stem cell, Adipose derived stem cell & umbilical cord stem cell. They in effect expose patients to more invasive treatments like drilling bones without offering other easier options. They also may use xray with unnecessary radiation for injections that can be easily avoided in most cases by using ultrasound. Furthermore, they may not have proper knowledge of how other modalities can enhance the effects of Stem Cells. These other modalities are used by us to focus on the whole joint and treating different parts of it instead of just treating one out of several diseased structures in the joint.
You May Like: Interprofessional Care For Ulcerative Colitis
Cost Of Treating Uc & Ibd With Msc+ Stem Cells
The treatment for ulcerative colitis or Crohns will require 12-16 nights in Bangkok. Due to the varying degrees of the disease progression, our medical team will need to better understand a potential patients needs before a treatment prognosis can be provided. Upon approval, a detailed treatment plan shall be provided that will include all specifics relating to the patients needs such as the exact total number nights required in Thailand along with the total medical related costs for the entire treatment. To begin your an inquiry, please prepare your recent medical records and diagnostic test results and contact us today.
Rehab After Treatment: Physical rehabilitation for treatment is optional depending on the patients travel/time constraints. Complete physical rehab programs can be provided for patients at a partner hospital from two to four hours per day and 7 days per week. Medical visas for longer travel and extended stay apartments or hotel accommodations for the patient and family can also be requested.
Treatments For Crohns Disease
Traditional treatment for IBD typically requires a wide variety of pharmaceutical medications ranging from:
- Corticosteroids & Prednisone
- Immunosuppressive medications
Patients with a chronic condition or a serious diagnosis may require surgery to remove the large intestine resulting in a life long need for a colostomy bag which is an eternal or internal plastic pouch for fecal and waste removal. A large number of Crohns disease patients often require strictureplasty surgery and or corrective surgery to repair fistulae, strictures to stop the bleeding in the intestines. A strict change in diet is also usually needed to promote proper cell signaling, help reduce stress and inflammation. Patients are usually recommended to avoid eating greasy foods, processed meat products, spicy foods, cream sauces, or foods with high fiber.
Read Also: What Foods To Eat With A Peptic Ulcer
Is Ulcerative Colitis A Genetic Disease
It is known to be more common in some families. First-degree relatives are also affected by the disease in about 20% of patients. However, there is no absolute genetic transition that has been identified to date but it would be fair to say that there is predisposition. For example, the risk in children with inflammatory bowel disease in both of their parents may increase up to 36%.
Ulcerative Colitis & Ibd Autoimmune Diseases
The definitive causes and triggers of IBD is still in debate but functional medical specialists believe that the IBD and SLE family has a certain genetic predisposition and can be directly linked
with over 165 specific genes in our bodies. Most doctors believe the culprit is a combination of environmental and hereditary conditions that are triggered by environmental factors that result in a sudden bacterial shift are examples of autoimmune diseases that can develop after an abnormal immune response. External factors like stress and dietary habits can significantly worsen the symptoms of IBD however they typically do not cause the disease.
There are several tests available today that can quickly diagnose UC ulcerative colitis and Crohns disease. The most common method uses a simple Blood test to trace symptoms of inflammation or anemia. Stool samples can also be used for finding signs on an infected digestive tract. Diagnosis can be confirmed using genetic testing along with sigmoidoscopy or colonoscopy test that uses long thin tubes that have lighted cameras to enter a patients intestine for visual inspection and/or to take tissue samples i.e. biopsy. Other minimally invasive tests to verify intestinal issues include MRI Scans, CT scans, Ultrasound Scan or capsule endoscopies.
TREATMENT PRECAUTIONS & RISKS
You May Like: Ulcerative Colitis And Colon Cancer Statistics
Generation And Characterisation Of Adipose
C57BL/6J, BALB/cJ and human aMSCs were generated from abdominal adipose tissue as described in Supplementary Material, available as Supplementary data at ECCO-JCC online. Human adipose tissue samples were obtained after informed consent approved by the Spanish Ethics Committee . aMSCs were defined according to the criteria of the International Society for Cellular Therapy .
Stem Cell Therapy For Crohn’s Complications
The evidence is stronger about the benefits of stem cell therapy for Crohn’s disease complications.
About 20% of people with Crohn’s disease get an abnormal tunnel between their intestines and their , called a perianal fistula. This can be very painful. It causes some people to lose control of their bowel movements.
Very few treatments help with perianal fistulas. Up to 90% of people who have this complication need surgery to fix it.
Stem cell therapy could offer a less invasive way to treat perianal fistulas. A few studies have shown that stem cells taken from fat tissue help close and heal fistulas.
Darvadstrocel is a stem cell treatment that has been fast-tracked by the FDA. Alofisel treats adults with complex perianal fistulas that haven’t improved with other treatments. The FDA considers Alofisel a regenerative medicine advanced therapy . This means it may help, but it may not be available at every medical center or covered by insurance.
You get this treatment as an outpatient procedure, which means you go home on the same day. The doctor injects stem cells taken from the fat tissue of a donor into the fistula.
Researchers are also studying stem cell injections as a treatment for strictures â narrowed areas of the intestines that affect some people with Crohn’s disease. So far, trials have only tested this treatment on a few people.
You May Like: How To Relieve Mouth Ulcer Pain
What Is Unique About Receiving Stem Cell Therapy Through Trustem Cell Therapy For Ibd
-
Our focus is safety, efficacy, and patient-centric care when providing access to superior stem cell therapy.
-
We utilize only board certified surgeons, physicians and accredited clinicians to provide care for patients.
-
Laboratory protocols are developed and refined by our PhD Neuroscientist.
-
A clinical team with expertise in practicing cellular based medicine.
-
Accredited Surgical Centers for enhanced procedural and patient safety
-
Targeted administration methods that direct stem cells toward specific
-
Skilled Patient Advocates who are trained to provide truthful, realistic expectations resulting from stem cell therapy. We do not make outlandish promises of cures or inaccurate claims related to improvement rates.
Lymphocyte Trapping By Sphingosine
A new class of sphingosine-1-phosphate receptor modulators enables functional inactivation of lymphocytes by trapping them within lymphoid organs . Sphingolipids are normal constituents of a cell membrane which can be phosphorylated to S1P by sphingosine kinases 1 and 2 . Degradation of S1P by S1P lyase results in a gradient of S1P with higher S1P concentrations in blood but lower concentrations in secondary lymphoid organs. Lymphocyte trafficking along this gradient results in the release of B cells, dendritic cells, and some T-cell subsets into the circulation .
Fig. 3.
Lymphocyte trapping by S1PR modulation. Lymphocytes enter a lymph node via afferent lymphatics and leave the lymph node via an efferent lymphatic vessel. For the egress from a lymph node, lymphocytes follow a S1P gradient. Blocking of S1P receptors by filgotinib, ozanimod, or etrasimod inhibits release of lymphocytes into the circulation and results in lymphocyte trapping within the lymph node. Figure adapted from . S1PR, sphingosine-1-phosphate receptor.
Expert Opinion
S1P receptor modulation is an attractive new therapeutic principle. Newer S1P receptor modulators might be safer than fingolimod, and if no unforeseen safety issues arise, these drugs would be promising and powerful new agents for the treatment of UC.
Also Check: Best Prebiotic For Ulcerative Colitis
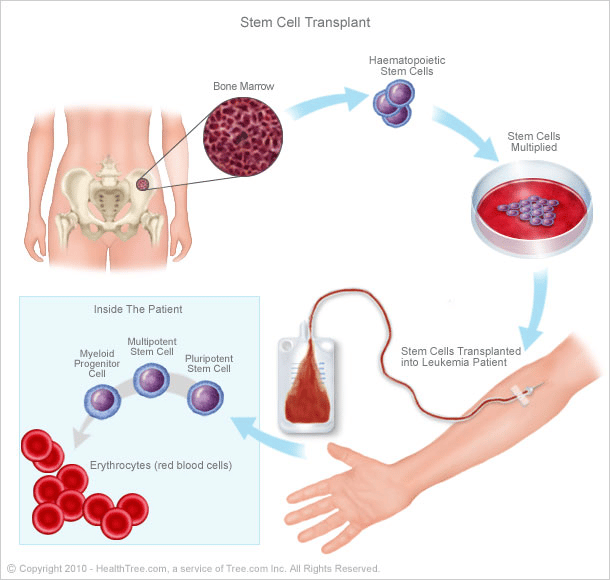
Bone Marrow Or Peripheral Stem Cell Transplantation
In most quarters transplantation of stem cells mobilised to and recovered from the circulation has replaced the use of those directly harvested from the bone marrow. This is because it is easier and cheaper, no general anaesthetic is needed, and engraftment occurs more rapidly. Peripheral stem cell transplantation requires mobilisation by single agent chemotherapy and/or use of a haemopoetic growth factor such as granulocyte colony stimulating factor . Use of growth factors in autoimmune disease has been associated with a temporary flare of the disease. If the same occurs with inflammatory bowel disease, use of growth factors for stem cell mobilisation in inflammatory bowel disease might be sufficiently deleterious to the underlying problem to be contraindicated. If so, use of directly obtained bone marrow would be an alternative.
Why Utilize Mesenchymal Stem Cells To Treat Crohn’s
Stem cells are the body’s raw materials â cells from which all other cells with specialized functions are created. Mesenchymal stem cells are adult stem cells that have self-renewal, immunomodulatory, anti-inflammatory, signaling, and differentiation properties. Mesenchymal stem cells , self renewal capacity is characterized by their ability to divide and develop into multiple specialized cell types present in a specific tissue or organ.
MSCs are widely used in the treatment of various diseases due to their self-renewable, differentiation, anti-inflammatory, and immunomodulatory properties. In-vitro and in-vivo studies have supported the understanding mechanisms, safety, and efficacy of MSC therapy in clinical applications.
According to a 2018 study conducted by Crigna, et al.
“MSCs mainly exert their regenerative effects through paracrine and endocrine modes of action, which include immunomodulatory, anti-inflammatory, mitogenic, anti-apoptotic, anti-oxidative stress, anti-fibrotic, and angiogenic influences.”
Read Also: How To Soothe Mouth Ulcers
Stem Cell Therapy For Crohn’s Disease
Inflammation is prevalent in disorders ranging from heart disease and diabetes to IBD and Crohn’s Disease. Treatment of these diseases, as well as many other common conditions, usually addresses the reduction of inflammation in the body. Whether through drugs, diet and lifestyle changes, or other natural methods, the goal is to eliminate as much inflammation from the body as possible.
Researchers have shown over the years that Mesenchymal Stem Cells are one of the strongest anti-inflammatory tools available today and many patients are turning to stem cell therapy to meet their needs.
T-cell activation within the gastrointestinal tract leads the body to conduct an immune response leading to chronic inflammation causing pain and discomfort. Mesenchymal Stem Cells have the inherent ability to target inflammation within the body and repair damaged tissue. This potentially makes a large stem cell transplant an effective treatment for inflammatory conditions such as Crohn’s Disease.
Stem cell therapy may help Crohn’s Patients through these processes:
- Reduction in inflammation throughout the digestive tract
- Regulating the immune system
- Repairing injured tissue within the gastrointestinal tract
Stem cell research has shown that cell therapy may have the ability to promote the repair of diseased, dysfunctional or injured tissue. There have been many positive and exciting outcomes for patients who have had little success with conventional treatments.
How Is Ulcerative Colitis Diagnosed
The most important diagnostic method is evaluation and examination of the patient by the doctor. In addition to the foregoing, some tests are required for a definitive diagnosis.
- In particular, a fecal test for certain bacteria and amoeba should be performed. Because some bacteria such as shigella and some parasites such as Entamoeba histolityca may show a presentation similar to that of ulcerative colitis.
- Anemia, elevated levels of white blood cells height and elevated sedimentation can be seen. Anemia is caused by bleeding. Elevated levels of white blood cells and sedimentation reflect the severity of inflammation.
- The study of the large intestine using a medicinal agent can be used to get an insight about the type and spread of the disease. Blood count and amoeba examination in feces can be performed to make differential diagnosis of other diseases with similar symptoms.
Read Also: Symptoms Of Crohn’s Disease And Ulcerative Colitis
Immunosuppressive Mediators Of P
Immunosuppression-mediating molecules were measured in P-ADSCs or H-ADSCs after priming IFN- and TNF- separately or combined. With no treatment, there was a certain amount of IL-6 secretion by both P-ADSCs and H-ADSCs , as well as secretion of TSG-6 , PGE2 , and IDO activity . Upon treatment with IFN- or/and TNF-, the secretion of IL-6, TSG-6, and PGE2, and IDO activity of P-ADSCs and H-ADSCs were increased. P-ADSCs primed with IFN- alone or with the combination of IFN- and TNF- exhibited significantly lower TSG-6 secretion compared with H-ADSCs . P-ADSCs primed with TNF- alone or with the IFN-/TNF- combination exhibited lower PGE2 secretion compared with H-ADSCs . Moreover, P-ADSCs incubated with IFN-, TNF-, or both exhibited lower IDO activity , but IL-6 secretion was not significantly different between P-ADSCs and H-ADSCs .
FIGURE 5. Immunosuppressive mediators involved in the immunosuppressive effect of P-ADSCs and H-ADSCs. P-ADSCs or H-ADSCs were primed with IFN- and TNF- separately or combined for 48 h. Levels of the immunosuppressive factors IL-6 , TSG-6 , and PGE2 determined by ELISA. IDO activity expressed as the concentration of kynurenine .
Exosomes From Olfactory Ecto
Olfactory ecto-MSCs are a novel population of resident stem cells in the olfactory lamina propria with considerable immunosuppressive activity. In colitis mice, the intravenous administration of exosomes derived from OE-MSCs markedly increased the colon length, reduced the DAI score and inflammation, and retained the integral structure of the colon, and with less lymphocytic infiltration, decreased the crypt loss and lowered the histopathological scores . The ameliorative effect of OE-MSC-Exo on the disease severity was accompanied by diminished Th1/Th17 cell pro-inflammatory responses and enhanced Treg cell anti-inflammatory responses . Mechanistically, OE-MSC-Exo administration was found to exert immunomodulatory effects by suppressing differentiation of Th1/Th17 cells and inducing the differentiation of Treg cells as well as inhibiting T cell proliferation via reducing IL-17 and IFN- and enhancing TGF- and IL-10 production by the T cells .
Also Check: Ulcerative Colitis And Blood Clots
How Well Does Stem Cell Therapy Work
That’s hard to say. Most stem cell treatments for Crohn’s disease are still experimental. This therapy hasn’t been studied in enough people to prove that it works, but thereâs reason to be hopeful.
In studies done so far, stem cell therapy eased inflammation, helped the intestines heal, and improved quality of life in people with Crohn’s disease.
One review looked at 18 studies that included 360 people with Crohn’s disease. People who received stem cell therapy had less active disease than those who didn’t get this treatment. Over 70% of people who got stem cell therapy were in remission â meaning they had no signs of the disease â 3 months later. More than half were still in remission 1 to 2 years after their treatment. Some people said their quality of life improved after the stem cell treatment.
In the studies, HSCs worked better against Crohn’s disease than MSCs. Stem cells that were taken from a person’s own body helped more than cells from a donor.
Mesenchymal Stroma Cell Therapy
Treatment with MSCs might be a paradigm shift in the treatment of fistulizing CD. MSCs are adherent cells with a fibroblast-like phenotype with reservoir function as stem cells for adipocytes, osteoblasts and chondrocytes . MSCs constitute up to 1% of the cellular content of the adipose tissue but can also be found in the bone marrow and other tissues. Upon stimulation by pro-inflammatory cytokines, MSCs secrete a variety of immunosuppressive molecules, thus decreasing overall inflammation . In addition, MSCs can promote wound healing and tissue regeneration by secretion of TGF- and fibroblast growth factor, and MSCs are also able to differentiate into fibroblasts or endothelial cells for formation of granulation tissue . Thus, MSCs combine anti-inflammatory and regenerative properties, and both of these properties would be of value for the treatment of fistulizing CD. MSCs do not express MHC II, and only low amounts of MHC I, and do not stimulate T cells, thus enabling escape from immune surveillance and low rejection after transplantation .
Expert Opinion
Mesenchymal stem cell therapy is an innovative therapy for CD fistula with surprisingly high success rates in this very hard-to-treat patient population. While MSC therapy is currently established in large centers, costs, logistical challenges, and lack of long-term data so far limit wide-spread application.
Don’t Miss: Primary Sclerosing Cholangitis Ulcerative Colitis