When To Contact A Doctor
People without a diagnosis should seek guidance from a doctor if they experience UC symptoms for more than a few days. Symptoms of UC may indicate other conditions, so a doctor will need to rule out all potential causes.
Individuals with a UC diagnosis should contact a doctor to determine the appropriate treatment and to create a plan of action for when a painful flare occurs.
A person should also contact a healthcare professional whenever their pain worsens or a new type of pain appears.
How To Treat Ulcerative Colitis Pain
While there isnt a cure for ulcerative colitis yet, there are ways to treat the inflammation and discomfort. In most UC cases the pain is at its worst during a flare-up, and some peeps are completely pain-free outside of these times. Pain treatment involves a mix of reducing the risk of painful flare-ups and the discomfort experienced during them.
Some treatments are medical interventions, while others are lifestyle and self-management techniques. Here are some effective options:
How To Define Ulcerative Colitis Pain
To help your doctor figure out whats causing your abdominal pain and other symptoms, you need to be able to accurately describe the sensation. Before seeing your doctor, take stock of what youre feeling. It may be useful to keep a colitis symptom journal to write down what you are experiencing. Be ready to describe:
- How long youve had your pain
- Where you feel your pain
- How it feels, both in sensation and intensity
- The frequency and duration of your pain
- What seems to trigger your abdominal pain
- What seems to help ease the pain
- What time each pain occurred, including how long after eating, and how long it lasted
The more specific you can be about your pain, the better, Dr. Kane says.
Read Also: Does Ulcer Pain Come And Go
You May Like: Foods To Eat To Heal An Ulcer
What Do Abdominal Spasms In Ulcerative Colitis Feel Like
People with ulcerative colitis have many different experiences with abdominal or intestinal spasms. Sometimes, these spasms can be uncomfortable, but not painful. As one MyCrohnsAndColitisTeam member wrote, Ive been having spasms in my colon since yesterday. I am so glad they arent painful, but its super annoying. Another agreed, saying, I dont think my abdominal spasms really hurt at all.
Some people with UC have painful spasms. One member described their daily spasms like this: Normally, by 8 p.m., the spasms start in my colon. By 10 p.m., I usually go to the bathroom in tremendous pain and with more spasms. Another member who also experiences painful spasms wrote, I have been having rectal spasms that last and cause me so much pain! My whole pelvic floor is sore.
Ultimately, the abdominal spasms associated with ulcerative colitis can range from annoying and frustrating to painful and debilitating. No matter what they feel like, talking to your doctor may help you find ways to manage this symptom and improve your quality of life.
Can Lifestyle Changes Help Relieve Ulcerative Proctitis Symptoms
Remember, ulcerative proctitis is an autoimmune disease, meaning you didnt do anything to cause it. Even in remission, theres a risk of disturbing the very fine balance within the colon that can tip a flare-up, Dr. Lerrigo says. Its not the patients fault.
However, he says there are a few things you can do to try and support a healthier GI tract.
The perfect diet doesnt exist because each person has unique nutrition needs, explains Dr. Lerrigo. Thats why most of his patients work with a registered dietitian. However, experts do know that a diet that closely mimics the Mediterranean diet, one that is focused on fiber-rich whole grains, leafy vegetables, nuts, legumes, lean proteins like chicken and fish, and some dairy if you tolerate it, promotes a healthy gut ecosystem2 and reduces the risk of ulcerative proctitis flares, Dr. Lerrigo says.
He also recommends getting plenty of exercise and doing your best to manage stress, both of which can impact the immune system.
Read Also: Anbesol Gel For Mouth Ulcers
Avoid Your Personal Trigger Foods
If your cramps tend to flare up after a meal, your body is probably struggling to digest something you ate. Trigger foods can worsen inflammation and gas, which increases the pain, Dr. Naik says. Keeping a food log can help you spot any culprits, which may include dairy, carbonated drinks, and high-fiber foods, according to the Crohns & Colitis Foundation. Try eating soft, bland foods like bananas and toast while you figure out your personal triggers.
Herbal And Alternative Treatments
Cannabis research increasingly points to benefits for a range of chronic health conditions, but there is minimal evidence specific to ulcerative colitis at this time. Studies so far suggest the potential of cannabis to improve the quality of life for people with UC, likely due to its anti-inflammatory and antioxidant effects. More investigation is needed before recommendations can be made.
Other studies show that, compared to placebo, the treatments of aloe vera gel, wheatgrass juice, andrographis paniculata extract, and topical Xilei-san may all help alleviate UC symptoms. Before experimenting with any alternative treatments, you should always consult with your health care provider.
Also Check: Foam Dressing For Diabetic Foot Ulcer
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Ulcerative Colitis Treatment In Children
Ulcerative colitis tends to be more severe and aggressive in childrenand the inflammation tends to affect more of the colon, according to Yale Medicine1. But the good news is that it can be treated so that kids with UC can live largely normal lives.
Overall, management of ulcerative colitis in children is similar to management in adults, according to Dr. Pasha. For example, kids have similar medication options available to them, such as 5-ASAs, steroids, biologics, and immunomodulators. However, nutrition and growth issues are usually closely monitored. A childs doctor will keep a close eye on any signs of loss of appetite and weight loss, since those can impede a childs growth.
In severe cases, surgery, such as the surgical removal of the colon, may also be an option if the children dont respond well enough to medications, or they experience a ruptured colon or severe bleeding. But ulcerative colitis surgery in kids is much less common these days, thanks to advances in medications like biologics that help control symptoms and let the children enjoy longer periods of remission.
Recommended Reading: Best Toothpaste For Mouth Ulcers
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Pain As A Tool For Diagnosis
Because pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint, it is not a symptom that is normally used to diagnose IBD or a particular form of IBD.
Rather, the type and location of pain is more often used together with other signs and symptoms when diagnosing IBD or other conditions. In other words, it might be a starting point to help a healthcare provider know where to start looking for inflammation, but its only one part of the picture.
Recommended Reading: Can You Eat Oatmeal With Ulcerative Colitis
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
People Describe How They Were Diagnosed With Ulcerative Colitis

Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohns disease .
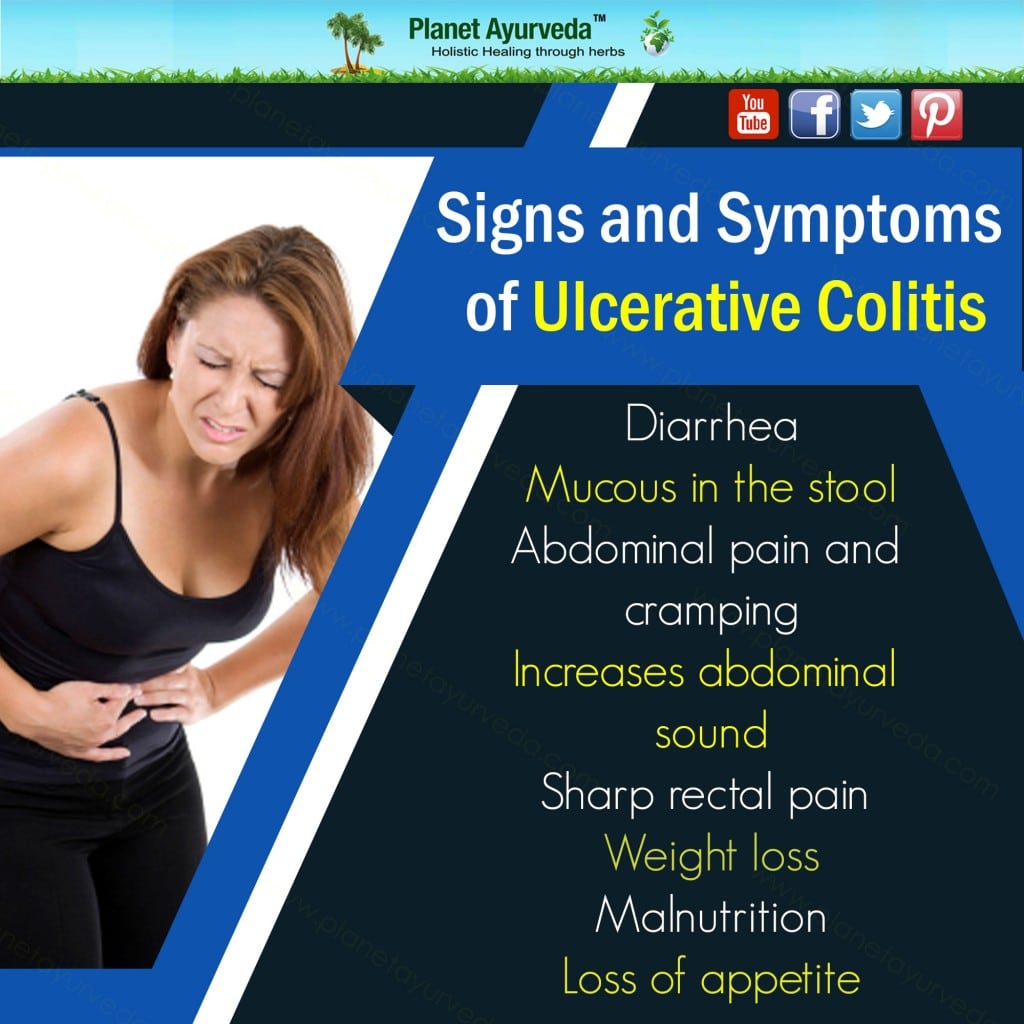
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while theres no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesnt cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related:
Don’t Miss: Ulcer In Colon Found In Colonoscopy
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Keep Up With Regular Physicals
Getting an annual physical is always smart, but its especially important if you have UC.
During the checkup, your healthcare provider will ask whether your treatments are going well and ensure that screening is performed at the appropriate intervals to catch any cancer in the early stages. Even if your UC symptoms are in remission , seeing a healthcare provider regularly can help ensure that you stay on the healthy track.
You May Like: Is Constipation A Symptom Of Ulcerative Colitis
Recommended Reading: Best Nsaid For Stomach Ulcers
Set A Daily Or Weekly Goal
Goal-setting is a great way to distract yourself from the discomfort caused by UC. Youre engaging the brain, says Dr. Szigethy, and in the process also shifting any pain you might feel to the back of your mind. The doctor recommends any goal that involves physical activity: a daily walk or a 15-minute yoga flow are two great options. Youll feel good that youre doing something to improve your health, she says. Plus, exercise is a proven stress-reducer, which can help alleviate symptoms of UC, too. Make sure you regularly update your goals, she suggests, noting how the brain responds well to novelty.
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
Read Also: Ulcerative Colitis Abdominal Pain Relief
Don’t Miss: Can Alcohol Cause Stomach Ulcers
Give Yourself Some Tlc
Stress doesn’t cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
10
Surgery For Ulcerative Colitis
Surgery for ulcerative colitis usually involves removing the entire colon and the rectum. Removal of the colon and rectum is the only permanent cure for ulcerative colitis. This procedure also eliminates the risk of developing colon cancer. Surgery in ulcerative colitis is reserved for the following patients:
Standard surgery involves the removal of the entire colon, including the rectum. A small opening is made in the abdominal wall and the end of the small intestine is attached to the skin of the abdomen to form an ileostomy. Stool collects in a bag that is attached over the ileostomy. Recent improvements in the construction of ileostomies have allowed for continent ileostomies. A continent ileostomy is a pouch created from the intestine. The pouch serves as a reservoir similar to a rectum, and is emptied on a regular basis with a small tube. Patients with continent ileostomies do not need to wear collecting bags.
Recommended Reading: Indian Diet For Ulcerative Colitis
Don’t Miss: How To Treat Stress Ulcers
Diet And Lifestyle Changes To Try
Managing ulcerative colitis isnt just about taking medication. You can embrace certain lifestyle changes that can help improve your overall health. For example, you should make sure youre staying hydrated by drinking plenty of fluids, but you might want to reduce your intake of items like alcoholic and carbonated beverages or even skip them altogether, Dr. Pasha says.
As for your food, you might benefit from taking inspiration from a Mediterranean-style diet when youre not experiencing an acute flare, says Dr. Pasha. This kind of diet typically includes lots of fruits and vegetables, as well as olive oil as a primary fat source, whole grains, beans, nuts and seeds, and some amounts of low-fat dairy and lean sources of protein like fish and poultry, per the American Heart Association. Many of these foods are thought to have anti-inflammatory properties, although its not clear how much that might really help combat ulcerative colitis symptoms. Also, its important to be cautious about high-fiber foods, including some like whole grains that are integral to the Mediterranean diet, if youre experiencing any flare-ups, as that might exacerbate the problem.
The Mayo Clinic also recommends limiting your dairy intake, since many people with inflammatory bowel disease like UC have some trouble processing lactose in foods and experience diarrhea and pain as a result, according to the Mayo Clinic.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
You May Like: Most Common Extraintestinal Manifestation Of Ulcerative Colitis
Meal Timing And Portion Sizes
For most people with IBD,eating small meals is easier on the digestive tract. For others, the simple act of eating can rev up the digestive system and make diarrhea worse. If your bowel movements subside when you take a break between meals, consider reworking your meal timing to include more substantial meals less often.
Since UC symptoms vary from person to person, theres no one-size-fits-all meal schedule. Pain can feel worse when you’re not well-rested. Choose meals that are easy to tolerate when its close to bedtime, or finish eating for the day a few hours before going to sleep.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You May Like: How To Get Rid Of Stomach Ulcer Pain