Diagnosing Stage 3 Bedsores
Doctors diagnose stage 3 bedsores based on the symptoms and how deep the wound is.
Your doctor will likely look closely at your skin to decide if you have a pressure ulcer and, if so, to assign a stage to the wound. Staging helps determine what treatment is best for you.
Mayo Clinic
Factors that doctors look at to diagnose bedsores include:
PainPatients with stage 3 bedsores may not be able to sense pain due to severe skin and tissue damage. In stage 1 and stage 2, pain is very common.
Depth of the WoundA stage 3 bedsores is a deep tissue injury. It is a tunneling wound that penetrates the top layers of skin and underlying tissue but not the bone or muscle.
Seek immediate medical attention if your loved one has or may have a stage 3 bedsore. Bedsores pose a severe health risk and need to be treated promptly.
If nursing home staff members fail to help a resident get prompt medical attention for their stage 3 bedsore, they could be to blame if the sore worsens or causes dangerous complications.
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Here Are The Signs Of Stage Three Ulcer Development
In the healthcare industry, conversations surrounding risk management and patient care will inevitably lead to the topic of pressure injuries. And rightly so, as they are concerning to health care practitioners right across the globe. In the United States alone, 2.5 million people develop pressure injuries each year. Of that number, a startling 60,000 patients die as a result of pressure injuries. Those bedsores, also known as hospital acquired pressure ulcers , develop in operating rooms and hospital beds. In fact, up to 45% of HAPUs originate in the operating roomreminding us that pressure injury management must remain a top priority when designing patient care plans. If left untreated, pressure sores and pressure ulcers can cause severe tissue damage and even death proper treatment is key.
In the past year, weve seen continual reminders that the prevention of pressure sores must go beyond simple management efforts, instead reaching to more intelligent prevention tactics. The COVID-19 pandemic continues raging worldwide, putting significant strain on hospitals. To alleviate pressure on healthcare workers, we have an opportunity to work smarter in the prevention and mitigation of pressure injuries by integrating technology that helps staff optimize labor-intensive and time consuming pressure sore prevention methods.
Also Check: How Can You Tell You Have An Ulcer
Evidence And Scientific Basis For Guidelines
The panel identified six categories of pressure ulcer treatment: positioning and support surfaces, nutrition, infection, wound bed preparation, dressings, and surgery and adjuvant therapies. Specific guidelines and the underlying principle were developed in each category. Evidence references for each standard are listed and coded. The code abbreviations for the evidence citations were as follows:
| STAT |
-
Lyder CH. Pressure ulcer prevention and management. JAMA 2003 289: 2236.
- 2
Barrois B, Allaert FA, Colin D. A survey of pressure sore prevalence in hospitals in the greater Paris region. J Wound Care 1995 4: 2346.
- 3
Allman RM, Paprade CA, Noel LB, et al. Pressure sores among hospitalized patients. Ann Intern Med 1986 105: 33742.
- 4
Walter JS, Sacks J, Othman R, et al. A database of self-reported secondary medical problems among VA spinal cord injury patients: its role in clinical care and management. J Rehab Res Dev 2002 39: 5361.
- 5
Shiffman RN, Dixon J, Brandt C, Essahihi A, Hsiao A, Michel G, O’Connell R. The GuideLine implementability appraisal : Development and validation of an instrument to identify obstacles to guideline implementation. BMC Med Inform Dec Making 2005 5: 123.
How To Treat Pressure Ulcer
When Pressure ulcers are in the early stages, people may be able to treat them at home. Frequently changing positions can help the ulcers heal and keep new ones from forming.
Pressure ulcers can be prevented by periodically repositioning yourself to avoid stress on the skin. Other strategies include taking good care of the skin, maintaining good nutrition and fluid intake, quitting smoking, managing stress, and exercising daily.
MaxioCel, an advanced wound dressing product, provides faster healing to patients suffering from chronic wounds, such as pressure ulcers, diabetic foot ulcers, venous leg ulcers, cavity wounds, and skin abrasions to name some.
MaxioCel range of advanced chitosan dressings has the potential to address this gap and be a real game-changer. With a range of MaxioCel products, millions of patients who need advanced wound care products are being treated every year. MaxioCel with its 360-degree care combined hemostatic, pain management, and scar improvement properties, fulfills a large gap in the market.
Juwariah Khan
Don’t Miss: Can Ulcerative Colitis Lead To Crohn Disease
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Causes Of Stage 3 Bedsores
form when blood flow to the skin is cut off, causing healthy tissue to die and an abrasion to appear. The longer the bedsore is left untreated, the deeper the wound may become.
Stage 3 bedsores occur when fail to heal and the sore deepens into the patients skin.
Nursing home residents are at risk of bedsores if they sit or lie in the same position for long spans of time, which restricts blood flow and causes skin cells to die. While all nursing home residents with limited mobility may be vulnerable to advanced-stage bedsores, some residents have an especially high risk.
Residents are at higher risk of a stage 3 bedsore if they have:
- A cast on
- Health issues stemming from malnutrition
- Spinal cord injuries that limit movement
However, stage 3 bedsores can usually be prevented even in high-risk patients. Its the duty of nursing home staff members to identify these risk factors in patients and treat them.
Don’t Miss: What Are Some Symptoms Of An Ulcer
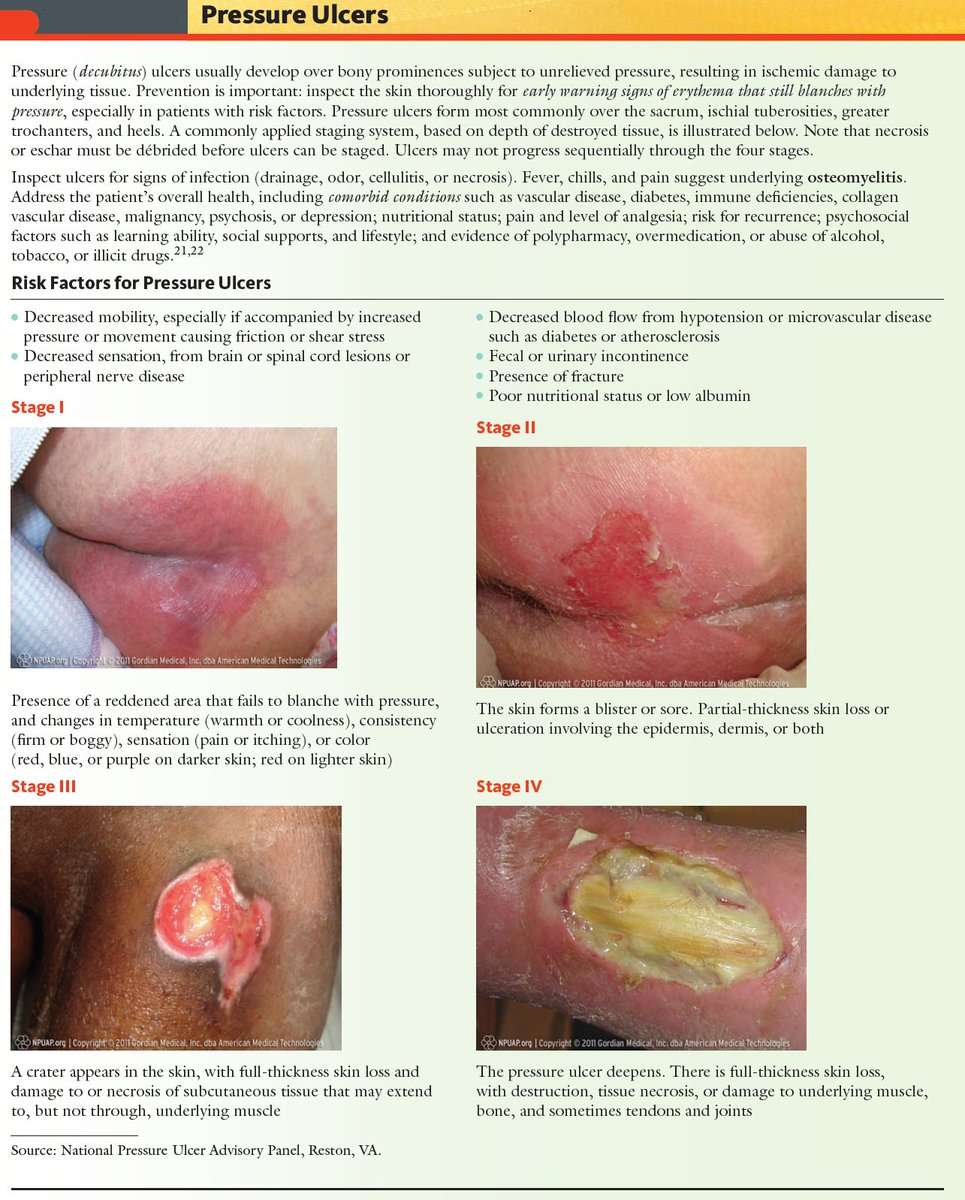
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
Also Check: Diabetic Foot Ulcer Treatment Guidelines
Bedsores And Nursing Home Neglect
Stage 3 bedsores in nursing homes are often caused by nursing home neglect. Many older adults and their loved ones rely on nursing homes and their staff to provide care. This is especially true when a resident has health problems that prevent them from moving, such as a spinal cord injury.
Nursing home staff members are trained to check on residents who are at risk of bedsores and help with repositioning. However, not all staff members follow through on their duty to help their residents.
Staff burnout, understaffing, and carelessness can prevent at-risk residents from getting the care they need. In these cases, nursing home staff members are directly responsible if a stage 3 bedsore develops.
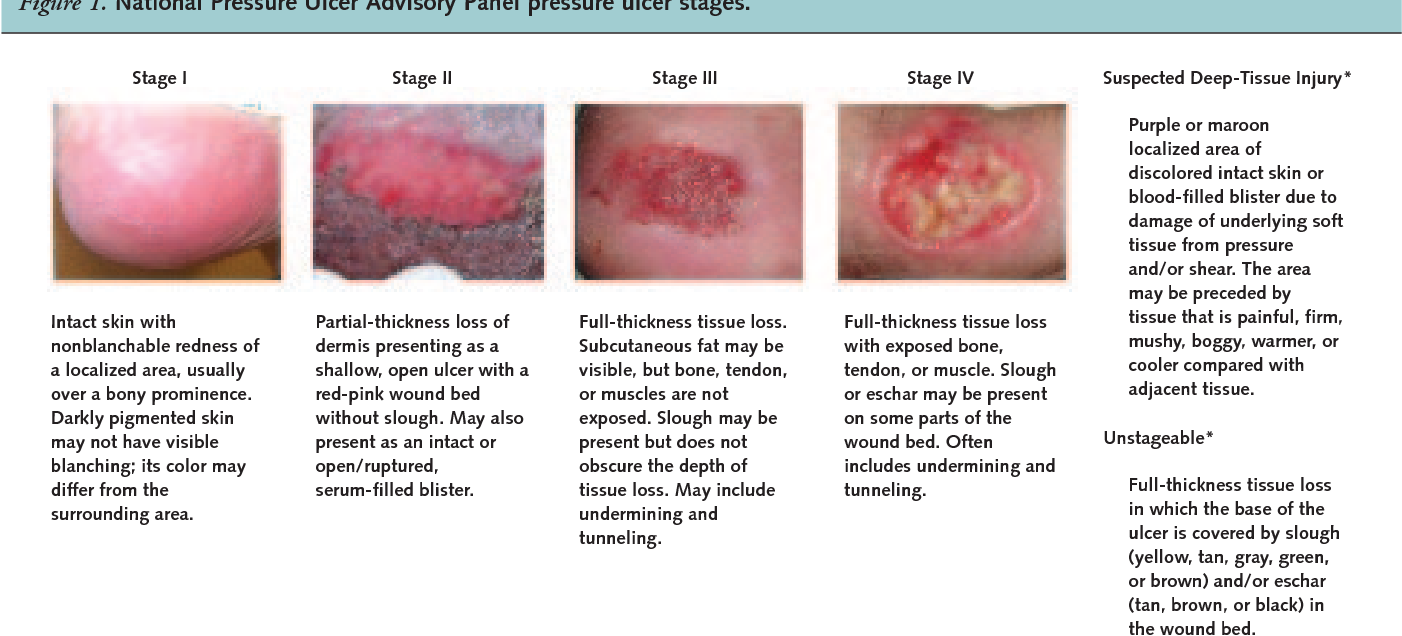
Stages Of Decubitus Ulcers
Stages of decubitus ulcers are classified from Stage I to Stage IV according to the severity of symptoms.
Stage Iâ In fair-skinned individuals, a defined skin area is characterized by persistent redness. Darker skin may come with hues of red, purple of blue. Compared to the other adjacent body area, the changes in the defined area involve skin temperature, sensation, and palpable or felt tissue consistency. When the define area is pressed, the skin does not turn to whiteâ a key indicator that decubitus ulcer has already started to occur.
Stage IIâ At this stage, the decubitus ulcer is still superficial. A blister, an abrasion, or a shallow crater or open sore has formed the surrounding area of which may appear to be irritated and red in color.
Stage IIIâ The superficial ulcer appears like a deep crater, where thick skin loss involves impairment in the skinâs underlying tissue. The depth of damage may reach the fascia, but does not pass through it.
Stage IVâ Further impairment takes place along with the fully thick skin loss. The depth of damage reaches the bone, muscle, or the supporting tendons and joint capsule. Furthermore, sinus tracts may also characterize Stage IV decubitus ulcers.
Also Check: What Foods Should I Eat With Ulcerative Colitis
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
-
absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
-
achieve freedom from particulate contaminants or toxic chemicals left in the wound
-
provide thermal insulation, in order to maintain the optimum temperature for healing
-
allow permeability to water, but not bacteria
-
optimise the pH of the wound
-
minimise wound infection and avoid excessive slough
-
avoid wound trauma on dressing removal
-
accommodate the need for frequent dressing changes
-
provide pain relief and
-
be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
Recommended Reading: How Effective Is Humira For Ulcerative Colitis
Protect The Periwound Skin
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or body fluids, to protect sensitive, fragile skin and severely dry skin, including periwound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab andAskina® Barrier Film Spray are sterile liquid dressings which form a transparent film when applied to the skin. The film possesses good oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Read Also: List Of Foods To Eat When You Have An Ulcer
Who Is At Risk Of A Pressure Ulcer
People immobile due to illness or injury are at greatest risk of getting a pressure ulcer.
- They may be unable to change position without assistance eg, see Skin complications of paraplegia and tetraplegia.
- They may have nerve damage from injury or illness, such as spina bifida, diabetes or stroke, and are unable to sense pain or the signals that normally make people move.
- Older people are at greater risk because their skin is thinner and more fragile.
- A pressure ulcer may develop underneath a plaster of Paris or fibreglass plaster .
Diagnosing A Stage 3 Bedsore
A medical professional relies on a bedsores appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patients skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough or eschar in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
Don’t Miss: What’s The Signs Of An Ulcer
Sacral Decubitus Ulcers Are A Certain Type Of Wound Located On The Lower Back At The Bottom Of The Spine
How to measure a sacral wound. Clock terms can also be used to describe the location of undermining. Use the body as a clock when documenting the length, width, and depth of a wound using the linear method. The braden risk assessment scale can be utilized to assess a patientâs risk of developing a pressure ulcer.
Get the wound depth using a cotton pledget or applicator dipped in a normal saline solution to measure the deepest part of the wound bed. Look closely at the wound and its edges, and then draw the wounds shape. Measure the wound how to measure wound size consistency is key.
Any adult who scores lower than 18 on the braden scale is high risk. For example, you might use words like jagged, red, puffy, or oozing to describe the wound.step 2, use a ruler to measure the length. Remove the applicator and hold it against the ruler to measure the depth of the wound margin based on.
This is particularly important when The total amount of tissue debrided should be listed separately from the wound measurements The six approaches for measuring wound area were simple ruler method , mathematical models , manual planimetry , digital planimetry , stereophotogrammetry and digital imaging method .
Step 1, draw the shape of the wound and write a brief description. Assessing and measuring wounds you completed a skin assessment and found a wound. In all instances of the linear method, the head is at 12:00 and the feet are at 6:00.
Archives Of Plastic Surgery