Symptoms Of Ulcerative Colitis Flares
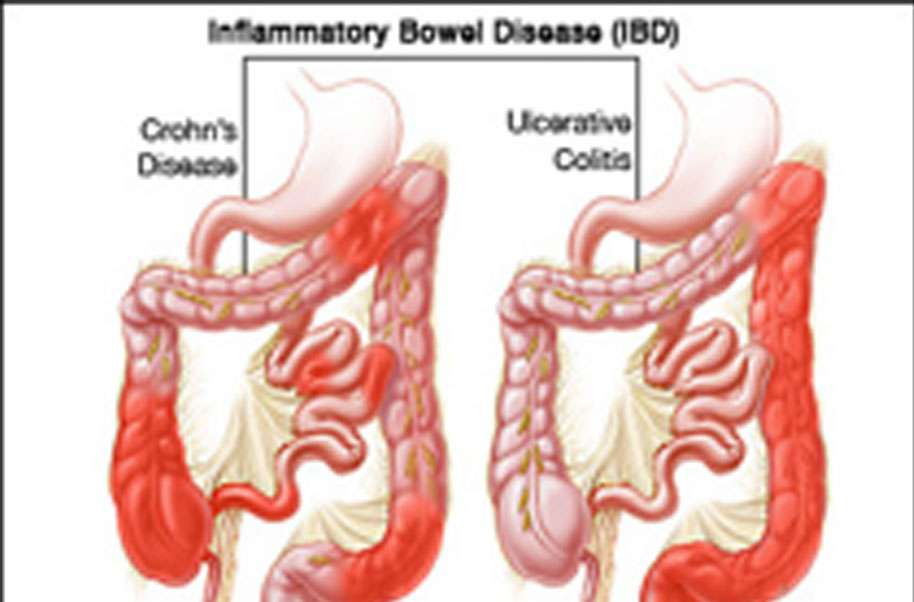
Ulcerative colitis happens when irritation and open sores appear in the large intestine. Its a kind of inflammatory bowel disease and can cause extremely uncomfortable ulcerative colitis flares.
An ulcerative colitis flare is when your disease symptoms reappear after a period of time without symptoms. Depending on where the inflammatory bowel disease is located in your gastrointestinal tract, youll have unique symptoms. Common symptoms of ulcerative colitis flares include:
- Frequent and urgent bowel movements
- Eye pain, redness, or difficulty seeing
What Are The Symptoms Of Ulcerative Colitis With Constipation
Thereâs no agreed-upon definition for UC with constipation. But a group of experts came up with a set of guidelines to better pinpoint it. In general, youâll need to have at least two of the following symptoms for at least 3 days a month during the prior 3 months:
- Bloating
- A sensation that you canât get all your stool out
Constipation may also cause:
- A sick feeling in your stomach
- Fatigue
The above symptoms can lead to other health issues, especially if you strain really hard when you poop. You may get:
- Tears or sores in the lining of your anus
- Swollen blood vessels around your anus
- Hard stool that gets stuck in your rectum
Inflammatory Bowel Disease Treatment Options
IBD is a lifelong disease, and at this point, people are rarely cured. However, thanks to advances in medication, gastroenterologists at CHI Health can help patients keep their condition in check and live an active, pain-free lifestyle.
The most common medications we prescribe include:
- Aminosalicylates: These treat mild to moderate Crohn’s disease by controlling inflammation in the lining of the gastrointestinal tract.
- Antibiotics: These treat symptoms and help heal infections.
- Biologics: These drugs treat people with moderate to severe disease, often if other drugs have not worked well. They don’t affect your whole immune system, so they tend to cause fewer side effects, although some side effects can be serious.
- Corticosteroids: These strong and fast-acting drugs can often relieve flares in moderate to severe Crohn’s within a few days. You usually take them in small doses for a short time because they can cause serious side effects.
- Immunomodulators: If you have moderate to severe Crohn’s, and you have not had luck with aminosalicylates or corticosteroids, your doctor may suggest one of these. They can help your body respond better to corticosteroids during a flare and help you stay flare-free longer.
Also Check: Can I Take Tylenol For Stomach Ulcer Pain
Warning Signs Of Perforated Bowel And Hemorrhaging
A perforated bowel is a hole in the wall of the intestine which can occur as a consequence of toxic megacolon, but can also be caused by intestinal infections, and certain types of medication.
A full colonoscopy during acute severe ulcerative colitis may also increase the risk of perforation, according to the January 2019 review in the BMJ Postgraduate Medical Journal.
This perforation is so dangerous because the contents of the intestine, which contain a large number of bacteria, can spill into the abdomen and cause a serious infection called peritonitis, notes the Crohn’s and Colitis Foundation.
Signs of bowel perforation include severe abdominal pain, a high fever, and heavy rectal bleeding or hemorrhaging. As a caregiver, look for, or ask about, sudden and dramatic increases in the amount of blood in your loved one’s stool.
If you suspect perforation, call 911 or go to the emergency room. Massive hemorrhaging in a patient with ulcerative colitis is an emergency condition that requires immediate medical attention and possibly surgical care to repair the hole in the colon wall.
RELATED: What Is Rectal Bleeding? Symptoms, Causes, Diagnosis, Treatment, and Prevention
Managing Uc To Treat Anemia
Getting UC under control through appropriate treatment treat anemia. There is no cure for UC, but a multifaceted approach to treatment can help manage the disease.
Treatment options for UC may include:
- Medications: Possible medications include aminosalicylates, corticosteroids, immunomodulators, targeted synthetic small molecules, and biologics. Medication can help limit flare-ups and reduce inflammation.
- Diet: Working with a doctor or dietitian to avoid foods that aggravate the digestive system may improve symptoms.
- Surgery: Between 2533% of people with UC do not benefit from medical therapy. For these people, doctors may recommend a surgery such as a colectomy.
You May Like: What Medicine Is Best For Stomach Ulcers
Treatment Options For Anemia
While anemia can be serious, it is also treatable.
Treatment options for anemia in people will UC will depend on the cause of the anemia and whether the UC is active.
A doctor will decide what treatment option is best, taking into account:
- whether UC is active
- whether other medical problems are present
- whether other nutritional deficiencies are present
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I cant bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I cant fully stand upright sometimes for a minute or so. Its frustrating.
Also Check: Ulcerative Colitis Shortness Of Breath
Tips For Managing Fatigue
- Keep a close eye on those blood testsChecking on iron levels, vitamin B12 and other chemical or nutrient deficiencies can help your treatment team to find the right mix of medication for you. Adding iron supplements or reducing the dosage of a medication can make a world of difference to energy levels for some people.
- Focus on keeping fitWhile being careful not to overstress yourself, try gradually increasing the amount of physical activity you do. Make use of a gym membership, walk rather than catching the bus for shorter trips, or commit to a team sport. Improving your overall fitness can ensure your energy stores are higher, potentially reducing the impact of those fatigue-ridden days.
- Assess your dietDo you have any foods that make you feel heavier, or sluggish? Complex carbohydrates such as cereals or porridge can provide you with energy over a longer time frame, while simple carbohydrates will give you a short burst of energy, often followed by a low. Consider if you are getting a good mix of fruits and vegetables, carbohydrates for energy, and rich protein.
- Manage your workloadWherever possible, ensure your workplace, family or education provider is aware of your condition and see what flexibility is available with responsibilities, work hours and prior planning. For example, taking the afternoon off following a doctors appointment may be a welcome break to rest, recover and prepare for the next week.
You May Like: Coconut Milk Good For Ulcerative Colitis
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: How To Heal Leg Ulcers Quickly
What Are The Signs And Symptoms Of Ulcerative Colitis
First, lets review: What isulcerative colitis, anyway? This condition occurs when your large intestinethat includes your colon and your rectumis chronically inflamed. Somehow, your immune systems signals got scrambled, so the body ends up attacking healthy cells as if theyre foreign invaders. The resulting inflammation is the root cause of most of its symptoms, too.
While most people associate the digestive system and intestinal issues with UC, not all UC symptoms stem from the large intestine. Because the inflammation of UC is systemic, it can affect your entire body, leading to problems like joint pain, extreme fatigue, and morenot to mention the stress and anxiety that can come with dealing with a serious chronic disease.
Heres a quick list of the main symptoms:
-
Blood or pus in your stool
-
Frequent diarrhea
-
Tenesmus, or when you have a sudden and constant feeling that you need to have a bowel movement
-
Abdominal pain or discomfort
Can The Immune Response To Covid
byKate Kneisel, Contributing Writer, MedPage Today March 1, 2022
A 50-year-old male patient presented to an outpatient clinic in the spring of 2020 with fever and dyspnea he told clinicians that the symptoms had persisted for the past 3 days.
Physical examination findings included a fever of 37.8°C , respiratory rate of 24 breaths/min, and heart rate of 105 beats/min. There was no organomegaly, and the patient was a non-smoker.
Initial laboratory test findings included:
- White blood cell count: 6.4 × 109/L
- C-reactive protein : 4.6 mg/L
- Ferritin: 162 ng/mL
- D-dimer: 842 ng/mL
Findings of a polymerase chain reaction test for SARS-CoV-2 were negative. However, the patient’s wife and two children had positive PCR test results and the patient’s CT chest scan revealed diffuse ground-glass opacities consistent with viral pneumonia. Clinicians diagnosed him with COVID-19, and he was started on a now-debunked 7-day regimen of hydroxychloroquine and azithromycin. Once he was clinically stable, he was released with instructions to return for a follow-up assessment.
On follow-up assessment 1 week later, the patient reported no improvement in symptoms. His stool calprotectin level was 1800 g/g . Endoscopy revealed a diffuse, micro-ulcerated, granulated appearance that clinicians noted continued uninterrupted from the dentate line to the sigmoid colon, as well as distortion of the submucosal vascularization.
Discussion
Disclosures
Also Check: What Does A Mouth Ulcer Look Like
Alarm Symptoms Of Ulcerative Colitis:
If you are already diagnosed with ulcerative colitis, there are several alarm symptoms to look out for. A change in your ulcerative colitis symptoms may mean that additional treatment is needed. Talk to your doctor immediately if you experience a new symptom, a change in your current symptoms or any of the following:
- An unusual amount of cankers or sores in your mouth
- Unexplained or unintentional weight loss
- Failure to gain weight
- Delayed puberty in teens
- Drainage of pus from, or severe pain near, the anus which is usually caused by an abscess.
- Anemia this blood condition results in fatigue and weakness. It is usually caused by heavy blood loss or a lack of dietary iron
- Rectal bleeding
Crohns Disease And Ulcerative Colitis

A serious but rare complication of these forms of inflammatory bowel disease is fulminant or toxic colitis, formerly called toxic megacolon.
The signs and symptoms of this condition can include bloody diarrhea along with fever, racing heartbeat , low blood pressure , metabolic acidosis , low urine output , and acute kidney failure.
Toxic colitis is more common with ulcerative colitis than it is with Crohns disease.
Recommended Reading: Herbal Tea For Ulcerative Colitis
Reducing Your Arthritis Risk When You Have Ulcerative Colitis
Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis werent enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although its not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.
Also Check: Signs And Symptoms Of Peptic Ulcer
Causes Of Ulcerative Colitis Flares
Ulcerative colitis flares can be caused by a variety of things, including:
- Skipping medications or not taking the correct dose. If you regularly take medicine for your ulcerative colitis, you need to be consistent even when your disease is in remission. If you dont follow prescription instructions, flares can occur.
- Taking non-steroidal anti-inflammatory drugs. Common drugs like aspirin, naproxen, and ibuprofen can inflame the bowel and bring on serious symptoms. If you need mild pain relief or fever treatment, you should take acetaminophen.
- Taking antibiotics. Although theyre useful when you have bacterial infections, they affect the bacteria that live in your intestine. These changes can result in diarrhea or the growth of too much of a certain bacteria that then causes inflammation. If you have a bacterial infection, make sure your healthcare provider knows you have ulcerative colitis.
- Not managing stress. Physical and emotional stress can bring on flare-ups. Once you understand that stress causes such a reaction, you can find out what stress management strategies work to keep flare-ups at bay.
- Eating and drinking triggering items. The foods and drinks that bring on symptoms vary by person. Youll need to track your diet so you can pinpoint triggering items when you experience ulcerative colitis flares.
Don’t Miss: What Medicine Is Good For Ulcers
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Also Check: Best Probiotic For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.