Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
-
Ovid MEDILINE
-
Ovid MEDLINE
-
Ovid Embase
-
EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
-
ClinicalTrials.gov
-
WHO International Clinical Trials Registry Platform
-
EU Clinical Trials Register .
Searching other resources
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
You May Like: How Do They Treat Ulcerative Colitis
Dressings For Pressure Sores
If your skin has broken down you may need to have a dressing on it. The dressing protects the area, keeps it clean and moist and helps it to heal.
There are different types of dressings, the one you need will depend on your wound. These could include:
- alginate dressings, made from seaweed
- Clear film dressings, like medical cling film
- gels put on to the wound that soak up fluid
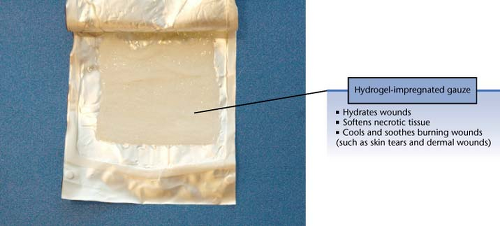
- hydrogel, which keeps wounds moist and helps to clean them
- foam dressings that absorb fluid from the wound
- honey dressing
- silver dressing
Your nurse will assess your pressure sore to decide which dressing is best for you, change it as needed and monitor how well it is working.
Recommended Reading: What Foods Can You Eat When You Have An Ulcer
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Stage 4 Bedsore Prevention

The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
Also Check: How To Get Remission In Ulcerative Colitis
Read Also: What To Do When Ulcerative Colitis Flares
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Data Collection And Analysis
Two review authors independently performed study selection, risk of bias assessment and data extraction. We conducted network metaanalysis using frequentist megaregression methods for the efficacy outcome, probability of complete healing. We modelled the relative effectiveness of any two treatments as a function of each treatment relative to the reference treatment . We assumed that treatment effects were similar within dressings classes . We present estimates of effect with their 95% confidence intervals for individual treatments compared with every other, and we report ranking probabilities for each intervention . We assessed the certainty of the body of evidence using GRADE for each network comparison and for the network as whole.
Don’t Miss: Indian Diet For Ulcerative Colitis
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
Recommended Reading: Herbal Medicine For Ulcerative Colitis
Potential Biases In The Review Process
This was a sparse network and there may have been smallstudy effects which impacted on the network . The STATA routines have largely been developed for and tested on larger networks, and our work has contributed to modifications for sparse networks in the netweight routine. Other STATA routines can be modified by the user to take into account smallstudy effects, but we did not explore these approaches because there was too much uncertainty in the network for us to be confident of interpreting the results. Instead, we used the standard routines for NMA and adapted the recent approach to GRADE to bring in sparseness when assessing evidence certainty.
A further effect of the sparseness of the network may have been to hide any inconsistencies. The various statistical tests for inconsistency were generally not significant, but this may have been due to a lack of sensitivity of the tests and the wide CIs around the measures. Despite this, we found inconsistencies in the network for contrasts involving phenytoin. We cannot be sure that there are no other inconsistencies, but this may not matter given the already identified large uncertainties.
Read Also: What Medicine Is Best For Stomach Ulcers
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation |
|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
-
absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
-
achieve freedom from particulate contaminants or toxic chemicals left in the wound
-
provide thermal insulation, in order to maintain the optimum temperature for healing
-
allow permeability to water, but not bacteria
-
optimise the pH of the wound
-
minimise wound infection and avoid excessive slough
-
avoid wound trauma on dressing removal
-
accommodate the need for frequent dressing changes
-
provide pain relief and
-
be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
You May Like: How To Relieve Mouth Ulcer Pain
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Risk Of Bias In Included Studies
Risk of bias for all included studies is summarised in . In order to represent ‘very high’ risk of bias, we have used two columns so very high risk of bias occurs when the cell is red in the final column .
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
We judged only one of the 51 studies to be at low risk of bias and ten to have unclear risk of bias . We judged 14 studies to be at very high risk of bias, that is, to have high risk of bias for two or more domains . We assessed the rest of the studies at high risk of bias. We grouped the low and unclear categories together.
*Studies marked with an asterisk were not included in the individual network.
Don’t Miss: Is Colitis And Ulcerative Colitis The Same Thing
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
Read Also: Classic Features Of Ulcerative Colitis
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Recommended Reading: Bleeding Ulcer Treatment At Home
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
Recommended Reading: Best Medicine For Ulcerative Colitis