What Other Kinds Of Aids Are Available
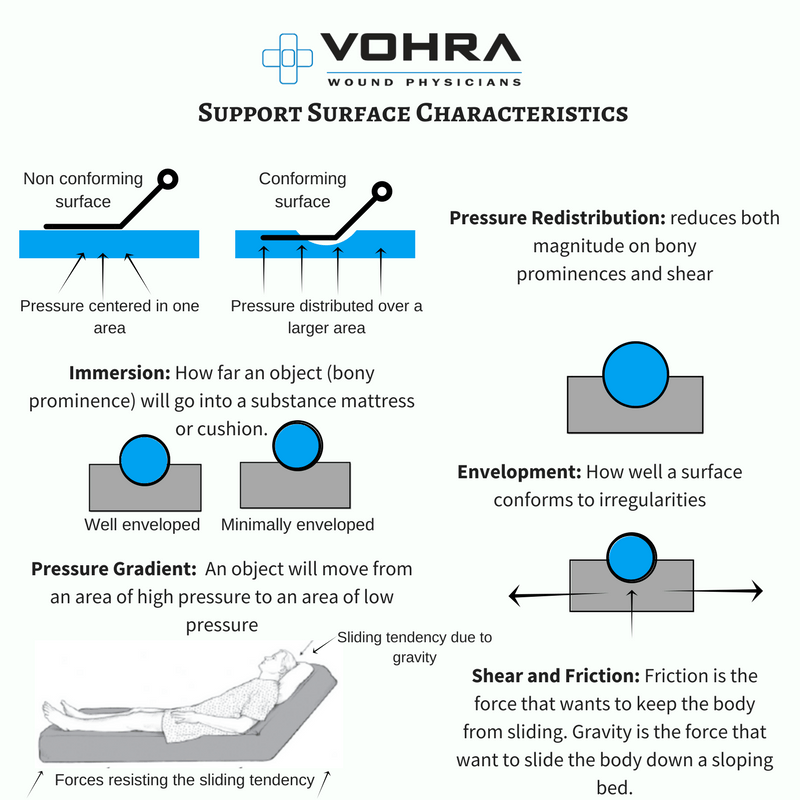
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
What Are Pressure Ulcers Exactly
The injuries have been known by various names, including bedsores, pressure sores and decubitus. Pressure ulcer is now the term preferred by healthcare professionals, and it is defined as a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction.
The mechanism by which the damage occurs is that compression prevents efficient blood flow to the area, so the tissues are deprived of oxygen, leading to damage and death. A pressure ulcer has been likened to an iceberg, in that what is visible at the surface is just a small proportion of the injury that lies beneath.
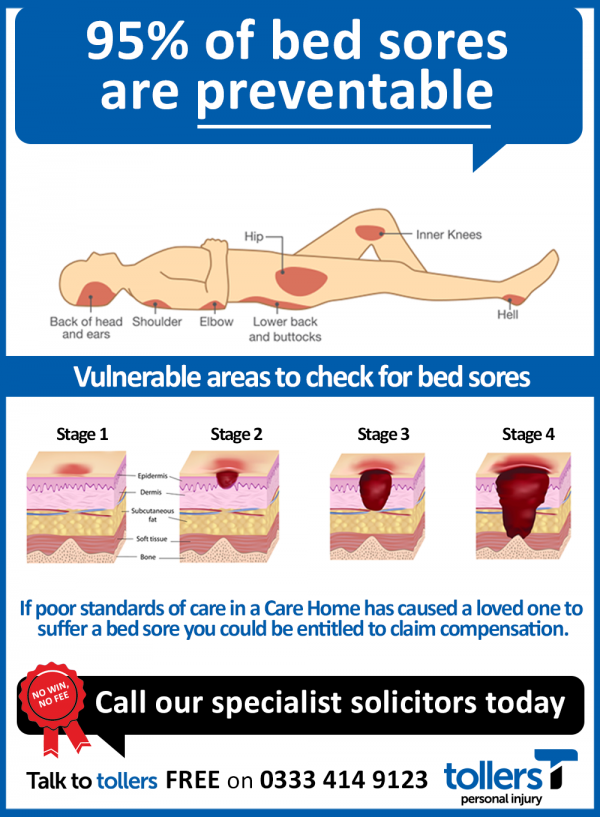
The most common places to develop pressure damage are the heels and sacrum, followed by buttocks, elbows, ankles and hips: generally, areas where bone is close to the surface, with less padding for protection. It is the tissue nearest to the bone that is damaged first, with the surface of the skin being the last to be affected.
Pressure ulcers are categorised from I to IV, according to severity.
Pressure Ulcers: Applying All Our Health
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/pressure-ulcers-applying-all-our-health/pressure-ulcers-applying-all-our-health
Read Also: Can Food Allergies Cause Ulcerative Colitis
Encourage Seniors To Maintain A Healthy Diet
The benefits of a well-functioning circulatory system are only as good as the nutrients it delivers. Seniors should strive to eat a well-balanced, healthy diet, explains Medscape. In fact, optimizing the nutritional status of a senior living with a pressure sore is key to ensuring successful treatment. For seniors living with metabolic disorders, such as diabetes, a healthy diet can go much further than simply preventing or encouraging the healing of pressure sores.
What Are Pressure Areas
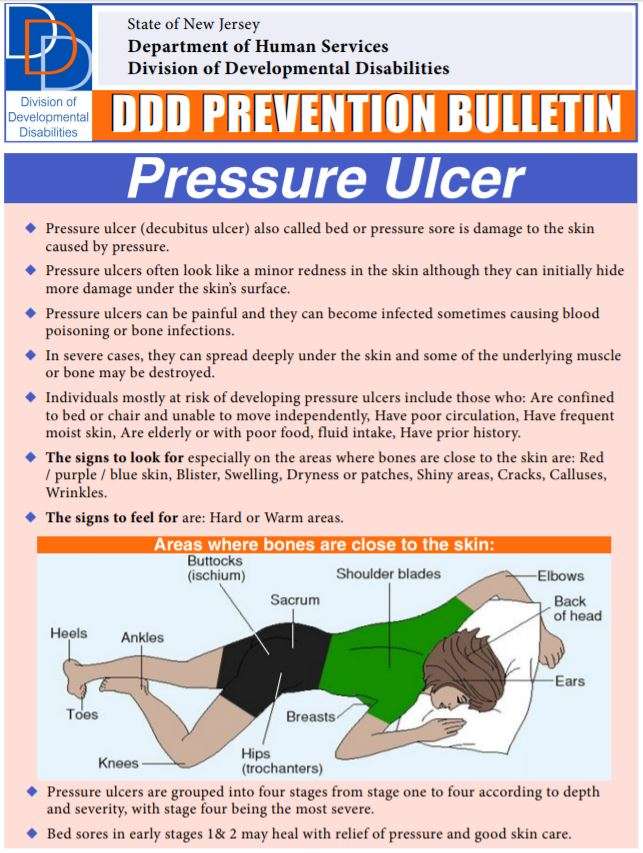
The most common sites are the back of the head and ears, the shoulders, the elbows, the lower back and buttocks, the hips, the inner knees, and the heels. Pressure injuries may also form in places where the skin folds over itself. And they can occur where medical equipment puts pressure on the skin.
Also Check: How To Heal Ulcers In Large Intestine
People At Highest Risk For Pressure Ulcers
Anyone can develop a pressure ulcer, but some people have a higher risk and should be monitored more closely for signs of skin breakdown. Aside from those who are immobile, others include people who have:
- Fragile skin that tears easily
- Dementia
- A chronic illness like diabetes, that can affect your blood flow
Or are:
- Smokers
What Are Pressure Ulcers
Pressure ulcers are damaged areas of skin and/or tissue under the skin. They are most common over bony parts of the body, where the persons body rests against a chair or bed.
There are different categories of pressure ulcer, ranging from intact skin that may be discoloured or painful, to open ulcers or wounds that affect the tissue under the skin. They may develop gradually over time or more quickly, over a few hours or less.
Its important to find and treat pressure ulcers quickly to prevent pain and damage to the muscle or bone under the affected area of skin. Untreated pressure ulcers can lead to unnecessary pain, infection and someone may need to stay in hospital.
Pressure ulcers are sometimes called pressure sores, bed sores, pressure injuries or deep tissue injuries.
Don’t Miss: Is Garlic Good For Ulcerative Colitis
What Are 3 Interventions We Commonly Use To Prevent Worsening Of Pressure Ulcers
Prevention includes identifying at-risk persons and implementing specific prevention measures, such as following a patient repositioning schedule keeping the head of the bed at the lowest safe elevation to prevent shear using pressure-reducing surfaces and assessing nutrition and providing supplementation, if needed
Facts About Pressure Ulcers
NHS Safety Thermometer reported that from April 2014 to the end of March 2015, just under 25,000 patients were reported to have developed a new pressure ulcer, and on average 2,000 pressure ulcers are newly acquired each month within the NHS in England.
Older people are the most likely group to have pressure ulcers this is especially true for those older than 70, up to a third of whom will have had surgery for a hip fracture. Age alone is not a risk factor rather, it is the problems common in older people that are associated with pressure ulceration .
Those with spinal injuries form another distinct group, in whom the prevalence is 20% to 30%, 1 to 5 years after injury.
Pressure ulcers in older patients are associated with a fivefold increase in mortality, and in-hospital mortality in this group is 25% to 33% .
Pressure ulcers can result in longer lengths of stay in hospitals. One study found that adult patients who develop pressure ulcers had an extended stay of over 4 days . Another study found patients over 75 years of age, who develop a pressure ulcer in hospital, had a 10 day longer stay .
The cost of treating a pressure ulcer varies from £1,214 to £14,108 costs increase with severity because the time to heal is longer and the likelihood of complications are higher in severe cases .
You May Like: What Is The First Sign Of Stomach Ulcer
What Categories Of Pressure Ulcers Are There
The Dutch scientific association of family physicians, the NHG, speaks of four degrees of pressure ulcers:
Grade 1
These are superficial wounds that look like shallow abrasions. A patient is most likely to develop this type of pressure ulcer when body weight is very high or, on the contrary, body weight is very low and activity levels are low.
Grade 2
Pressure ulcers have now progressed to deeper layers of the skin. This is accompanied by additional discomfort for the patient.
Grade 3
These are wounds that are deep enough to affect underlying tissues, blood vessels and bones. These may require stitches and a tetanus injection, or sometimes more serious medical treatment.
Grade 4
This is the worst kind of wound. A severe form of pressure ulcer often requires multiple stitches and special attention from the doctor. These wounds are usually larger than 7 inches.
Why Are Older Adults At Risk For Pressure Ulcers
Diseases related to neuromotor and skeletal muscle disorders impair quality of life, self-care, and functional capacity among the elderly, consequently interfering with nutrition and levels of sensory perception, mobility, activity, and moisture, which are classic risk factors for pressure ulcer development.
Also Check: Is Alcohol Bad For Ulcerative Colitis
The Cost Of Pressure Damage
The cost of pressure damage is enormous. First and most importantly, these are extremely painful wounds, which bring a great deal of suffering to the individual concerned.
The financial cost to the NHS has been estimated to be between £1,760 million and £2,640 million each year â approximately 4% of its total budget â making pressure ulcers the single most costly chronic wound to the Health Service. These figures have been arrived at based on typical costs for treating pressure ulcers, which are £1064, £4402, rising to £7313 and £10,551 for wounds of Category I through to IV.
It is widely believed that the prevalence and cost of pressure ulcers is understated, as the majority of studies have been based on hospital populations, where just 11% of cases are found. In fact, it is likely that some 20% of care home residents and 30% of people cared for in the community will develop pressure ulcers.
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
Also Check: Can Ulcerative Colitis Cause Low Testosterone
Looking For This Assignment Or A Similar One We Have Had A Good Success Rate On This Paper Order With Us Today For Quality Work And Get A Discount
Disclaimer:
All types of paper that Discount Writers provides is only for the purpose of assistance! No text, paper, assignment, discussion would be similar with another student therefore guaranteeing Uniqueness and can be used with proper references only!
More tools: Better Grades: Choose your Homework Help:
Assignment Help: We would write your papers according to the instructions provided and guarantee you timely work
Entire Online Class Help: We are here for you and we would do your entire Class work from discussions, assignments, Replies, Exams and Quizzes at a Cost
Exam/ Quiz Help: We have a team of writers who specialize on exams from any specific field and we would give you an A+ Grade!
Dont Miss: Best Things To Eat With Ulcerative Colitis
What Causes Pressure Ulcers
Pressure ulcers are caused by ongoing pressure to the skin, for example if someone spends a lot of time sitting or lying in the same position. They can develop after only a few hours, whether the person is in hospital, a hospice, a care home or living in their own home.
They may also happen if the layers of skin are forced in opposite directions, for example when someone slides down in bed or slides across to a chair.
Another possible cause is medical or other equipment rubbing against the skin . For example, catheters, oxygen tubing, glasses or shoes. Someones skin may also be damaged if theyre moved without using the correct moving and handling techniques.
Someone may have a higher risk of pressure ulcers if they:
- spend a lot of time in bed or a chair
- arent able to move easily, for example because they feel sore, are short of breath or have low mood
- have a history of pressure ulcers
- have diabetes, smoke heavily or have circulation problems
- have lost sensation in their skin due to their illness or medication.
You should regularly assess someones risk of getting pressure ulcers. If you havent had training on this, ask your manager if theres training you can attend.
Don’t Miss: How To Test For Ulcerative Colitis
Preventing Pressure Sores By Self
It is important to understand how and why pressure sores form. Once you do you can help to prevent pressure sores from forming by trying the following methods.
- Use moisturizing creams daily
- When bathing only use a soft sponge. Do not scrub hard
- Be sure to clean areas and dry properly in areas that could stay moist
- Do not shower or bathe daily as this can be counterintuitive and dry out your skin
- Stay clear of strong soaps
- Stay clear of talc powders
What you wear matters. Keep the following in mind when dressing.
- Do not wear clothes that are really tight
- Try and not to wear clothes that have buttons or seams that are thick. This can rub against the skin or cause unnecessary pressure points
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
Recommended Reading: How To Heal Mouth Ulcers
Ways To Prevent Pressure Ulcers
1. Risk Assessment: risk assessment tools, such as the Braden scale, help caretakers recognize a patients risk of developing pressure ulcers. Clearly documented risk assessment is vital in preventing and treating pressure ulcers.
2. Skin Inspections: a patients skin should be examined regularly for signs of pressure damage. The first sign of tissue damage is often non-blanching erythema. Other signs of skin damage include heat, induration and swelling.
3. Skin care: keeping a patients skin clean, dry, and hydrated can help prevent damage. Skin should be dried carefully and any rubbing or friction should be avoided.
4. Moisture: excessive perspiration, oedema and incontinence can cause skin damage from excess moisture. Incontinence can be particularly harmful to a patients skin and appropriate measures should be taken to prevent any associated damage.
5. Incontinence: incontinence and pressure ulcers often co-exist. The use of incontinence pads with the appropriate application of a barrier cream can be helpful, while the use of indwelling urethral catheters should only be considered as a last resort due to the risk of infection.
6. Nutrition: good nutrition is essential for pressure ulcer prevention and healing. A Patients diet should be assessed regularly and any nutritional needs should be addressed. Keeping patients hydrated is also a vital part of preventing pressure ulcers.
Enjoyed this Post?
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Don’t Miss: Ulcer In My Stomach Symptoms
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
Family And Individual Level
Healthcare professionals can have an impact on an individual level by:
- recognising the important role individuals, families and carers have in preventing and managing pressure ulcers
- engaging individuals, carers and families in what to look for and how pressure ulcers can be prevented
- using appropriate literature with visual images to explain how quickly pressure ulcers can develop
- educating the individuals and caregivers about the causes, assessment and management of pressure ulcers
- using appropriate terminology recognising and informing patients that pressure ulcers is another term for bed sores
- encouraging individuals to move independently whenever possible
- directing individuals to appropriate healthcare professionals if they suspect a pressure ulcer is forming or is present
- looking out for skin discolouration or soreness, particularly in areas where bones are close to the skin
- repositioning or turning patients frequently at least every 2 hours for those patients who need help
- using moving and handling aids to help reposition individuals who require assistance moving
- performing regular skin inspections to check areas at risk and document pressure areas at least once a day
- checking that patients with pressure ulcer risk factors are registered with a GP and receive primary health care support to minimise the risks
- providing holistic health assessments for people at risk of developing pressure ulcers
Recommended Reading: Is Nexium Good For Ulcers