Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
What Is Ulcerative Colitis
Ulcerative colitis is a disease in which there is chronic inflammation of the inner lining of the colon. The inflammation can cause the lining tissue to break down, forming ulcerations that can bleed. Inflammation can involve the entire colon or only parts of it. Almost always, ulcerative colitis requires treatment.
Living With Ulcerative Colitis And Kidney Disease
If you are living with UC and kidney disease, it is important to maintain a healthy lifestyle. Many MyCrohnsAndColitisTeam members have shared their tips on how they live with UC and kidney disease. I have regular appointments with my urologist/kidney specialist to check my blood and urine, one member noted. Another said, I exercise and stay at a good weight, while a third member wrote, I try to get enough potassium and vitamin D in my diet.
Other ways to manage UC and kidney disease include:
- Maintaining a healthy, well-balanced diet
Recommended Reading: Vsl 3 And Ulcerative Colitis
Do I Need To Be Screened For Colon Cancer
Yes. Everyone needs to be screened for colon cancer beginning at 50 years old. But if you have IBD, your risk of colon cancer is higher. You might need to be screened at a younger age or more often than people without IBD.
- Talk to your doctor about when to begin colon cancer screening, what tests to get, and how often to have them.
- Your doctor’s suggestions will depend on your family health history, how long you have had IBD, whether your colon is affected by your IBD, and how severe it is.
- If you have had IBD for 8 to 10 years, your doctor may recommend a colonoscopy with biopsies every 1 to 2 years. This test checks for early warning signs of cancer.
Can Changing My Eating Habits Help Treat Ibd
Maybe. Researchers don’t have enough evidence yet to show which specific diets, foods, or ingredients may make IBD symptoms worse or better. Some women say that changing the foods they eat helps relieve their symptoms during flare-ups. Most doctors recommend avoiding processed foods and foods with a lot of additives, such as carrageenan and maltodextrin .
Talk to your doctor about specific foods you may want to eat or avoid.21
Read Also: Natural Supplements For Ulcerative Colitis
Can Ulcerative Colitis Cause Urinary Problems
Patients with inflammatory bowel disease and irritable bowel syndrome often show evidence of bladder hypersensitivity such as detrusor instability, nocturia, frequency and some forms of urinary urge incontinence, back pain and, in women, dyspareunia, leading to significant problems in diagnosis and
You May Like: Do Kidney Stones Pass Through The Bladder
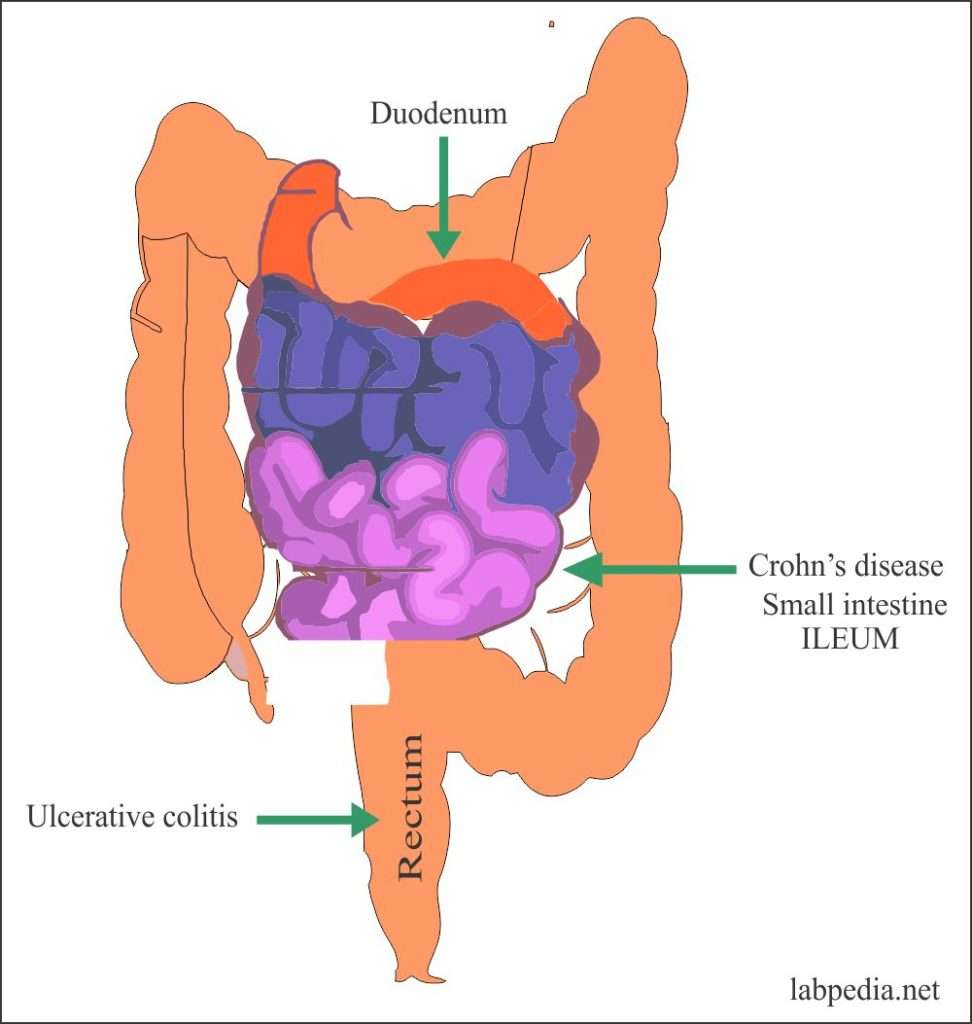
Colitis And Crohns Disease
Colitis and Crohns disease are Inflammatory Bowel Diseases where the intestines can become swollen, inflamed and ulcerated. The symptoms for these conditions include abdominal pain, loss of weight, diarrhoea, urgent need to go to the toilet, and tiredness. These symptoms will vary from person to person and can be more extreme for one person and not for another.
Diarrhoea caused by IBD is often accompanied by blood and mucus, especially with Ulcerative Colitis. The symptoms not only vary from person to person but may flare-up or improve/ go into remission unpredictably.
You May Like: Surgical Management Of Ulcerative Colitis Ppt
How Is Ibd Treated
Treatments for IBD may include:
- Medicines. Most people with IBD take medicine to control their symptoms.
- Surgery. Surgery may be an option if medicine does not work to control your symptoms. Learn more about surgery for Crohn’s disease and surgery for ulcerative colitis.
- Steps you can take at home. Your doctor can talk to you about steps you can take at home to help control your symptoms and prevent flare-ups.
- Changes to your eating habits. Avoiding certain foods, changing other eating habits, and limiting or avoiding alcohol may help control your symptoms during flare-ups.
Some forms of psychotherapy, sometimes called “talk therapy,” may also help you cope with stress related to IBD symptoms and help make your pain less severe.14 Your doctor can refer you to a counselor or therapist, or you can find one at .
Some counselors specialize in working with people who have IBD. A counselor can help you talk about any distressing emotions you might have about IBD symptoms. A counselor can also treat anxiety, depression, or other mental health concerns. Ask your doctor or nurse for a referral or recommendation for a counselor in your area.
Ibd Medications And Kidney Problems
The medications you take for IBD can sometimes cause issues with kidney function. Mesalamine and immunosuppressive medications like cyclosporine can sometimes change kidney function by causing the blood vessels in the kidneys to constrict, but this effect is very rare.
However, studies have found that other medications, such as aminosalicylates, methotrexate, and azathioprine, do not negatively affect estimated glomerular filtration rate , which is used to measure kidney function.
Read Also: Do You Still Have Ulcerative Colitis After Colectomy
Talking To Your Doctor
If you have noticed any of the symptoms listed above, talk to your doctor about your concerns. He or she may refer you to a specialist to treat your symptoms and to perform the necessary tests to determine if you do in fact have IBD.
Your doctor will want to hear about all your symptoms, any changes in medication, and any stressful life changes that may have recently happened. Be sure to write down all your questions before your visit so that you dont forget them during your appointment.
IBD can be a difficult condition to live with, but by talking to your doctor and finding treatment, it can be managed.
Need help finding a specialist near you? Try our doctor finder!
Unique Mechanisms In Ibd Patients Prompt Revised Guidelines
Although both gallstones and kidney stones may be associated with IBD, the studys authors described different mechanisms that may influence their development. Without sufficient ileal activity, for example, they noted that a patients bile may contain excess bilirubin, which may form gallstones. Furthermore, a patient with IBD may experience multiple effects in the digestive tract that potentiate a risk of gallstones.
Kidney stones typically form due to a high abundance of oxalate or similar compounds in the urine, according to the study publication. IBD may result in more concentrated urine due to factors such as dehydration from diarrhea and dysregulation of absorptionof salts in the ileum. An ileostomy may also result in urine that is more acidic.
Dr.Fagagnini and her co-authors suggested that clinical trials further explore treatment and relationships between IBD and the development of gallstones and kidney stones. Specifically, they recommended studying the use of ursodeoxycholic acid in IBD patients at risk of gallstones and a diet low in oxalate and high in fluid, with decreased ingestion of some fatty acids, for IBD patients at higher risk of kidney stones.
The authors disclosed no competing financial interests.
Recommended Reading: Ulcerative Colitis Flare Up Treatment Guidelines
Symptoms By Type Of Ulcerative Colitis
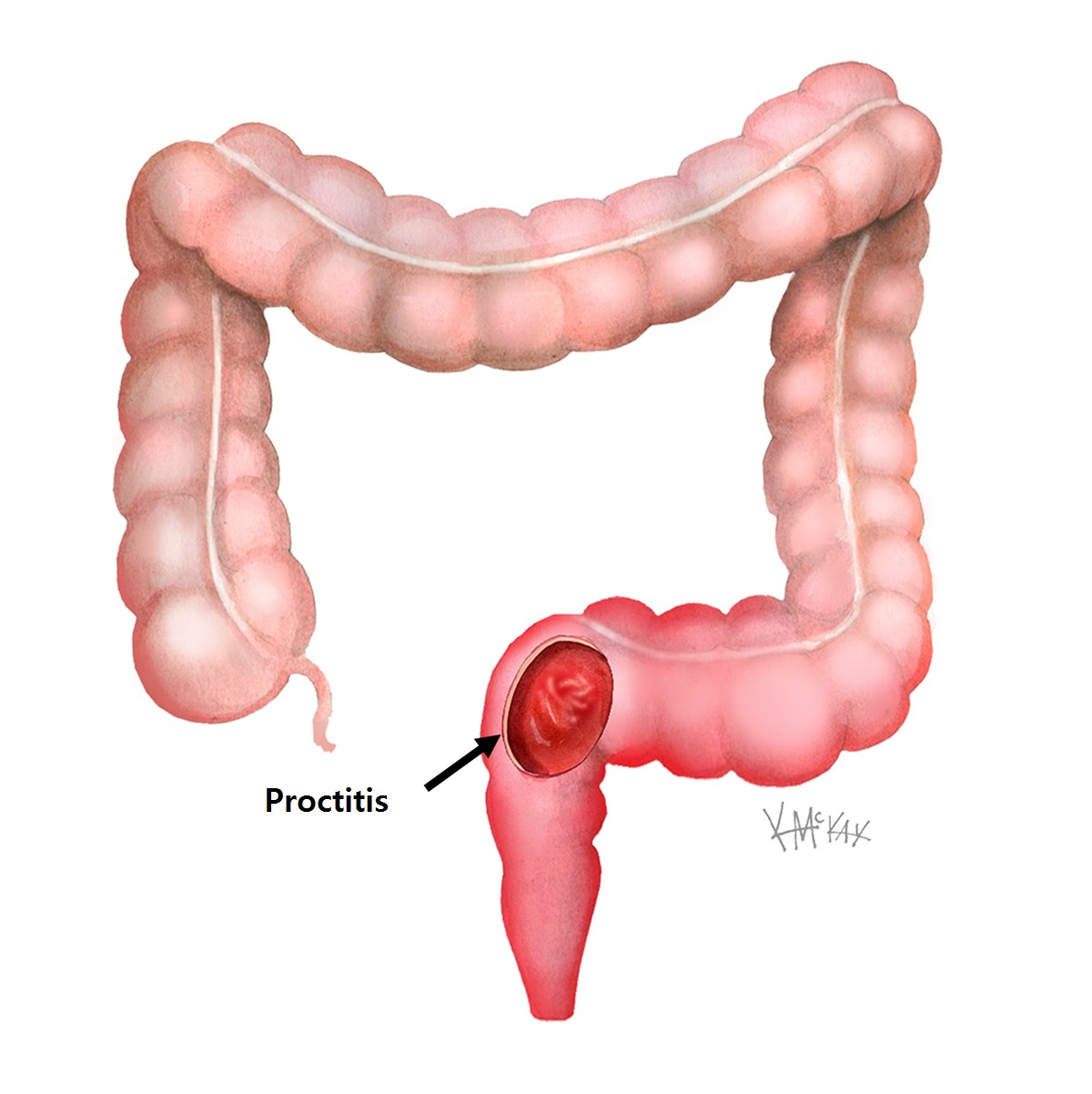
Ulcerative colitis can be broken into subtypes depending on where the inflammation is in your colon.
- Ulcerative proctitis. Ulcerative proctitis affects your rectum, the part of your colon closest to your anus. Its the most common type and affects 30 to 60 percent of people with ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis causes inflammation of your rectum and the lower part of your colon, called the sigmoid colon.
- Left-sided colitis. Left-sided colitis affects your rectum, your sigmoid colon, and the descending part of your colon on the left side of your body.
- Pancolitis.Pancolitis affects your entire colon.
Symptoms typically become worse as inflammation spreads farther along your colon.
| Ulcerative proctitis |
show ulcerative colitis is slightly more prevalent in men, but most studies show no difference.
Symptoms of ulcerative colitis are similar regardless of sex, but unique issues may occur for some people.
Rectovaginal fistulas may develop, which are holes that allow stool to leak from the bowel to the vagina.
Ulcerative colitis may also lead to irregular periods or increased menstrual pain. Women may also be at a higher risk of anemia and osteoporosis, and ulcerative colitis can further increase this risk.
Living With Uc: Supplements
The bleeding caused by ulcerative colitis may lead to iron deficiency anemia due to the loss of the body’s store of iron in the red blood cells that are lost into the colon. Iron supplementation may be necessary. Medications used to treat ulcerative colitis may reduce the absorption of nutrients such as folic acid and calcium. Supplements of vitamins and minerals may be necessary.
Don’t Miss: Ulcerative Colitis Medication Not Working
Urgent Care For Ulcerative Colitis
During a flare of ulcerative colitis, treatment is important to avoid complications. The most common complication is bleeding that can lead to anemia. With a severe flare, the colon may stop working and dilate . If not successfully treated, the colon may rupture and become a medical emergency. If treatment is not successful, surgery may be necessary. Usually, the entire colon is removed.
How Often Does Ulcerative Colitis Go Into Remission
In this Article. When you have ulcerative colitis, it can be hard to predict exactly how youll feel over the long haul. Usually, you go back and forth between flare-ups and remission. But like any long-term disease, youre bound to see changes. Flare-ups might take days or weeks. Remission might last for months or even years.
Recent Posts
Recommended Reading: History Of Ulcerative Colitis Icd 10
Ulcerative Colitis Or Crohns Disease
Ulcerative colitis is related to Crohn’s disease, another chronic inflammatory disease of the intestines however, Crohn’s disease, unlike ulcerative colitis, is not limited to the colon. In fact, Crohn’s disease usually involves the small intestine or small intestine and colon although occasionally it, too, is limited to the colon. Another chronic gastrointestinal disorder, irritable bowel syndrome, shares with ulcerative colitis abdominal pain and diarrhea as its main symptoms however, the cause of irritable bowel syndrome is believed to be dysfunction of the nerves and muscles of the intestines since there is no identifiable inflammation.
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Don’t Miss: Treating Hindgut Ulcers In Horses
When Should Someone Contact A Doctor About Colitis
Diarrhea is a common sign of colitis. It is usually self-limited and resolves on its own with supportive care, including rest and a short course of a clear-fluid diet. However, seek medical care if diarrhea persists for more than two to three weeks, if there is blood in the stool, fever, or the person has signs of dehydration.
- Blood in the stool is never normal and should always be evaluated. Common causes of blood in the stool include hemorrhoids however, other serious causes of bleeding need to be investigated. Colitis is not the only cause of rectal bleeding. Other causes include diverticular disease of the colon , colon polyps, anal fissures, and cancer.
- Chronic diarrhea may lead to dehydration and changes in the electrolyte balance in the body. If it is severe enough, the dehydration may require treatment with IV fluids or oral rehydration therapy. The symptoms of dehydration may include
- lightheadedness , especially when changing from a sitting or lying position to a standing position
- weakness
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: What Does It Feel Like To Pee A Kidney Stone
Don’t Miss: How Do You Know You Have A Stomach Ulcer
E Coli Infections Can Be Mild To Life
The strain of E. coli that most commonly causes hemorrhagic colitis is E. coli 0157:H7. Other strains of E. coli may also cause the infection, but they are hard to identify.
What makes these E. coli different from harmless E. coli is that they produce a toxin that damages the lining of the colon, causing inflammation and bleeding, says Dr. LoSavio.
Toxins are substances made by bacteria that are poisonous to humans. The toxin made by E. coli 0157:H7 is called Shiga toxin. Shiga toxin allows the bacteria to cling to cells lining the colon and cause inflammation and cell damage.
Shiga toxin can also cause red blood cells to die. The dead cells can overwhelm the kidneys and cause a dangerous complication called hemolytic-uremic syndrome . Deadly cases of E. coli colitis are usually due to HUS and are more common in children and the elderly.
Its hard to know how common E. coli hemorrhagic colitis is because many cases never get diagnosed. The Centers for Disease Control and Prevention estimate there are about 73,000 cases every year in the United States.
How Does Blood In The Stools Appear

According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Don’t Miss: What To Do When Ulcerative Colitis Flares
T Cell Isolation And Stimulation
Peripheral venous blood was obtained from healthy volunteers in compliance with the AIIMS Institutional ethics committee protocols. Peripheral blood mononuclear cells were separated by Ficoll-Paque plus gradient centrifugation. The PBMCs were stained with CD4- Allophycocyanin , CD25-phycoerythrin-Cy7 and CD45 RA- Phycoerithrin . Naive T cells were sorted by high speed flow cytometry with FACS AriaIII to > 95% post sort purity. Cells were cultured at 105 cells/well in a 96 well U bottom plate for 6 days in serum free X vivo medium and stimulated with plate bound anti CD3 and soluble anti CD28 . In Th polarization assay, at the start of the culture, cells were differentiated with recombinant IL-2 for Th0, TGF1 , IL-1 , IL-6, IL-21 and IL-23 for Th17 in the presence and absence of potassium chloride.
Who Is At Risk For Ulcerative Colitis
Some things may make you at higher risk for ulcerative colitis. These include your:
- Age. The disease most often starts when you are between the ages of 15 and 30 years old.
- Family history. Having a family member or close blood relative with ulcerative colitis raises your risk of the disease.
- Race and ethnicity. It happens more often in white people and people of Jewish descent.
Recommended Reading: Foods To Avoid With Peptic Ulcer
Living With Uc: Reducing Flares
There are few non-drug, controllable factors that can reduce the symptoms of ulcerative colitis. Stress reduction is important although it probably makes the symptoms seem less severe without actually reducing them. Of course, it is of utmost importance for patients to take their medications regularly and not miss doses. Although smoking can reduce the inflammation of ulcerative colitis, smoking cannot be recommended as treatment because of its many other detrimental effects.