Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
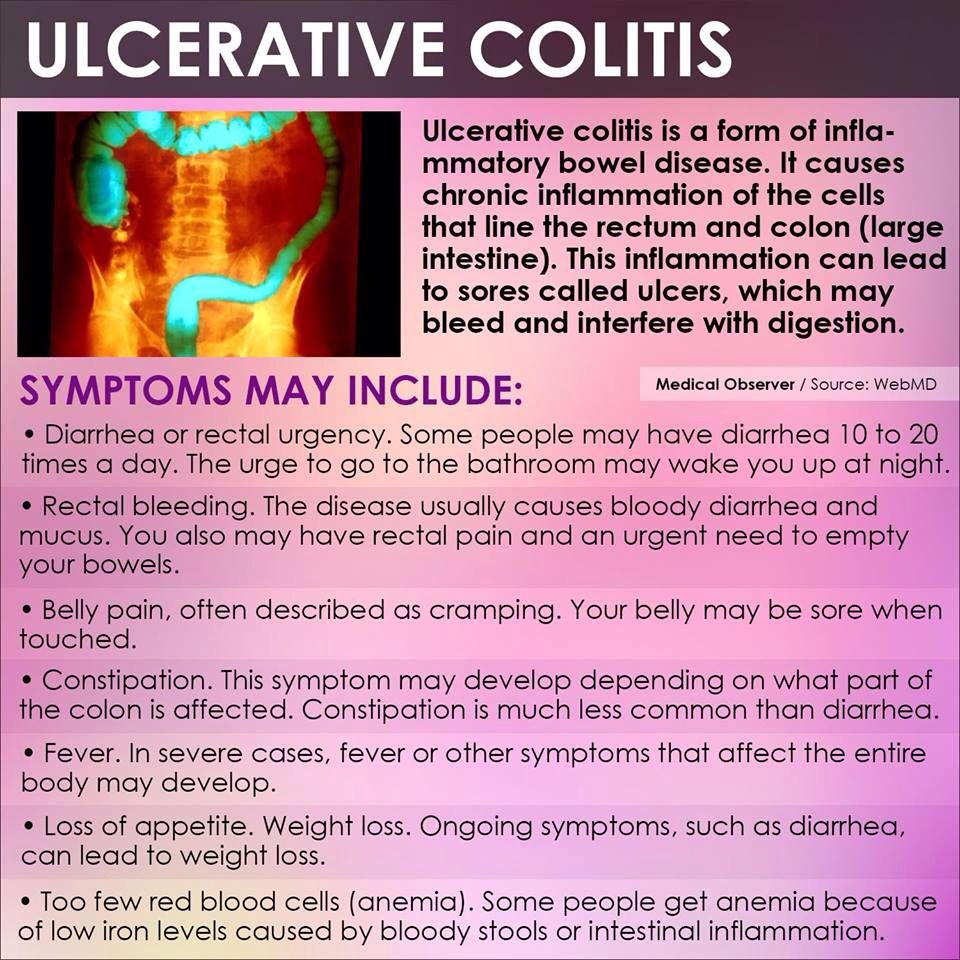
What Symptoms Do Colitis And Ulcerative Colitis Share
Colitis can cause similar belly and bowel issues no matter the cause. Some symptoms are mild while others are more serious.
General signs of colitis and UC include:
- Stomach cramps that come and go
- Constant belly pain
- Mucus or blood in your poop
- Weight loss without trying
- An urgent need to poop
- A feeling like you didnât get all your poop out
If you have periods, you may have:
- Worsening diarrhea during your period
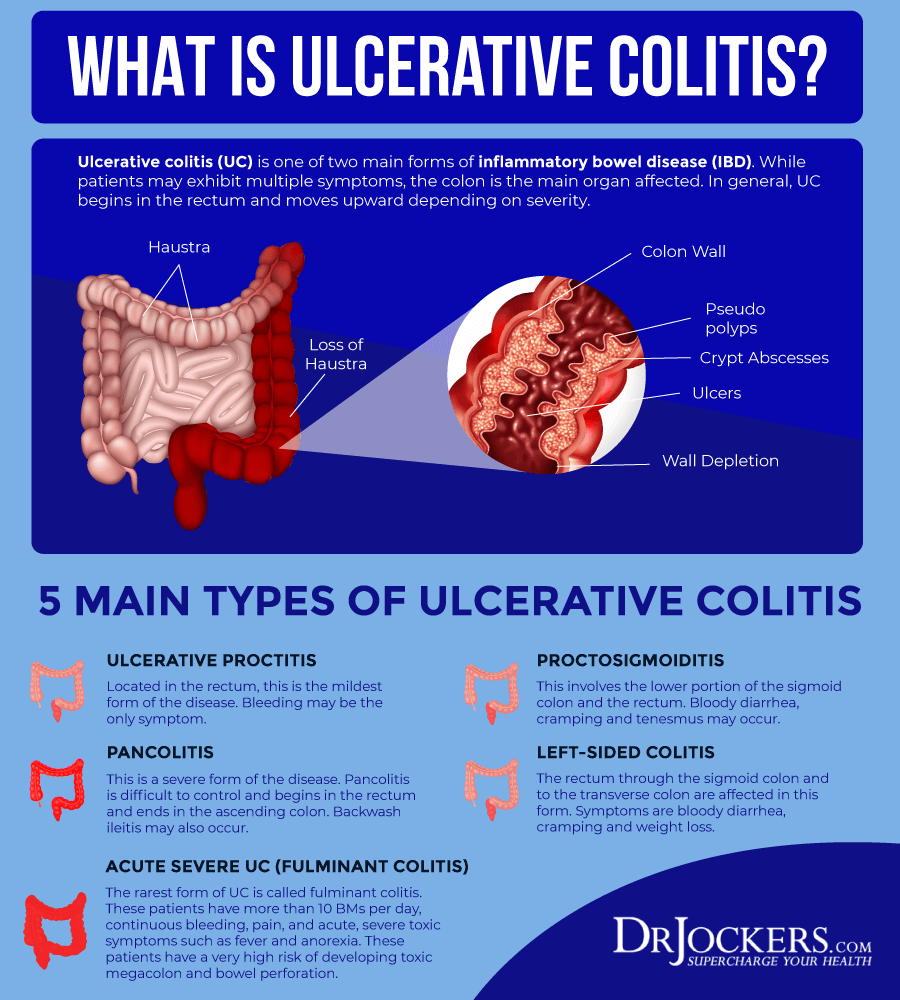
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Read Also: What Not To Eat When You Have Ulcerative Colitis
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Follow Up With Your Doctor

You may only need at-home or short-term care for some kinds of colitis. But UC is a condition youâll have for the rest of your life. And it affects everyone in a different way. Youâll need to work with your doctor to find a treatment plan that works for you.
No matter whatâs causing your symptoms, get medical care right away if you have:
- Watery diarrhea for more than a few days
- Heavy, ongoing diarrhea
Don’t Miss: Psc Liver Disease Ulcerative Colitis
Why Choose Mount Sinai
Mount Sinai has a unique and rich tradition of specialized and individualized treatment and scientific research and discovery in ulcerative colitis. The physicians/scientists in the Mount Sinai Health System are constantly conducting clinical trials and are developing new drug therapies to help patients manage their disease. Learn more about ulcerative colitis.
There are 3 basic tests for colon cancer a stool test , sigmoidoscopy , and colonoscopy . All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Ulcerative colitis is categorized according to location. Proctitis involves only the rectum. Proctosigmoiditis affects the rectum and sigmoid colon. Left-sided colitis encompasses the entire left side of the large intestine. Pancolitis inflames the entire colon.
What Diet Is Best For Ulcerative Colitis
There is no specific diet or meal plan for ulcerative colitis , according to the U.K.s National Health Service . Some people may find that certain foods trigger symptoms or make them worse.
You may find that consuming a diet low in fiber during a UC flare may help ease your symptoms. Foods you can consume as part of a low fiber eating plan include:
Other meal plan tips for UC include:
- eating smaller meals more frequently rather than fewer larger meals
- drinking plenty of fluids
- taking food supplements at your doctors advice
- avoiding caffeine and alcohol, which can make diarrhea worse
- avoiding fizzy drinks, which can cause gas
- keeping a food diary to monitor which foods may be triggering your symptoms
Contact your doctor before making any significant changes to your eating habits. Your doctor may refer you to a dietitian or nutritionist to help make sure you get all of the nutrients you need while managing your symptoms.
Find out more about foods that can affect UC. You can also learn more about meal planning with UC.
Recommended Reading: Garlic Powder And Ulcerative Colitis
When To See A Doctor
For people with ulcerative colitis, it can be challenging to know which symptoms are an emergency, which should prompt a call to the gastroenterologist, and which can wait.
After doing well and having few or no symptoms, when symptoms begin again, it is a reason to call the doctor and get evaluated for a potential flare-up. It may be necessary to change treatments or adjust the current care plan in order to get any inflammation under control quickly.
Ulcerative Colitis Doctor Discussion Guide
Get our printable guide for your next doctor’s appointment to help you ask the right questions.
In general, symptoms such as severe abdominal pain, excessive bleeding, and signs of dehydration are a reason to seek medical care right away. When possible, calling the gastroenterologist before going to the hospital might help in deciding what level of care is needed.
However, if treatment is needed right away, going to the emergency department may be the best choice. If a serious condition such as a bowel perforation or toxic megacolon is suspected, it may be necessary to call 911, because these are medical emergencies.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
You May Like: Sacral Decubitus Ulcer Icd 10
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Rectal Bleeding And Discharge
UC often causes bleeding or mucus discharge from your rectum. You may find spots of blood or mucus in your toilet or on your clothing. Your stool may also become very soft and bloody or contain red streaks or mucus. You may also experience pain in your rectal area, as well as a persistent feeling of needing to have a bowel movement.
Also Check: High Calorie Diet For Ulcerative Colitis
Do Different Types Of Ulcerative Colitis Cause Different Symptoms
Certain symptoms may point to different types of ulcerative colitis. These types, as outlined by the Mayo Clinic, are classified by location within the body:
- Ulcerative proctitis: With this form of the condition, which tends to be the mildest, a person has inflammation in the area closest to the rectum. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis: Inflammation with this form of the disease involves a persons rectum and lower end of the colon. Symptoms can include bloody diarrhea, abdominal pain, and an inability to go despite feeling like you need to let loose.
- Left-sided colitis: This involves inflammation from the rectum, through the lower colon, and into the descending colon. In addition to bloody diarrhea and abdominal pain on the left side, you may also experience weight loss. Most patients will have left-sided disease, Dr. Sinha says.
- Pancolitis: This usually impacts a persons entire colon, causing bloody diarrhea that can be severe, abdominal pain, fatigue, and rapid weight loss.
How Can I Find Support After An Ulcerative Colitis Diagnosis
When taking care of your physical well-being, dont forget that ulcerative colitis can take a toll on your emotional and mental well-being too. If it turns out your symptoms are ulcerative colitis, you can find a support group, or ask your doctor if they can connect you with a therapist or G.I. psychologist. Dr. Riehl, for example, works with patients on aspects of body image and even connects them with other patients who have experienced colectomy or ostomy . We talk openly about the impact that it can have on them from an intimacy perspective to how it impacts their self-identity, she says.
Since ulcerative colitis often starts at an age when people are thinking about their first job or starting a family, it can be particularly tough. One of the reasons that I and several of my colleagues went into this field is precisely because of thatso that we can hopefully make a difference in peoples lives early, and have them be able to lead productive and complete lives by putting their disease in remission, Dr. Sinha says.
You May Like: Ulcerative Colitis Flare Up Treatment Guidelines
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Don’t Miss: Air Mattress For Decubitus Ulcers
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Don’t Miss: How To Calm An Ulcer
What Are The Risk Factors For Ulcerative Colitis
The main risk factor for ulcerative colitis is having a family member with the condition.
While experts do not know the exact cause of UC, they believe that genetics may play a role in its development.
Age may also increase your risk of UC. It most commonly affects people between ages 15 and 30, though it can occur later in life.
Can I Prevent Ulcerative Colitis
Because experts do not know the exact cause of ulcerative colitis , it may not be possible to prevent it.
Yet you may be able to take steps to reduce the severity of symptoms or to prevent relapse. Per the NHS, these include:
- avoiding foods that trigger your symptoms
- drinking plenty of fluids to stay hydrated
- getting enough regular exercise
- taking steps to reduce stress, such as relaxation techniques
Contact your doctor for more advice on ways to reduce the severity of your symptoms or to prevent relapse if you are in remission.
Recommended Reading: Ways To Prevent Pressure Ulcers In Hospitals
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
Doctors arenât sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Itâs most likely if youâre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress donât cause it, but they can trigger a flare of symptoms.
Also Check: How Do You Check For Ulcers
Signs Of Possible Colitis
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.