Even On Good Days Take Your Meds
It can be easy to forget to take your medicines when you feel good. Or you might think itâs OK to skip them because you feel fine. But you need to stick with the plan your doctor prescribed to keep up those benefits.
You and your doctor will work together to decide if you need to stay on medicines to control your UC. The type of medicine will depend on how severe your UC is.
Read Also: Best Ointment For Leg Ulcers
Crohns And Ulcerative Colitis Pose Special Concerns For Women
Karen Nitkin Spring/Summer 2020
About 1.5 million Americans slightly more women than men live with Crohns disease and ulcerative colitis, the chronic gastrointestinal disorders collectively known as inflammatory bowel disease .
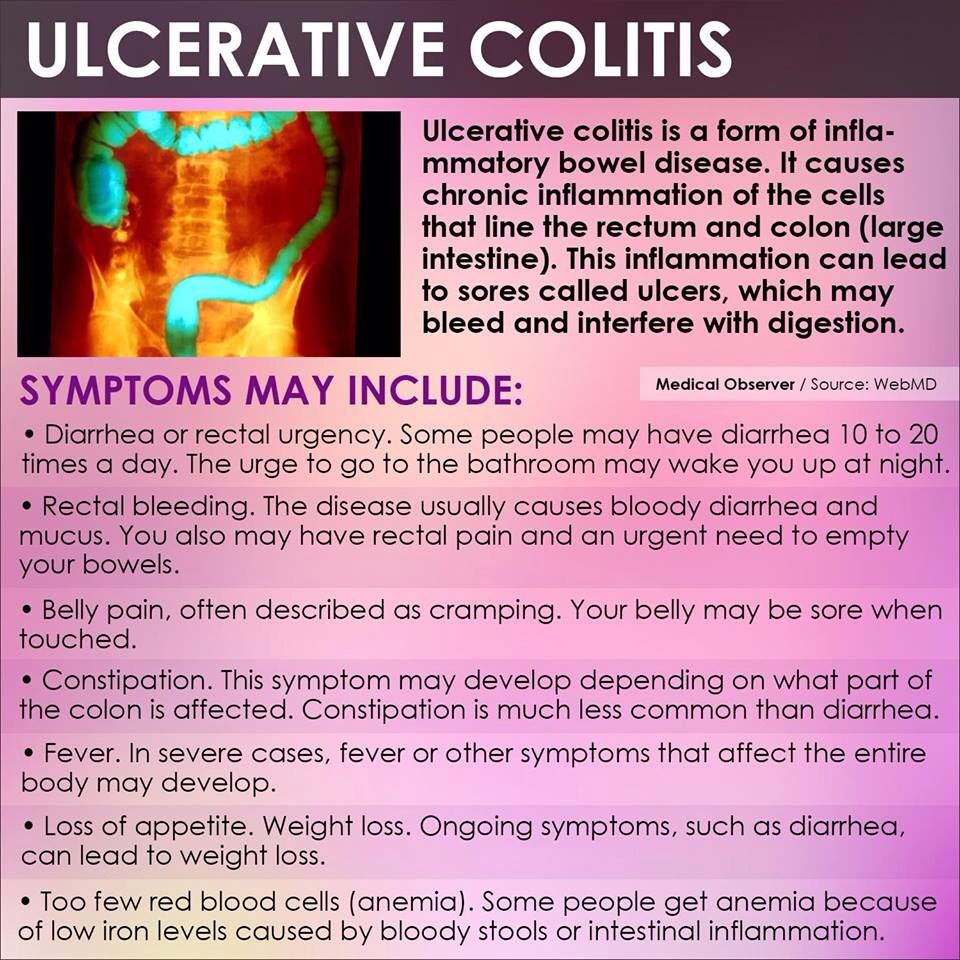
Both men and women with IBD experience painful and potentially damaging inflammation of the digestive tract. IBD has no cure treatments focus on controlling and preventing future flare-ups with medications and treating symptoms such as abdominal pain, fever or diarrhea.
Yet IBD affects women in unique ways, says Aline Charabaty, clinical director of gastroenterology and director of the Inflammatory Bowel Disease Center at Sibley Memorial Hospital. It can interfere with menstruation and childbirth and intensify anemia and osteoporosis, she notes.
Crohns disease and ulcerative colitis are not exactly the same. Crohns disease is characterized by inflammation in any part of the gastrointestinal tract, with symptoms that can include abdominal cramps, diarrhea, delayed growth, weight loss, fever and anemia. Ulcerative colitis affects the inner lining of the large intestine and rectum, with symptoms that often include bloody diarrhea, frequent bowel movements, abdominal and rectal pain, fever, weight loss, joint pain and rashes.
Here are four ways IBD poses particular concerns for women:
Alarm Symptoms Of Ulcerative Colitis:
If you are already diagnosed with ulcerative colitis, there are several alarm symptoms to look out for. A change in your ulcerative colitis symptoms may mean that additional treatment is needed. Talk to your doctor immediately if you experience a new symptom, a change in your current symptoms or any of the following:
- An unusual amount of cankers or sores in your mouth
- Unexplained or unintentional weight loss
- Failure to gain weight
- Delayed puberty in teens
- Anemia this blood condition results in fatigue and weakness. It is usually caused by heavy blood loss or a lack of dietary iron
- Rectal bleeding
You May Like: What Is Acute Ulcerative Colitis
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
Doctors arenât sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Itâs most likely if youâre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress donât cause it, but they can trigger a flare of symptoms.
Dont Miss: Is Omeprazole Good For Ulcers
What To Do During A Flare
Most skin issues associated with UC are best treated by managing the UC as much as possible, as many of these rashes can coincide with UC flare-ups. Others may be the first sign of UC in someone who hasnt been diagnosed yet.
Corticosteroids can help with the inflammation that often causes the skin issues associated with UC. Eating a well-balanced diet can help promote overall health and may aid in preventing skin issues.
When you do experience a flare-up of UC skin rash, there are several things you can try:
- Keep the lesion clean to prevent infections.
- See your doctor for prescription antibiotic ointment or pain medication if needed.
Also Check: Is Ulcerative Colitis A Disability
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Also Check: How To Get Rid Of Stomach Ulcer Pain
What Is The Hospital Treatment For Ulcerative Colitis
When you’re admitted to the hospital for ulcerative colitis, you may have to stay for many days. You’ll likely be hooked up to receive intravenous fluids via an IV in order to rehydrate your body and give you medications.
There are four main reasons why your medical team would want to keep you under observation:
Don’t Miss: How Fast Does Humira Work For Ulcerative Colitis
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Work With Your Doctor
Youll need to see your UC doctor regularly. It may be every 6 months while youre in remission. Youll have routine procedures like colonoscopies and bloodwork to check on your UC.
If youre having a flare-up, make sure to check in with your doctor. UC isnt the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Cant keep liquids down
When you have a flare, you can ask your doctor questions like these:
- Is UC causing my symptoms, or could they be due to another condition?
- Do I need to take any tests? If so, how often will I need to get them?
- Will you need to change the dose or type of my medication?
- If I need to take a new medication, what side effects could it cause?
- Should I make any lifestyle changes?
- When should I come back for another appointment?
You May Like: What Foods To Eat When You Have An Ulcer
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Living with Colitis
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
You May Like: How To Get Rid Of Tongue Ulcers
Managing Fevers With Ibd
Whatever the case, if you have IBD, always keep an accurate thermometer in your home. Take your temperature, and if it is 102.92 degrees Fahrenheit or higher, let your doctor know. While you have a fever, there are some home remedies you can use to reduce your symptoms and help your body recover:
- Drink plenty of fluids.
- Avoid covering yourself with heavy pajamas or blankets, which can raise your temperature further.
- Ask your doctor about taking medication like Tylenol.
- Avoid dehydrating foods, especially those with salt, and choose snacks like fresh fruit.
Will Ulcerative Colitis Ever Be Cured

Researchers are looking at other treatment options and potential cures for UC.
Two of the newest UC medications developed in the last couple of years include biosimilar medications and Janus kinase inhibitors.
Biosimilar medications contain copies of the antibodies used in a common type of UC medication referred to as biologics. Those antibodies help the body stop production of some proteins that can cause inflammation.
Severe cases of UC can be treated with a JAK inhibitor called tofacitinib . It helps block certain enzymes that can trigger inflammation.
Research is ongoing as to whether other therapeutics, such as stem cell therapy and stool transplant, can treat or cure UC.
It is my firm belief that there will be major improvements to UC management within the next decade.
You May Like: Best Oil For Horses With Ulcers
Symptoms Of Inflammatory Bowel Disease
Symptoms of inflammatory bowel disease may range from mild to severe, with periods of active illness followed by periods of remission. Common signs of both Crohns disease and ulcerative colitis include:
- Diarrhea: Loose stools are one of one of the most common symptoms of IBD.
- Fever and fatigue: Many people with IBD experience a low-grade fever. You may also feel tired or have low energy.
- Abdominal pain and cramping: Inflammation and ulceration can affect the normal movement of contents through your digestive tract and may lead to pain and cramping. You may also experience nausea and vomiting.
- Blood in your stool: You might notice bright red blood in the toilet bowl or darker blood mixed with your stool. You can also have bleeding you dont see .
- Reduced appetite: Abdominal pain and cramping, as well as inflammation, can affect your appetite.
- Unintended weight loss: You may lose weight and even become malnourished because you cannot properly digest and absorb food.
I Take Medication Regularly Can A Flare
Unfortunately, yes. Ulcerative colitis is a chronic condition. Medications and lifestyle changes can help reduce the intensity and frequency of ulcerative colitis flare-ups, but not stop them completely.
Regular flare-ups may indicate a problem with your current treatment. If you are taking your medications as prescribed and still experiencing flare-ups, you should contact your physician who may adjust your medication or suggest other treatment options.
You May Like: Over The Counter Ulcer Treatment For Horses
When To Call Your Doctor
If youre having any of the above UC symptoms, especially bloody stool, endless diarrhea, or severe pain, make an appointment with your primary-care doctor. It could always be something other than UC, but its important to get it checked out.
The sooner you treat UC and work to stop the damage to your intestinal lining and overall health, the better. If your GP suspects UC, they will likely refer you to a gastroenterologist, which is a type of physician specializing in digestive health care. This doc can further evaluate your symptoms, run any necessary tests, and get you a diagnosis.
If youve already been diagnosed with UC, call your gastro if youre experiencing any increase in symptoms like bloody stools, diarrhea, and pain, along with weight loss, fatigue, and fever.
And we totally get it. Talking about UC symptoms with your doctoror anyone!can feel awkward or embarrassing . But its hugely important that youre honest about whats going on so your doctor can get you the best treatment possible.
Important Information About All Medicines
|
Never take more than the prescribed dose. If you suspect that you or someone else might have taken an overdose of this medicine, go to the accident and emergency department of your local hospital. Take the container with you, even if it is empty. If you are having an operation or dental treatment, tell the person carrying out the treatment which medicines you are taking. If you buy any medicines, check with a pharmacist that they are suitable to take with your other medicines. This medicine is for you. Never give it to other people even if their condition appears to be the same as yours. Do not keep out-of-date or unwanted medicines. Take them to your local pharmacy which will dispose of them for you. If you have any questions about this medicine ask your pharmacist. |
You May Like: What Happens When You Have A Stomach Ulcer
You May Like: Can Ulcerative Colitis Cause Low Testosterone
What Other Conditions Can Cause Fever And Night Sweats
Fever is a symptom of many conditions, including infections, malignancies, and autoimmune disorders.7 The cause of most fevers can be readily diagnosed and treated. Often, fevers get better on their own.7
Night sweats are also non-specific. People report night sweats related to cancer, infection, and hormone changes.8 They can be related to some medications, changes in blood sugar levels, pregnancy, and some mental health problems.
When To Call Your Doctor About A Flare
Flares come with different levels of intensity. You may be able to manage a mild flare-up of symptoms on your own. But a more severe flare may be a warning sign of an ulcerative colitis complication that needs immediate attention.
Theodore J. Saclarides, MD, a colon and rectal surgeon at Rush University Medical Group in Chicago, suggests calling your doctor if you have any of these ulcerative colitis symptoms:
- Severe abdominal pain that lasts more than 24 hours
- A decrease in bowel movements along with abdominal pain
- Abdominal pain with a high fever
- Blood during a bowel movement that is too thick to see through
Editorâs Picks
Read Also: I Have Ulcerative Colitis Can I Get Disability
Lifestyle Changes To Treat Ulcerative Colitis
You can make dietary and lifestyle changes to help alleviate symptoms and lengthen time between flare-ups.
While there is no evidence that says certain foods cause ulcerative colitis, there are certain foods that can aggravate your symptoms. Limiting dairy products and avoiding problem foods may help improve your symptoms. Problems foods can vary for each person, but you should also avoid gassy foods such as beans, cabbage and broccoli, raw fruits and fruits, popcorn, caffeine and carbonated beverages. Experiment with fiber. For some, adding more high-fiber foods can help with bowel issues however, if you have an inflammatory bowel disease fiber may worsen your symptoms. Try eating five or six meals instead of two or three large ones and drink plenty of fluids, preferably water.
Avoiding stress is also a good way to alleviate your symptoms. Stress can aggravate your symptoms, so learning to better manage stress can help. Exercise, biofeedback, regular relaxation and breathing exercises are all ways you can manage stress.
Causes Of Ulcerative Colitis Flares
Ulcerative colitis flares can be caused by a variety of things, including:
- Skipping medications or not taking the correct dose. If you regularly take medicine for your ulcerative colitis, you need to be consistent even when your disease is in remission. If you dont follow prescription instructions, flares can occur.
- Taking non-steroidal anti-inflammatory drugs. Common drugs like aspirin, naproxen, and ibuprofen can inflame the bowel and bring on serious symptoms. If you need mild pain relief or fever treatment, you should take acetaminophen.
- Taking antibiotics. Although theyre useful when you have bacterial infections, they affect the bacteria that live in your intestine. These changes can result in diarrhea or the growth of too much of a certain bacteria that then causes inflammation. If you have a bacterial infection, make sure your healthcare provider knows you have ulcerative colitis.
- Not managing stress. Physical and emotional stress can bring on flare-ups. Once you understand that stress causes such a reaction, you can find out what stress management strategies work to keep flare-ups at bay.
- Eating and drinking triggering items. The foods and drinks that bring on symptoms vary by person. Youll need to track your diet so you can pinpoint triggering items when you experience ulcerative colitis flares.
Dont Miss: What Medicine Is Good For Ulcers
Read Also: How Do You Know If You Have Bleeding Stomach Ulcer