What Is Ulcerative Colitis
Ulcerative colitis is often limited to the rectum and lower colon but can involve the entire colon.
Ulcerative Colitis is the result of an abnormal response by your bodys immune system, in which the cells and proteins that normally make up the immune system to protect you from infection, mistake food, bacteria, and other materials in the intestine as foreign or invading substances. When this happens, the body sends white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcerations.It is important to understand the difference between Ulcerative Colitis and Crohns Disease.
Crohns Disease can affect any part of the Gastrointestinal Tract, but Ulcerative Colitis affects only the colon. Additionally, while Crohns Disease can affect all layers of the bowel wall, Ulcerative Colitis only affects the lining of the colon. Although both Ulcerative Colitis and Crohns Disease are types of Inflammatory Bowel Diseases , they should not be confused with Irritable Bowel Syndrome , since that is a disorder which affects the muscle contractions of the colon and is not characterized by intestinal inflammation.
Can I Treat Ibd If I Am Pregnant Or Breastfeeding
Yes, but your doctor may change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31
Before you get pregnant, make a plan with your obstetrician and gastroenterologist about the medicines you will take during and after pregnancy. Take your medicines as your doctor tells you to. If you stop taking your medicines and your symptoms come back , it may be difficult to get them back under control.31
Talk with your doctor about your medicines and breastfeeding before you give birth. You can search for your medicine in the LactMed database to find out if your medicine passes through your breastmilk and, if so, if it has any possible side effects for your nursing baby.
Also Check: How Do You Stop A Stomach Ulcer From Hurting
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Don’t Miss: How To Cure Peptic Ulcer Disease
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Also Check: Stelara Dosing For Ulcerative Colitis
You May Have An Increased Risk Of Miscarriage And Other Pregnancy Complications
Bonthala notices that many of her patients who are pregnant or trying to conceive are wary of taking medications to treat their ulcerative colitis, citing concerns about how the treatment may affect their baby.
Its important to put out there that the vast majority of medications are safe for pregnancy and for breastfeeding with only a few exceptions, she says. A bigger risk to pregnancy? Untreated IBD.
In fact, a September 2020 review published in the journal Digestion found that active IBD is associated with an increased risk of miscarriage, stillbirth, preterm delivery, low birth weight, and other pregnancy complications. The researchers found that women who have inactive disease before conceiving have pregnancy outcomes that are similar to women without IBD.
If youre trying to get pregnant, Bonthala recommends getting your ulcerative colitis under control first. If youre already pregnant and are having a flare, seek treatment as soon as possible.
Also Check: Succeed For Horses With Ulcers
Treating Ibd And Anxiety
The study authors say it is important for physicians to determine whether patients with IBD also have a functional disorder. Differentiating symptoms between the two can be difficult, so they suggest that doctors first look for signs of inflammation, treat those, and then if symptoms remain it could indicate a functional disorder, at which point they should consider treatment for this disorder as well.
Physicians typically involved in caring for IBD patients, such as general practitioners and gastroenterologists, sometimes dont have much formal training in psychological disorders, and since patients are often hesitant to bring up psychological symptoms due to social stigma, they typically remain undiagnosed and untreated for too long. When IBD patients with an anxiety disorder experience stigma and therefore dont seek treatment, it can lead to further disability. It is very important that physicians are aware of the increased risk of anxiety in IBD patients, and should be prompt in detecting and treating any coexisting anxiety disorders. Patients also have a responsibility to speak up and ask for help if they perceive that anxiety is a problem for them.
If you are an IBD patient and are concerned that you might have anxiety or a functional gastrointestinal disorder, speak with your doctor.
First published in the Inside Tract® newsletter issue 195 2015
Email News Sign Up
Eating During Remission From Uc
During remissionthat blissful time when your insides arent rioting against youyou may wonder if you can relax a little bit more about the foods you eat. In general, move slowly when adding new foods to your diet during remission. In fact, its best to do it one at a time so you can monitor any reaction. Otherwise, aim to hit the main points of a Mediterranean diet to get the nutrients you need. Your doctor or R.D. can offer more advice too. In the meantime:
-
Prioritize whole grains, non-cruciferous vegetables and low-fiber fruits, and healthy fats
-
Incorporate poultry, fish, beans, and eggs weekly
-
Add moderate portions of dairy if you can tolerate lactose
-
Limit your consumption of red meat
-
Limit processed foods
Also Check: What Kind Of Yogurt Is Good For Stomach Ulcer
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Is There Any Diet That Helps Ibd
Yes, an all-liquid diet of nutrients, called an elemental diet, has been shown to reduce inflammation in the intestines. However, most people cannot tolerate it because it is given overnight through a tube that runs through the nose to the stomach. There are other diets that reduce the amount of different types of sugars that cause bacteria to create gas in the intestine, which can lead to a lot of symptoms of pain, bloating, and cramping. The best proven diet is the FODMAP diet.
Dont Miss: Treating Leg Ulcers With Sugar
Don’t Miss: Drugs To Treat Ulcerative Colitis
Eating During A Flare
During a UC flare, you may need to eliminate certain foods from your diet. Working with a doctor or dietitian to adjust your diet can help you avoid nutrient deficiency.
Start by cutting out foods you know trigger your symptoms. These can vary from person to person.
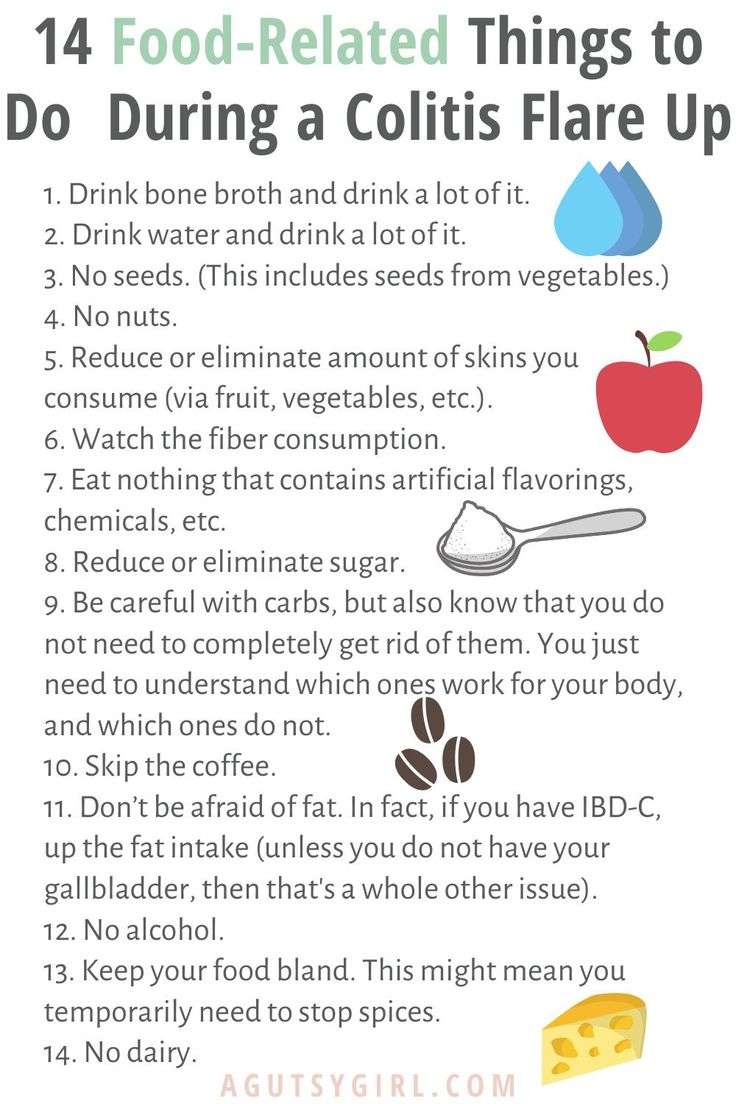
According to the , common trigger foods for UC include:
- whole nuts or whole grains
- fruits with skin and seeds
- raw cruciferous vegetables
- alcohol
- spicy foods
You may also find it helpful to steer clear of greasy or fried foods, which can worsen symptoms, per the .
Throughout a flare, its also important to make sure youre still getting the right amount of nutrients.
Inflammation, diarrhea, vomiting, and other symptoms can make it difficult for your body to absorb nutrients, potentially leading to deficiencies.
Focusing on nutrient-rich foods that dont tend to worsen UC symptoms may help you get the recommended amounts of vitamins and nutrients.
Here are some foods that may be easier to tolerate during a UC flare:
- low fiber fruits
- cooked vegetables without seeds or skins
- homemade protein shakes
Its also important to stay hydrated during a UC flare. Keeping a full water bottle by your side may help you remember to drink enough.
You may also want to use a straw and sip slowly. This helps prevent swallowing air, which can contribute to increased gas.
What About Vitamins And Minerals
It is a good idea for all people with IBD to take a standard multivitamin every day. People with IBD who are doing well do not need any extra vitamins or minerals. If you have Crohns disease is in the ileum or the ileum has been removed you may need to take B12, calcium, or vitamin D. You may need iron supplements if you have blood loss during inflammation or reduced iron absorption as a result of inflammation. Diarrhea or vomiting can cause loss of potassium and magnesium. If you are lactose intolerant and avoid dairy products, this can lead to low calcium. Ask your doctor if you need to be tested for any of the above.
Recommended Reading: How To Heal Ulcerative Colitis With Food
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Breathe And Be In The Moment
We learned a few breathing techniques while at Nutrition School, but try breathing in for a few counts, hold for a few and then release for a few. Repeat several times. Allow yourself to just be in the moment vs. thinking backward or forward. This applies to meal times, in particular. Sit, be and eat your food in the moment, slowly. Want more on breathing? Check out: Breathe Deep.
p.s. Once your flare ends, get yourself on the gut-healing fast track.
Our bodies are not just made up of food. We are whole human beings, and our circumstances at any given moment might have more to do with our current well-being state when the food arrives in us vs. the actual food itself.
I have gotten a lot of help, and I have worked really hard on healing. When it comes to food, I am reaping the benefits , feeling incredible and remaining flare-free.
My wish is for you to find the same, and in the meantime, my wish is that these tips will help you get over your next flare quickly.
If you liked this post, you might also enjoy:
Recommended Reading: Can Ulcerative Colitis Make You Vomit
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Fruit Or Vegetable Juices
After a flare of Crohnâs disease or ulcerative colitis, you may not feel like eating much. But you need calories and nutrients, so start your diet again slowly. Fruit or vegetable juices are great when you donât have much of an appetite. They give you vitamins plus hydration without weighing you down. Just choose one without pulp — the fiber could cause cramping or bloating. You may want to water down your juice if itâs high in sugar, since too much of the sweet stuff could trigger diarrhea.
Also Check: Ulcerative Colitis Treatment In India
How Does The Diet Work
Breaking the Vicious Cycle states that a person can begin step 1: the introductory period where they can only eat certain very simple foods. This period typically lasts 12 days.
This stage is crucial to clear harmful microbes by starving them and feeding the body with easy-to-digest, nutritious foods.
It is important to maintain close contact with a healthcare professional at the start of the diet. A doctor will check a persons weight to assess if they have gained or lost any weight and perform a complete blood count.
Anti-inflammatory foods may include:
- mashed fruits and vegetables
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Read Also: In Order To Prevent Pressure Ulcers
The Role Of Peripheral Substance P
In addition to its central effects, peripheral release of SP from the ENS may have a role in stress induced increases in mucosal inflammation. Although there are no published data to show an increase in mucosal SP in response to stress, SP containing neurones are found in close association with mast cells, a cell type implicated as central in mediating stress induced permeability changes . SP has been shown to increase histamine release from mucosal mast cells in patients with IBD. Lastly, SP can act not only as a neurotransmitter but also an inflammatory cytokine in its own right, enhancing cytokine production and stimulating chemotaxis of inflammatory cells. It also increases expression of leucocyte adhesion molecules on microvascular endothelium, and of CD11b on neutrophils, facilitating leucocyte adhesion at sites of inflammation.
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohn’s disease.
Recommended Reading: What Happens When You Have A Bleeding Ulcer
You May Have An Increased Risk Of Osteoporosis
The reason undertreated and untreated ulcerative colitis can lead to osteoporosis is twofold, according to Bonthala. One is that active inflammation steals from the bones. Patients are in the bone-building phase of their life until their mid-30s, so if you have active inflammation, youre depleting nutrients from your bones, and youre not absorbing a lot of the nutrients your bones need, she explains.
The second reason: Flares that arise from poorly managed ulcerative colitis are often treated with steroids, which themselves can lead to osteoporosis. I get a lot of referrals for bone density tests in ulcerative colitis patients in their early 20s, she says.
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Also Check: What Pain Reliever Is Safe For Stomach Ulcer