Optimal Asuc Care Is Multidisciplinary In Nature
ASUC management requires early liaison with other medical specialities from the start of the admission with the multidisciplinary team consisting of a gastroenterologist specialised in IBD, an abdominal surgeon, a radiologist, the IBD nurse and a nutritionist.
Discussing the timing and advantages of surgery early on with the patient is important and requires not only the colorectal surgeon but an early intervention of the stoma nurse. Despite offering the prospect of a restored bowel function, IPAA in itself has a significant impact on functionality and quality of life. Frequently occurring complications such as leakage, sexual dysfunction, soiling and the occurrence of inflammatory disorders of the pouch in up to 50% of IPAA patients should be discussed upfront. Importantly, ileal pouch-anal anastomosis has profound effects on female fertility in a population often within the child-bearing age, although laparoscopic approaches tend to have less severe effects, presumably due to less intra-abdominal adhesions.54,55
Future Directions And Controversies
The number of drugs modulating different disease pathways is expected to expand in the near future. There are at least 27 new drugs for ulcerative colitis with either recently completed or active trials. One example is the oral pan-janus kinase inhibitor tofacitinib, which has shown higher rates of clinical remission than placebo in phase 2 studies. Etrolizumab, a subcutaneous monoclonal antibody that blocks the 7 subunit of the heterodimeric integrins 47 and E7 achieved higher clinical remission rates than placebo in a phase 2 trial. An oral anti-4 integrin therapy significantly increased clinical remission and endoscopic healing in a phase 2 trial. An oral drug inhibiting sphingosine-1-phosphate receptors that blocks lymphocyte egress from lymph nodes has also shown efficacy. In a small trial of 5-ASA non-responders, curcumin increased endoscopic remission in mild to moderate ulcerative colitis as an add-on therapy. Biosimilar biological drugs should decrease the cost of therapy. Results from initial studies with an infliximab biosimilar, CT-P13, have shown efficacy at inducing endoscopic healing in ulcerative colitis. However, immunogenicity and efficacy remains a concern particularly in patients switching from the originator to the biosimilar.
Can Ulcerative Colitis Be Cured
- Ulcerative colitis is not a fatal illness, but it is a lifelong illness.
- Most people with ulcerative colitis continue to lead normal, useful, and productive lives, even though they may need to take medications every day, and occasionally need to be hospitalized.
- Maintenance medication has been shown to decrease flare-ups of ulcerative colitis.
- Surgery may be required in some patients, but it is not required in every patient with ulcerative colitis.
- Routine cancer screening is a must for those who do not undergo surgical removal of the colon.
Learning about ulcerative colitis is the key to living a long and healthy life. Patient and family education will allow a better understanding of the disease and what steps may be taken to control it. Under a doctor’s direction, medications, lifestyle and diet modification may be able to lengthen the time between symptom relapse.
You May Like: Will Ulcer Cause Back Pain
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
What Is Diverticular Disease
- Diverticulosis is a condition that describes small pouches in the wall of the digestive tract that occurs when the inner layer of the digestive tract bulges through weak spots in the outer layer. When these diverticula become inflamed, that is called diverticulitis.
- One of the main causes of diverticulosis is a diet low in fiber.
- Many people with diverticulosis have no symptoms. When symptoms do occur they can include:
- Pain in the abdomen
Recommended Reading: Herbal Medicine For Ulcerative Colitis
What Is The Difference Between Diverticulitis And Ulcerative Colitis
Diverticulosis is a condition that describes small pouches in the wall of the digestive tract that occurs when the inner layer of the digestive tract bulges through weak spots in the outer layer. When these diverticula become inflamed or infected, diverticulitis can develop.
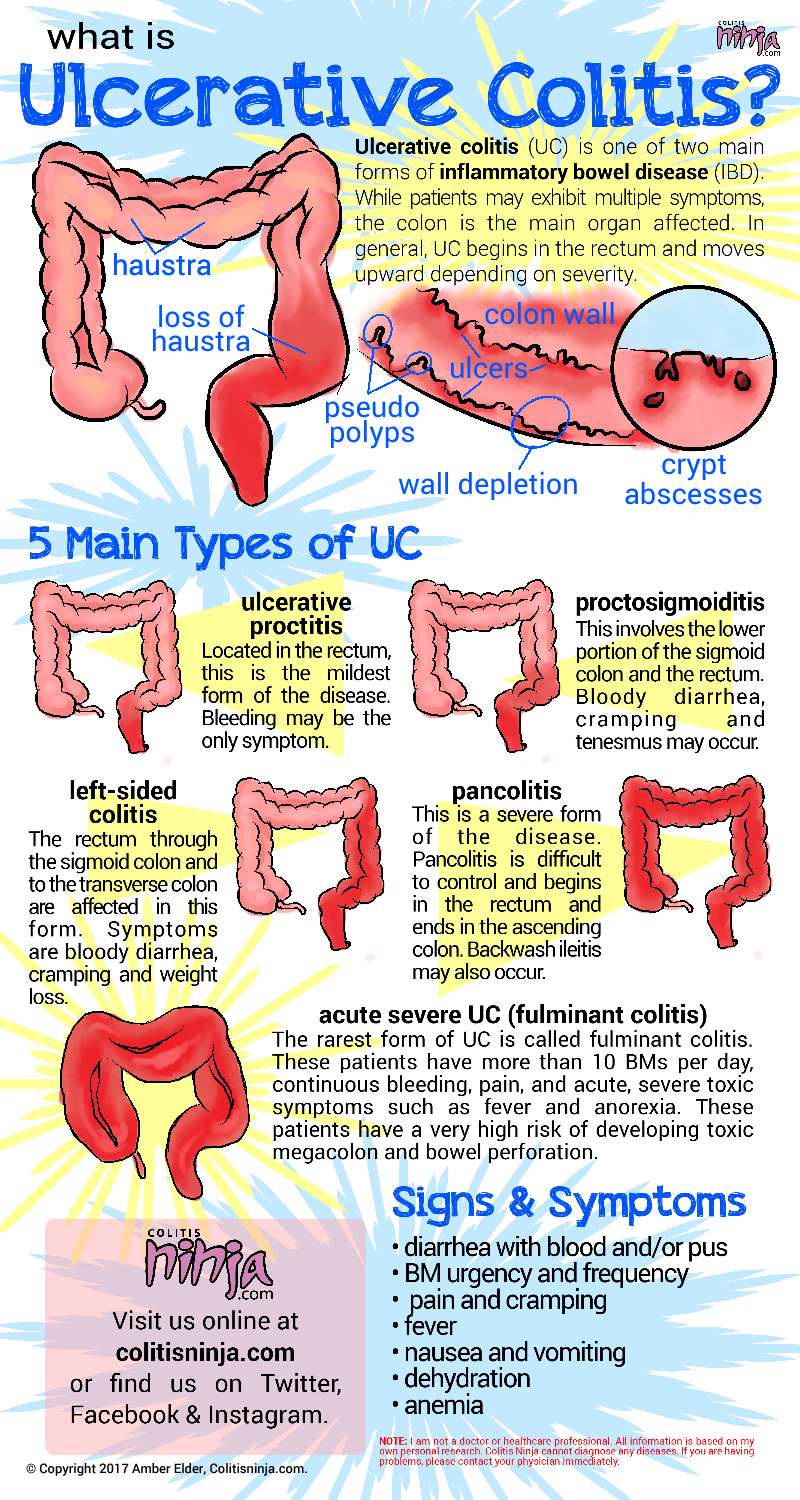
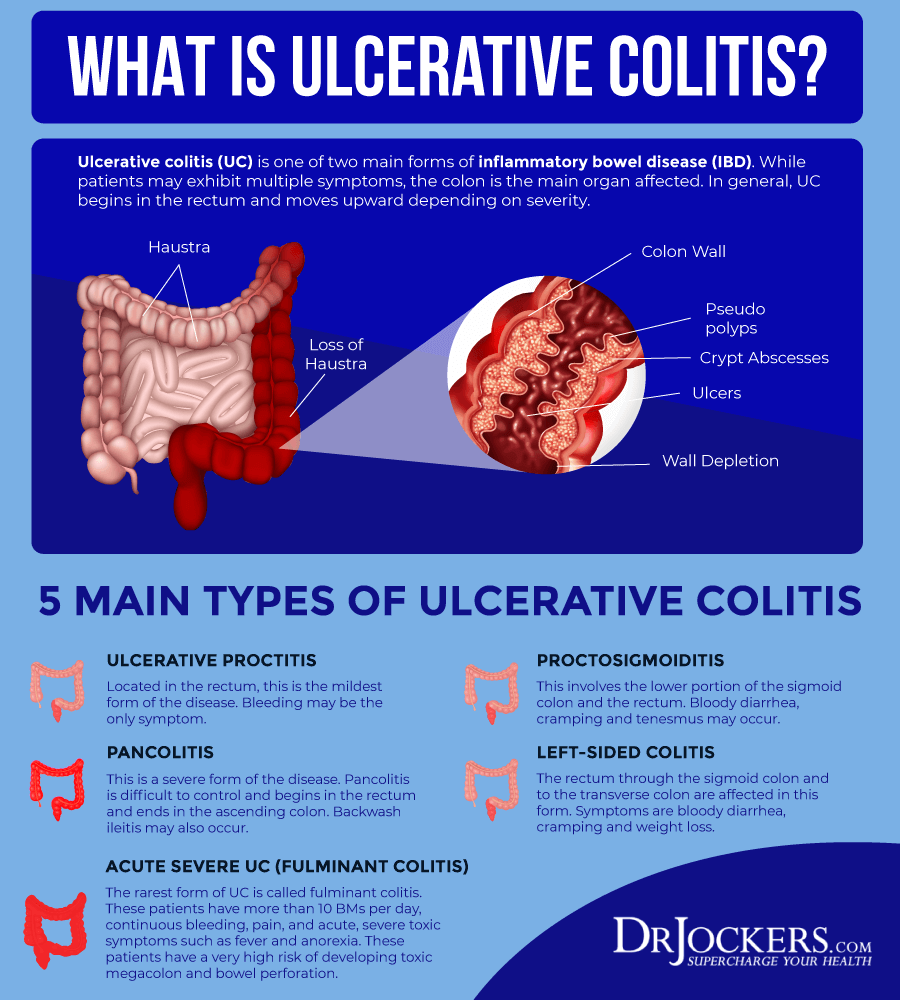
Ulcerative colitis is an acute or chronic inflammation of the membrane that lines the colon . The inflammation occurs in the innermost layer of the colon and may result in the formation of sores . Ulcerative colitis rarely affects the small intestine except for the lowermost section, called the terminal ileum. Ulcerative colitis is a type of inflammatory bowel disease .
What Are The Symptoms And Signs Of Ulcerative Colitis
- Liver and bile duct disease
- Kidney problems
Tell a healthcare professional about any persistent changes in bowel habits. If the patient is already under treatment for inflammatory bowel disease or irritable bowel syndrome, contact a doctor if the patient experiences any prolonged changes in the symptoms or passes blood in the stools.
When Should You Call 911 or Go to the Emergency Department?
Seek medical care if any of these conditions are associated with colitis.
- Blood or mucus in your stool
- Diarrhea that lasts more than three days.
Also Check: How Long Does An Ulcerative Colitis Flare Up Last
What Imaging Tests And Procedures Diagnose Colitis
Colonoscopy: The length of the colon can be directly viewed by colonoscopy. A gastroenterologist uses a thin, flexible tube equipped with a fiberoptic camera to view the inside lining of the colon. The appearance of the colonic lining often allows the doctor to make the diagnosis and also provides the opportunity to look for tumors and polyps. Biopsies can be obtained from the mucosal lining during colonoscopy and evaluated under the microscope by a pathologist to determine the cause of colitis. A biopsy is the only way to diagnose microscopic colitis.
Computerized tomography and barium enema are tests that are sometimes ordered to help diagnose the potential cause of colitis. CT scan of the abdomen has become a more common test to evaluate patients with abdominal pain. However, it is important for the health care professional to balance the risk of radiation with the reward of the information that can be obtained. These tests usually are performed by a radiologist.
Investigations Required At Admission
In addition to monitoring patients clinical feature and vital signs, all patients should have their full blood counts, liver and kidney function tests, electrolytes including serum magnesium and inflammatory markers . At least 3 stool samples for Clostridium difficile toxin should be obtained to rule out superimposed pseudo-membranous colitis. A plain abdominal X-ray should be done to exclude megacolon. Plain radiograph can also provide information about the extent of disease and can also predict response to treatment. The distal distribution of fecal residue can provide a rough estimate of disease extent as it correlates with the proximal extent of disease. The predictors of poor response to treatment on a plain abdominal radiograph are presence of mucosal islands which are small, circular opacities that represent residual mucosa isolated by surrounding ulceration, or presence of more than two gas-filled loops of small bowel. Flexible unprepared sigmoidoscopy with minimal air insufflation should be performed to confirm the diagnosis and exclude superimposed infection, especially cytomegalovirus colitis. Endoscopic markers of severe disease activity include hemorrhagic mucosa with deep ulceration, mucosal detachment on the edge of these ulcerations, and well like ulcerations.
Also Check: What Should You Eat When You Have Ulcerative Colitis
What Is Colon Cancer
Cancer is the transformation of normal cells. These transformed cells grow and multiply abnormally. Cancers are dangerous because of their uncontrolled growth and potential for spread. Cancer overwhelms healthy cells, tissues, and organs by taking their oxygen, nutrients, and space.
In colon cancer, these abnormal cells grow and eventually spread through the colon wall to involve the adjacent lymph nodes and organs. Ultimately, they spread to distant organs such as the liver, lungs, brain, and bones.
Most colon cancers are adenocarcinoma tumors that develop from the glands lining the colon’s inner wall. These cancers, or malignant tumors, sometimes are referred to as colorectal cancer, reflecting the fact that the rectum, the end portion of the colon, also can be affected. Anatomic differences in the rectum as compared to the rest of the colon require that doctors separately recognize these areas.
When To See A Doctor
Bleeding from the rectum or blood in or on the stool is never normal. It should always be brought up to a doctor. However, its not always an urgent situation.
If the cause of the bleeding is from a chronic condition , it should be discussed with your gastroenterologist.
In the case of new bleeding, see a doctor as soon as possible. Rectal bleeding that wont stop is a reason to go to the emergency department. Additionally, if you feel faint from blood loss, get to the emergency department right away or call an ambulance.
Abdominal pain can come and go with ongoing conditions, like Crohns disease or ulcerative colitis. Its important to discuss pain at doctors visits. However, if abdominal pain comes on suddenly and is severe, you should go to the emergency room or see a doctor right away.
In infants, caregivers will want to take the baby to see a pediatrician as soon as possible after seeing blood in the stool or around the rectum. Allergic colitis may be a common reason for bleeding, but its important to have a doctor check it out to make sure theres not a more serious reason.
Also Check: Foods To Eat To Help Ulcers
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Common Symptoms Of Ulcerative Colitis
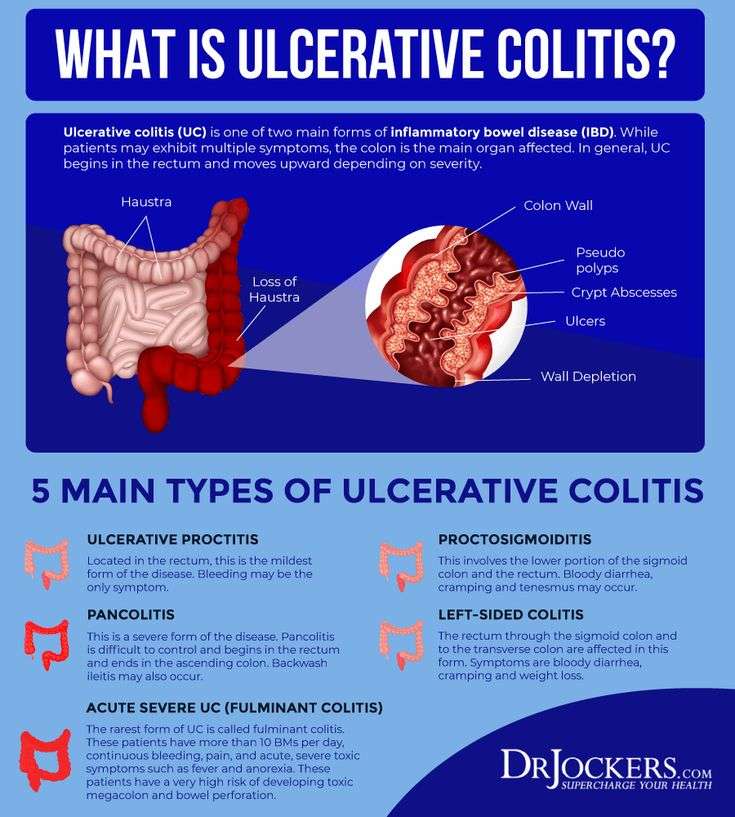
While UC symptoms can vary over time and from person to person, the most common symptoms are diarrhea with blood and abdominal discomfort.
However, your symptoms may vary depending on where inflammation occurs in your GI tract and how severe it is.
Other signs and symptoms include:
- An urgent need to have a bowel movement
- Feeling tired
- Nausea or loss of appetite
- Weight loss
- Fever
- Anemiaa condition in which the body has fewer red blood cells than normal
Also Check: What Foods Should Be Avoided With Stomach Ulcers
What Are The Signs And Symptoms Of Diverticular Disease Vs Ulcerative Colitis
Symptoms and Signs of Diverticulosis
- Pain in the belly
- Bloating
- Constipation
- Cramping
These symptoms are nonspecific. This means that similar symptoms are seen in many different digestive disorders. They do not necessarily mean that a person has diverticulosis. If an individual has these symptoms, he or she should see a healthcare professional.
Symptoms and Signs of Diverticulitis
Diverticulitis is a more serious condition and causes symptoms in most people with the condition that include:
- Pain in the abdomen, usually in the lower-left side
- Bleeding, bright red or maroon blood may appear in the stool, in the toilet , or on the toilet paper. Bleeding is often mild and usually stops by itself however, it can become severe.
- Fever
- Chills
- Constipation
- Worsening abdominal pain
- Vomiting
- Constipation for an extended period of time
- Burning or pain during urination
- Bleeding from the rectum
Symptoms and Signs of Ulcerative Colitis
- Frequent loose bowel movements with or without blood
- The urgency to have a bowel movement and bowel incontinence
- Lower abdominal discomfort or cramps
- Fever, lethargy, and loss of appetite
- Weight loss with continuing diarrhea
- Anemia due to bleeding with bowel movements
What Are The Treatments Complications And Risk Of Cancer For Diverticular Disease Vs Ulcerative Colitis
Diverticular Disease Treatment
A high-fiber diet is the mainstay of diverticulosis and diverticulitis prevention.
- Start a high-fiber diet because it will decrease the risk of complications and the accompanying symptoms however, will not make the diverticula a person has gone away. Foods high in fiber include:
- Whole-grain cereals and bread
- Fruits
- Vegetables
- Beans, peas, and lentils.
In the past patients with diverticulosis/diverticulitis were told that foods to avoid included seeds, corn, and nuts because it was thought fragments of these foods would get stuck in the diverticula and cause inflammation. However, current research has not found this to be the case, and the fiber content of such foods may benefit individuals with diverticulosis/diverticulitis. Discuss your diet or potential diet changes with your doctor.
Treatment for diverticulitis depends on the severity of the condition.
Treatment consists of IV or oral antibiotics, bowel rest, and possibly surgery.
If diverticulitis attacks are frequent or severe, the doctor may suggest surgery to remove a part of the patient’s colon.
- As with any surgery, there are risks the patient should discuss with his or her doctor.
- Sometimes the operation requires at least two separate surgeries on different occasions.
Recommended Reading: Medications For Ulcers Over The Counter
Southern Cross Medical Library
The purpose of the Southern Cross Medical Library is to provide information of a general nature to help you better understand certain medical conditions. Always seek specific medical advice for treatment appropriate to you. This information is not intended to relate specifically to insurance or healthcare services provided by Southern Cross. For more articles go to the Medical Library index page.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Also Check: Stelara Ulcerative Colitis Side Effects
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Recommended Reading: Stomach Ulcer And Chest Pain
Overview Of Ulcerative Colitis
While it can be overwhelming to receive a chronic disease diagnosis, learning all you can about ulcerative colitis will prepare you to manage your symptoms and live a full life.
Have you or a loved one been recently diagnosed with ulcerative colitis? Or were you diagnosed years ago but still dont fully understand your disease? Check out our latest video chat to learn more.
Video Length00:38:13
Video Chat: Ulcerative Colitis 101
Ulcerative colitis is a chronic inflammatory disease of the large intestine, also called the colon, that affects the lining of the colon and causes small sores, or ulcers, to form.
Those ulcers produce pus and mucous, which cause abdominal pain and the need to frequently empty your colon.
Video Length00:06:55
Ulcerative Colitis 101 This introductory video provides information on potential causes, symptoms, treatment and overall management of ulcerative colitis.
Enhancing Healthcare Team Outcomes
Ulcerative colitis is a systemic disorder with no cure. The disorder has numerous extraintestinal involvement in addition to the colon. Thus, it is best managed by an interprofessional team. All patients with the disorder need lifelong monitoring. Because of the risk of colorectal cancer, surveillance colonoscopy should occur every 1-2 years. Further, since patients are often treated with biological agents, they need to undergo screening for melanoma and nonmelanoma skin cancer.
The pharmacists should assist the team by educating the patient on the importance of medication compliance to avoid relapse. The nurse should encourage regular vaccinations, hand washing, and cancer screening. A dietary consult should be obtained to educate the patient on foods to eat and what not to eat, especially if they have a stoma. In addition, a stoma nurse should be involved in the teaching of stoma care.
An infectious disease nurse should monitor the patient in the outpatient setting to ensure that they are not immunocompromised. Social workers should be involved to ensure that the patient has ample support and finances so that the treatments are not missed. Patients with risk factors for osteoporosis need screening for bone mineral density periodically. Patients should be encouraged to undergo annual vaccination against influenza and pneumococcus. Finally, many patients with ulcerative colitis develop depression and anxiety and should be referred to a mental health counselor.
Outcomes
Don’t Miss: What Is The Best Thing To Put On Leg Ulcers