Change In Your Bowel Habits
In general, any change in your bowel habits is something to take note of. That could be a change in frequency or urgency, a change in how your poop looks, or the addition of symptoms like pain, abdominal cramping, pain, tenesmus, or mucus, pus, or blood in the stool. Any time symptoms persist or seem to get worse, and definitely any time there is blood in your stool, you should check in with your doctor.
Hemorrhoid Blood Clot Tips
Thrombosed hemorrhoids are the product of a blood clot forming inside of a external hemorrhoid.
External hemorrhoids can be painful and uncomfortable, and the formation of a blood clot inside of them certainly does not make it any better.
One of the most important things to remember is that a clot will usually go away on its own.
Dont try to pop a thrombosed hemorrhoid yourself, as you could develop an infection.
Instead, use wipes with witch hazel or creams designed for hemorrhoid relief to reduce swelling and discomfort.
Gently soak in a warm bath or a sitz bath for twenty minutes to alleviate the pain of a blood clot.
The best method of dealing with a blood clot is to see your physician or medical care provider.
Your blood clot may need to be lanced and drained, which is best left to a medical professional. Blood clots can leave behind a skin tag, and this can irritate through friction.
A proctologist or gastroenterologist should be able to help remove the blood clot safely and efficiently.
The most common procedures for removal of bloody hemorrhoids include:
Also Check: Offloading The Diabetic Foot For Ulcer Prevention And Healing
What Tests Are Done To Find Causes Of Blood In Stool
Your provider will check your pulse and blood pressure. He or she will probably also perform a rectal examination to look for hemorrhoids, fistulas, or fissures that could cause bleeding. You may need to have blood tests to check for anemia, clotting problems, and changes in your blood chemistry.
Your health care provider may recommend a colonoscopy.2 This procedure allows your provider to see inside your digestive tract and look for the source of bleeding. Colonoscopy is helpful for people with unexplained bleeding and bleeding that continues despite treatment. Colonoscopy is especially important if you have lost weight, are anemic, are older than 40, or have a family history of colorectal cancer.
Don’t Miss: Does Alcohol Affect Ulcerative Colitis
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
Blood In Stool And Ulcerative Colitis
Bleeding in ulcerative colitis can be significant and even contribute to anemia. Many patients with ulcerative colitis may require iron supplements to manage their anemia, along with other vitamin supplements.
In severe cases, bleeding in ulcerative colitis can be life threatening. If it cant be stopped, the rectum may have to be surgically removed.
Also Check: Does Ulcerative Colitis Cause Fever
Treatment By Disease Severity And Location
Mild-moderate distal colitis
- Oral aminosalicylates, topical mesalamine, or topical steroids
- Combination of oral and topical aminosalicylates is better than either alone
For refractory cases, oral steroids or IV infliximab can be used
Mild-moderate extensive colitis
- Oral sulfasalazine 4-6 g/day or alternative aminosalicylate 4.8 g/day
- Oral steroids for patients refractory to above therapy + topical therapy
- 6-MP or azathioprine for patients refractory to oral steroids, but not so severe as to require IV therapy
- Infliximab in patients who are steroid refractory/dependant on adequate doses of 6-MP/thiopurine or who are intolerant to these medications
Severe colitis
- Infliximab if urgent hospitalization is not needed
- If patient is toxic, should be admitted to the hospital for IV steroids
- Failure to improve in 3-5 days is indication for colectomy or IV cyclosporine
Indications for Surgery
- Absolute: Hemorrhage, perforation, documented or strongly suspected cancer
Also, surgery is recommended for severe colitis refractory to medical therapy
What Is Bloody Stool Like With Uc
Many MyCrohnsAndColitisTeam members have discussed bleeding and bloody stools with UC. As one member wrote, although the frequency of their bowel movements had decreased, this symptom persisted. I hadnt used the toilet for 12 hours, but when I did, I had bloody, loose stools. Afterward, I had a semi-normal stool, they wrote. They went on to ask members whether their experience was common, to which others replied that they had dealt with similar issues while managing their UC.
As one member advised, Its normal for being in a flare, which you are. You need to see your doctor so they can get something to help you. They probably will give you prednisone to get you under control.
Users also frequently report experiencing other gastrointestinal symptoms with bloody stools. One member shared that they were having diarrhea and bloody stools on one of their particularly bad days, while another said they were experiencing abdominal pain, urgency, diarrhea, some bloody stools, and nausea for the past week, despite taking medication for the last five months.
You May Like: Best Probiotic Brand For Ulcerative Colitis
What Are Immunomodulator Medications
Immunomodulators are medications that weaken the body’s immune system. The immune system is composed of immune cells and the proteins that these cells produce. These cells and proteins serve to defend the body against harmful bacteria, viruses, fungi, and other foreign invaders. Activation of the immune system causes inflammation within the tissues where the activation occurs. Normally, the immune system is activated only when the body is exposed to harmful invaders. In patients with Crohn’s disease and ulcerative colitis, however, the immune system is abnormally and chronically activated in the absence of any known invader. Immunomodulators decrease tissue inflammation by reducing the population of immune cells and/or by interfering with their production of proteins that promote immune activation and inflammation. Generally, the benefits of controlling moderate to severe ulcerative colitis outweigh the risks of infection due to weakened immunity. Examples of immunomodulators include azathioprine , 6-mercaptopurine , cyclosporine , and methotrexate .
Azathioprine and 6-MP
Azathioprine and 6-MP are increasingly recognized by doctors as valuable drugs in treating Crohn’s disease and ulcerative colitis. Some 70% of patients with moderate to severe disease will benefit from these drugs. Because of the slow onset of action and the potential for side effects, however, 6-MP and azathioprine are used mainly in the following situations:
Other Issues in the Use of 6-MP
Methotrexate
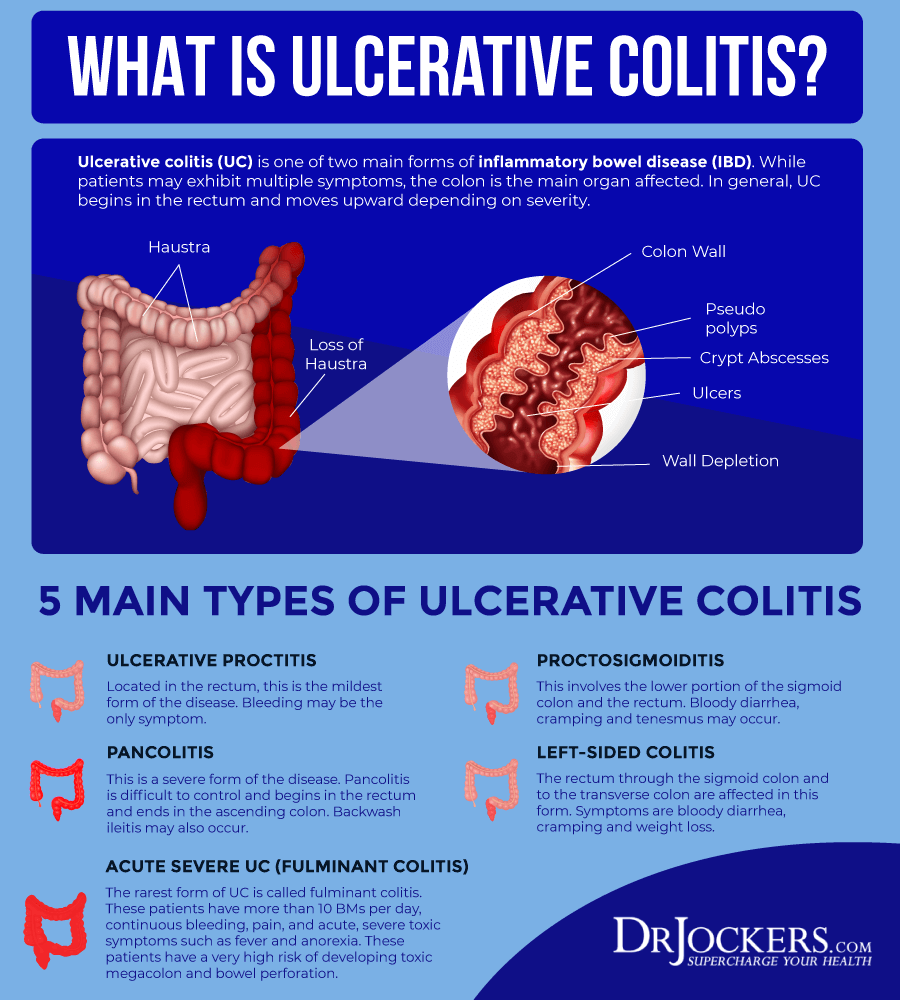
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Don’t Miss: Can Stomach Ulcers Cause Diarrhea
How Is It Evaluated And Diagnosed By Doctors
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Bleeding In Crohn’s Disease
Crohn’s disease causes blood in the stool less commonly than does ulcerative colitis, but this will vary between patients based on where the Crohn’s is causing the inflammation.
Crohn’s disease that is found in the colon or rectum, rather than in the small intestine, is more likely to cause blood to appear in or on the stool. Treating blood loss from Crohn’s disease will be similar to that in ulcerative colitis:
- Getting the IBD under control
- Supplementing with vitamins
- Blood transfusion, if necessary
- Surgery, if necessary
With Crohn’s disease, resection surgery may be done in order to remove the parts of the intestine that have been damaged by inflammation. J-pouch surgery isn’t usually done for Crohn’s disease because the Crohn’s may reappear in the pouch.
Blood loss can also occur when an anal fissure has developed as a complication of Crohn’s disease. Fissures are more common with Crohn’s than they are with ulcerative colitis. In most cases, fissures can be treated successfully without surgery.
Also Check: How To Prevent Pressure Ulcers In The Hospital
Its Time For Some Potty Talk Because What You Find In Your Toilet Bowl Can Reveal A Lot About Your Uc
by Health Writer
Consistency, liquidity, shape, smell, frequency. Whether or not youre living with ulcerative colitis , chances are those words immediately make you think about poop. But if you do have UC, an inflammatory bowel disease that causes painful intestinal cramping and frequent bathroom runs, those five worlds just might be your mantra.
Everybody poops, but anyone with IBD can attest to how big of a role bowel movements can play in daily life. Truth is, your poopand how often nature callscan reveal a lot about your disease and whether a flare of your worst symptoms is on the horizon. So much so that its worth taking a look in the toilet bowl every now and then.
Here, we talk to top poop experts, who break down what your bodys waste can reveal.
Reducing Blood In Stools
prebiotic supplement may help reduce bloody stools and other symptoms of UC.
Participants taking the prebiotics supplement experienced significantly decreased abdominal pain and cramping. They also reported reduced nausea, vomiting, diarrhea, and blood in stools, although these effects were not statistically significant.
The study was small, so more research is needed to determine the best way to reduce blood in stools.
If a person frequently has bloody stools, a doctor may prescribe iron supplements to help prevent anemia.
Also Check: Best Medicine For Ulcerative Colitis
What Does Blood In Stools Look Like
Blood from your stool could look bright red, or it might be dark red or black.
How the blood looks depends on where it is coming from.
Spots of red blood on the toilet paper, drops in the toilet bowl, blood on the surface of your stool or in your underwear indicate the bleeding is coming from the anus or lower rectum.
If the blood is mixed in with your stool, this suggests bleeding might be from higher up in the bowel.
If your stools are black and like tar, and they smell bad, this is also probably because the blood is coming from higher up in the bowel.
Why Blood Clots Are More Common In People With Ibd
Its well known that inflammatory bowel disease is associated with whats called extra-intestinal manifestations: conditions that are related to IBD but arent found in the digestive tract. One of these is the risk of developing blood clots.
The increased risk of blood clots in people with Crohns disease and ulcerative colitis is known to IBD experts but it may not be as well understood by other physicians and by people who have IBD. Its unclear exactly why people with IBD are at risk for blood clots but its thought to have to do with disease activity and changes in the blood that promote clotting.
While the risk of blood clots has been shown to be higher in people with IBD, there are things that can be done to prevent them. Whats vital is that people with IBD understand their personal risk of blood clots and that physicians take steps to avoid this complication when necessary, such as after surgery. People with IBD can also familiarize themselves with symptoms of a blood clot, such as pain, swelling, tingling, and pale skin in one leg.
Recommended Reading: Do Probiotics Help Stomach Ulcers
Increase Dietary Fiber And Fluid Intake
Increasing dietary fiber can help to relieve many of the digestive conditions that lead to rectal bleeding and pooping bloody stools. Fiber can help to relieve the symptoms of hemorrhoids, anal fissures, diverticulitis, and constipation. It is important to note that since fiber draws water into the stool to make it softer, its essential to consume enough water or other fluids on a regular basis to help the fiber work.
According to the PubMed Health, fiber can help to soften stool and make them easier to pass. This can help to ease digestive discomfort and prevent conditions like constipation that can lead to enlarged hemorrhoids. It was reported that increased fiber in the diet also reduces the frequency of rectal bleeding and bloody stools.17
Always increase fiber slowly to prevent uncomfortable side effects, such as gas and bloating, constipation, diarrhea and abdominal pain.
Causes And Treatment Of Occult Blood In Stool
1. Anal fissure
- Definition: Minor rip that occurs when anal tissue is stretched when straining during a hard bowel movement, resulting in rectal bleeding and extreme pain.
- Treatment: Anal fissures typically resolve on their own within 4-6 weeks. Treatment may include dietary fiber and stool softeners, as well as lotions applied to the afflicted area.
2. Crohn’s disease
- Definition: A type of chronic inflammatory bowel disease that causes abdominal pain, severe diarrhea, exhaustion, weight loss, and rectal bleeding due to inflammation in the digestive tract.
- Treatment: Crohn’s is incurable. To slow the progression of illness, however, dietary modifications and medications such as steroids and immunosuppressants may be recommended. If these measures do not work, surgery may be necessary. Patients with Crohn’s disease may require routine colorectal cancer screening due to an elevated risk.
3. Diverticular disease
- Definition: Diverticula are small pockets that form and push through weak places in the colon wall, caused by straining during bowel movements. Diverticulitis occurs when the pockets become infected or inflamed, causing nausea, vomiting, and rectal bleeding.
- Treatment: Antibiotics can be used to treat diverticulitis symptoms. If complications develop or if other treatment options fail and the condition is severe, surgery may be required.
4. Colonic polyps
5. Hemorrhoids
6. Meckel’s diverticulum
7. Vascular conditions
8. Ulcerative colitis
9. Ulcers
You May Like: Ulcerative Colitis How Much Blood Is Too Much
Bleeding In Ulcerative Colitis
Bleeding from the rectum is more common in ulcerative colitis than it is in Crohn’s disease.
Ulcerative colitis often involves the rectum. Because the rectum is at the end of the large intestine, blood from this source is quite visible in or on the stool.
Bleeding also occurs with ulcerative colitis because this form of IBD attacks the lining of the large intestine. The ulcers that form in the mucosa of the large intestine tend to bleed.
Ulcerative Colitis: Causes And Risk Factors
Causes
Experts dont know what causes ulcerative colitis, but it may be related to your immune system. Normally, your immune system attacks bacteria and viruses that could make you sick. However, with UC, the immune system mistakes the cells of your large intestine for a threat and attacks. When your immune system attacks your own healthy cells, it is referred to as an autoimmune condition. This causes inflammation and ulcers.
Why some people develop ulcerative colitis and not others is still being studied. It may have to do with genetic factors. You are more likely to develop UC if a family member has it. However, most cases develop in people without a family history.
Environmental factors, like exposure to certain viruses or bacteria, may also play a role. Your body may try to fight this infection and then overreact.
Doctors used to think that excess stress and certain foods cause ulcerative colitis, but we now know this isnt true. Diet and stress can make symptoms worse, but they dont cause them.
Risk factors
A risk factor is anything that increases your chance of developing a certain disease. Some risk factors for ulcerative colitis include:
Read Also: Ulcerative Colitis Surgery Recovery Time
Lifestyle Changes And Behavioral Treatments To Ease Constipation
There arenât specific guidelines to manage UC with constipation. But you can take steps to boost your bowel movements, including:
Change your diet. Your doctor might urge you to eat more fruits, vegetables, and whole grains. But keep track of how you feel after you eat plant-based foods. Too much fiber can make your poop bulky. That can be a good thing. But it might worsen constipation in some people with UC.
Always check with your doctor before you make any big changes to your diet. But some things that may help UC with constipation include:
- Adding soluble fiber
- Reducing your dietary fiber until symptoms get better
- Trying a low-FODMAP diet
- Avoiding dairy foods
Stay hydrated. Extra fluid can soften your stool so itâs easier to pass. Youâve probably heard that you should aim for 8 cups of water a day. But there isnât a perfect number that works for everyone. Drink when you feel thirsty. And pay attention to the color of your urine. It should be clear or light yellow.
Get moving. Regular physical activity can urge your stool to move along. Talk to your doctor about activities that are safe during or after a flare. Some examples of UC-friendly exercises might include:
- Fast walking
- Elliptical
- Rowing
Try biofeedback. This is a kind of therapy to retrain the muscles that help you poop. A pelvic floor therapist or physical therapist can let you know if this kind of treatment might be right for you.
You might want to ask your doctor or therapist about the following: