Advanced Therapies For Diabetic Foot Ulcers
Physicians of individuals with diabetic foot ulcers may have difficult decisions to make if wounds do not heal. Many of these patients have a significant cardiac risk and health care practitioners need to make complicated decisions about whether to perform invasive procedures like angiography. Other options can be:
- Covering the wound with cultured human cells.
- Heterogenetic dressings or grafts with recombinant growth factors.
- Hyperbaric oxygen therapy.
Diabetes And Diabetic Foot Ulcers
According to the Centers for Disease Control , an estimated 30 million people in the United States have diabetes, including 7 million who are unaware they are living with the disease. The percentage of adults with diabetes increases with age, reaching a high of 25 percent among those aged 65 years or older, according to the Amputee Coalition. In addition to age, risk factors for diabetes also include diet, activity level, obesity and heredity.
Diabetes may be accompanied by other co-existing conditions such as blindness, heart disease, kidney failure or lower-limb amputation.
High blood sugar levels, poor circulation, immune systems issues, nerve damage and infection may contribute to a non-healing diabetic foot ulcer. Four to 10 percent of people living with diabetes will develop a foot ulcer. An estimated 15 percent of people with foot ulcers will experience a major amputation. Even more alarming, people with an amputation have a 50 percent mortality rate within five years.
There are several common factors of diabetic foot ulcers including neuropathy, peripheral arterial disease , deformities and Charcot foot. Neuropathy is a result of damage to peripheral nerves and often causes weakness, numbness and pain in hands and feet. Similarly, PAD is caused by narrowed arteries which reduces blood flow to the limbs. Charcot foot is a deformity that results from nerve damage in the foot or ankle, which may cause injuries to go untreated, leading to the breakdown of joints.
What Are Arterial Ulcers
A condition called peripheral arterial disease can reduce blood flow to your extremities. When this happens, your foot tissue may start to die. The ulcers that form from reduced blood flow are called arterial ulcers.
The word arterial means relating to arteries. Arteries are blood vessels that transport blood from your heart to the rest of your body, including your feet and toes. Anyone can get an arterial ulcer, but people who smoke or have diabetes, high blood pressure or high cholesterol are at higher risk.
Unlike neurotrophic ulcers, arterial ulcers can form on many parts of your body, including:
- On the tips of your toes.
- Between your toes .
- The bony parts of your feet and toes that rub against bed sheets, socks or shoes.
Arterial ulcers are:
- An unusual walk that puts too much pressure on one part of your foot or toe.
- Friction when your foot or toe rubs against the toe box of your shoe.
Although they dont cause ulcers, foot and toe ulcers are often found alongside toe conditions such as hammertoe, mallet toe and claw toe.
You May Like: Foods Bad For Stomach Ulcers
Risk Factors Of Dfu Mortality
In August 2022, DFU follow-up data were collected via telephone interview with the patient or the patients family. A total of 653 individuals out of 2131 were successfully followed up, while 219 DFU patients perished. These results demonstrated that 33.6% of DFU employees perished .
FIGURE 1. Clinical outcomes of DFU: death, non-healing, and healing. A total of 653 patients underwent successful follow-up, of which 33.6% of DFU patients lost their lives, 62.6% of DFU patients were healing, and 3.8% of DFU patients were non-healing.
According to diabetic foot ulcer patients follow-up data, three types can be identified: death, healing, and non-healing. In univariate analysis, mortality correlated with advanced age , diabetes duration vs. 16 years, healing vs. non-healing p= 0.018), retinopathy , C-reactive protein vs. 8.9 , death vs. healing p= 0.005), albumin vs. 38.1 , death vs. healing p< 0.0001), creatinine vs. 72.7 , death vs. healing p= 0.007), and procalcitonin vs. 0.04 , death vs. healing p= 0.007) .
TABLE 3. Comparison of risk factors for DFU mortality. *p< 0.05, **p< 0.01, and ***p< 0.001.
After adjusting for age, diabetes duration, retinopathy, C-reactive protein, albumin, creatinine, and procalcitonin, a logistic regression analysis identified only age and albumin as independent predictors of death . Higher DFU mortality was significantly associated with increasing age and decreasing albumin levels.
Ix In Which Patients With A Diabetic Foot Infection Should I Consider Surgical Intervention And What Type Of Procedure May Be Appropriate

Recommendations
-
38.We suggest that nonsurgical clinicians consider requesting an assessment by a surgeon for patients with a moderate or severe DFI .
-
39.We recommend urgent surgical intervention for most foot infections accompanied by gas in the deeper tissues, an abscess, or necrotizing fasciitis, and less urgent surgery for wounds with substantial nonviable tissue or extensive bone or joint involvement .
-
40.We recommend involving a vascular surgeon early on to consider revascularization whenever ischemia complicates a DFI, but especially in any patient with a critically ischemic limb .
-
41.Although most qualified surgeons can perform an urgently needed debridement or drainage, we recommend that in DFI cases requiring more complex or reconstructive procedures, the surgeon should have experience with these problems and adequate knowledge of the anatomy of the foot .
Recommended Reading: How To Gain Muscle With Ulcerative Colitis
Establishing Extent Of Infection
Early recognition of the area of involved tissue can facilitate appropriate management and prevent progression of the infection . The wound should be cleansed and debrided carefully to remove foreign bodies or necrotic material and should be probed with a sterile metal instrument to identify any sinus tracts, abscesses, or involvement of bones or joints.
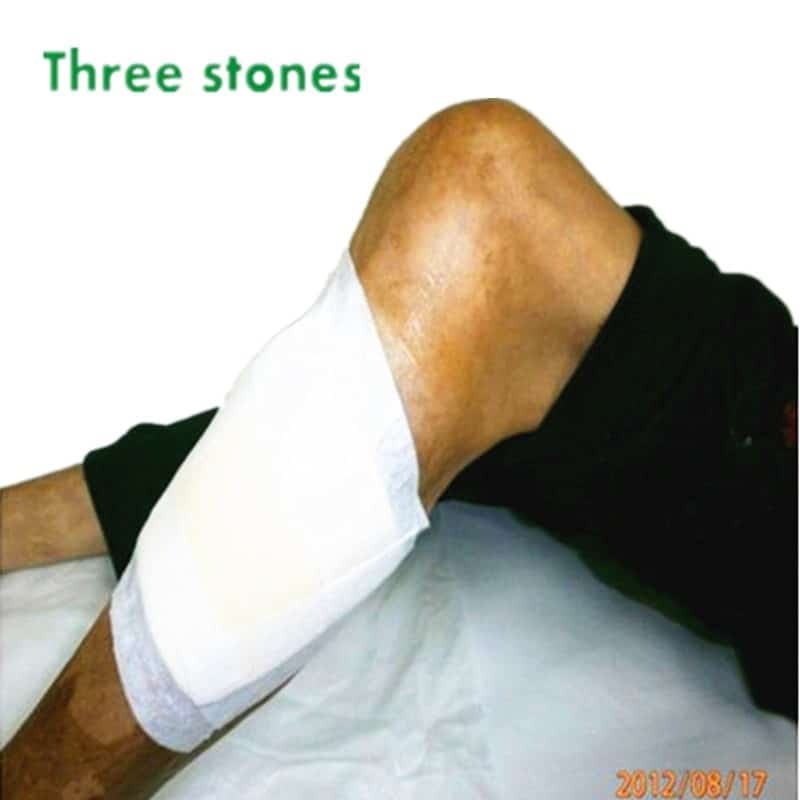
Plantar foot ulcers with a deep space infection.
Figure 3.
Plantar foot ulcers with a deep space infection.
Osteomyelitis is a common and serious complication of diabetic foot infection that poses a diagnostic challenge. A delay in diagnosis increases the risk of amputation.13 Risk factors associated with osteomyelitis are summarized in Table 1.3,1316 Visible bone and palpable bone by probing are suggestive of underlying osteomyelitis in patients with a diabetic foot infection.1314 Laboratory studies, such as white blood cell count and the erythrocyte sedimentation rate , have limited sensitivity for the diagnosis of osteomyelitis. Osteomyelitis is unlikely with normal ESR values however, an ESR of more than 70 mm per hour supports a clinical suspicion of osteomyelitis.13 Definitive diagnosis requires percutaneous or open bone biopsy. Bone biopsy is recommended if the diagnosis of osteomyelitis remains in doubt after imaging.3
Wound lacking purulence or any manifestations of inflammation
Guidelines For Infection Control In The Treatment Of Diabetic Ulcers
Preamble: Infection results when the bacteria: host defense equilibrium is upset in favor of the bacteria. Infection plays various roles in the etiology, healing, operative repair, and complications of diabetic ulcers.
Guideline #3.1: Remove all necrotic or devitalized tissue by surgical, enzymatic, mechanical, biological, or autolytic debridement. .
Principle: Devitalized tissue provides a safe haven for bacterial proliferation, a barrier for antibiotics to reach bacterial pathogens. In addition, it limits the bodys cellular defenses to fight infection. Removal of devitalized tissue reduces bacterial bioburden.
Guideline #3.2: If there is suspected infection in a debrided ulcer, or if epithelialization from the margin is not progressing within two weeks of debridement and initiation of offloading therapy, determine the type and level of infection in a debrided diabetic ulcer by tissue biopsy or by a validated quantitative swab technique.
Principle: High levels of bacteria impede wound healing and surgical wound closure. Reduction of the bacterial bioburden in the wound reduces the risk of clinical infection and improves wound healing. Cultures should be performed to isolate both aerobic and anaerobic bacteria.
Guideline 3.8: If osteomyelitis is suspected, determine the type of bacterial pathogens by bone biopsy .
You May Like: What Is A Gastric Ulcer And What Is Its Cause
Read Also: Difference Between Colon Cancer And Ulcerative Colitis Symptoms
Preventive Care And Treatment
Preventive measures against the risk of amputation include regular foot examination, evaluation of amputation risk, regular callus debridement, patient education, professionally fitted therapeutic footwear to reduce plantar pressure and accommodate foot deformities, and early detection and treatment of diabetic foot ulcers . Many studies that have assessed interventions to prevent and treat diabetic foot ulcers have had limited quality of supportive evidence because of problems in study design and methods . However, the treatment of foot ulcers typically is most effective with an interprofessional approach and includes measures to improve glycemic control, decrease mechanical pressure with off-loading, treat infection, ensure adequate lower-extremity arterial inflow and provide local wound care .
| Table 3 |
|---|
|
Treatment of the acute Charcot foot requires immobilization of the foot, typically for several months, in a total contact cast, removable walker boot or custom orthosis until consolidation occurs . Surgical stabilization may be indicated for Charcot arthropathy associated with marked instability, deformity or nonhealing ulcers. Although bisphosphonates have been considered for the treatment of Charcot arthropathy, further studies are necessary to fully evaluate these agents and other medical therapies in the routine treatment of Charcot arthropathy .
Recommended Reading: How Do You Cure Mouth Ulcers
How Big Are Foot And Toe Ulcers
There are many different sizes of ulcers. They start as small as 1 centimeter wide and can grow to the size of your entire foot if left untreated.
The depth of the ulcer can change, too. Several different classification systems exist to define the depth of an ulcer. The Wagner Diabetic Foot Ulcer Grade Classification System, for example, has six grades:
- Grade 0: Your skin is intact .
- Grade 1: The ulcer is superficial, which means that the skin is broken but the wound is shallow .
- Grade 2: The ulcer is a deep wound.
- Grade 3: Part of the bone in your foot is visible.
- Grade 4: The forefront of your foot has gangrene .
- Grade 5: The entire foot has gangrene.
Don’t Miss: What To Avoid Eating If You Have An Ulcer
Diabetic Foot Ulcer Home Treatment
A diabetic foot ulcer is an open wound that happens due to uncontrolled sugar levels in diabetes patients. It is a troublesome condition that hinders a person from carrying on their daily routines. The worst part about diabetic foot ulcers is that person may not even be aware of its growing seriousness due to the damaged sensation of the affected area.
If you suffer from this problem of a diabetic foot ulcer, here is a sigh of relief for you in the name of home treatments or remedies. Yes, there are things that you can try at home to treat diabetic foot ulcers to some extent.
Healing Tips For Diabetic Wound Care And Ulcers Of The Foot
Patients with diabetes can be at risk for diabetic foot ulcers, infections, and complications from those infections. Diabetic foot ulcers or wounds put patients at a higher risk of hospitalization and need for surgery or amputation. In fact, according to the CDC, there are 130,000 hospitalizations a year for amputations in those with diabetes. Up to 11.8% of those with diabetes have a wound and many may go on to need surgery. This means that wound care for diabetic foot ulcers as well as prevention is of the utmost importance.
As physicians, we have to use our resources and work with patients in order to heal diabetic foot wounds to prevent such complications. If a patient also has numbness in their feet, they may not feel a foot wound developing. Diabetic foot sores that start from a small scrap or cut can unknowingly form into a deep ulcer. Checking your feet and keeping your blood sugar
Whether you have diabetes or are caring for a loved one requiring foot diabetic wound treatment, Certified Foot and Ankle Specialists can effectively help your wound heal and prevent further complications. Here we will discuss diabetic foot care and how to minimize the traumatic consequences of ulcers.
How do we care for diabetic foot wounds and how does one clean a diabetic foot wound?
For proper wound care, clean the wound with saline, apply a topical gel or antibiotic ointment medication to the wound once a day, as recommended by your doctor.
Preventing diabetic wounds
Don’t Miss: What Is Peptic Ulcer Pain Like
Its Been Longer Than Four Weeks
If wounds dont heal within a month, they are considered chronic wounds. While its possible for chronic wounds to heal on their own, its best to get a doctors help to identify why the wound isnt healing and provide treatment.
Our Wound Healing Center offers advanced treatments for severe and chronic diabetic wounds
Sensory And Autonomic Neuropathy
Distal symmetric polyneuropathy is perhaps the most common complication affecting the lower extremities of patients with diabetes mellitus. This complication occurs in up to 58 percent of patients with longstanding disease.19 Neuropathy, a major etiologic component of most diabetic ulcerations, is present in more than 82 percent of diabetic patients with foot wounds.4 This lack of protective sensation, combined with unaccommodated foot deformities, exposes patients to undue sudden or repetitive stress that leads to eventual ulcer formation with a risk of infection and possible amputation.20
In the diabetic foot, autonomic neuropathy has several common manifestations. First, denervation of dermal structures leads to decreased sweating. This causes dry skin and fissure formation, which predispose the skin to infection. In vascularly competent patients, this autosympathectomy may lead to increased blood flow, which has been implicated as one of the primary etiologic factors in the development of Charcot’s joint and severe foot deformity.2123
The nylon monofilament test is a simply performed office test to diagnose patients at risk for ulcer formation due to peripheral sensory neuropathy.24 The test is abnormal if the patient cannot sense the touch of the monofilament when it is pressed against the foot with just enough pressure to bend the filament25 . Physicians can obtain a monofilament kit at a small cost from the National Diabetes Information Clearing-house .
Also Check: Gel Cushion For Pressure Ulcers
Guidelines And Conflicts Of Interest
All members of the expert panel complied with the IDSA policy regarding conflicts of interest, which requires disclosure of any financial or other interest that might be construed as constituting an actual, potential, or apparent conflict. Members of the expert panel were provided a conflicts of interest disclosure statement from IDSA and were asked to identify ties to companies developing products that might be affected by promulgation of the guideline. The statement requested information regarding employment, consultancies, stock ownership, honoraria, research funding, expert testimony, and membership on company advisory committees. The panel was instructed to make decisions on a case-by-case basis as to whether an individuals role should be limited as a result of a conflict, but no limiting conflicts were identified.
Caution About Diabetic Foot Ulcer:
- Caution should be exercised in case of sudden pain and swelling of the legs, blisters, small sores, piercing of the feet, hot water or hot objects.
- If the toenails become thick and curved and enter the toes, if there is any structural defect in the toes. If you have a history of any previous wound on your feet, the sensation of the feet is so low that you do not feel the feeling of cold or heat, but you should be careful and seek medical attention. It is best to have your feet checked every three to six months.
- Wear flat, soft, hard-soled leather shoes instead of sandals when going out. So that no sharp object pierces the sole of the shoe and creates sores on the feet. I also want the size of the shoes to be right, so that it is neither big nor small.
You May Like: What Not To Eat With Bleeding Ulcers
Don’t Miss: Herbal Medicine For Stomach Ulcer
Customer Care Center And Patient
If you have questions about any Organogenesis products, policies, or programs, we’ve got answers. Our Customer Care Center offers the following services dedicated to providing the best possible customer journey.
- Dedicated and trained staff
- Return goods and cancellation policy
- Standing order and on-demand programs
- Product experience program
- Free shipping and order tracking
Organogenesis is committed to providing access to our products for those most in need through our patient-focused programs. These programs can assist patients with limited financial resources who also have no public or private insurance coverage.
Keep Your Nails Clean
Whether you have diabetes or not, neglecting your toenails unclean and unhygienic. It is not advisable for diabetic patients to trim their nails. But dont let this be an excuse for you to go on with unclean toenails, as bacteria could easily reproduce and reach your wound, leading to infection. There are doctors who specialize in foot care called podiatrists, and they will help you keep your foot maintained and your foot ulcer safe.
Don’t Miss: How To Get Rid Of Stomach Ulcer Pain
Treatment By Npwt In Combination With Prp
The treatment efficacy of NPWT alone and NPWT combined with PRP therapy for DFU was evaluated. There are two groups. The combined group was treated with NPWT first and then PRP, while the control group was treated with NPWT first and then traditional dressings. A total of 31 DFU patients meeting the inclusion criteria were recruited. There were no significant differences between these two groups concerning basic characteristics such as age, gender, HbA1c, hypertension, nephropathy, retinopathy, neuropathy, diabetes duration, C-reactive protein, and procalcitonin . In terms of healing time, however, ulcers in the combination group d) healed much faster than ulcers in the control group d) . Quantitatively, the combined groups 93.8% healing rate was much greater than the control groups 53.3% healing rate. The combined groups mortality rate of 6.3% dropped more sharply than the control groups mortality rate of 40% . Overall, this study indicated that, compared to NPWT paired with standard dressing, NPWT combined with PRP therapy could accelerate ulcer healing and reduce DFU mortality.
TABLE 5. Comparison of the combined group and control group, follow-up wound healing time, and outcome in the two groups. *p< 0.05, **p< 0.01, and ***p< 0.001.