Comparison Of Symptoms Reported In Focus Groups To Symptoms From Pooled Disease Activity Indices
The lists were directly compared to determine which symptoms were present in both the focus group list and in the common indices list which symptoms were only present in the indices and which symptoms were reported by patients to be important, but were not measured by any of the common disease activity indices.
What Triggers An Ulcerative Colitis Flare
Triggers of ulcerative colitis flare-ups vary from person to person. It is helpful to identify factors that trigger or worsen your symptoms in order to try and avoid them. You may want to use a symptom diary or tracking app. Some of the most common include:
- **Diet. **Certain foods may trigger flares or worsen symptoms. Try to identify any foods that impact your ulcerative colitis.
- Medications. Pain relieving medications such as non-steroidal anti-inflammatories or antibiotics can worsen symptoms of ulcerative colitis
- Not taking medication as prescribed. Missing ulcerative colitis medications or taking an incorrect dose can lead to a flare-up.
- Stress. In some people, stress may impact ulcerative colitis symptoms.
Are There Pancolitis Complications To Be Aware Of
The most alarming short-term complication of pancolitis is a rare condition called toxic megacolon.5 Thats when your colon becomes dilated due to inflammation and eventually perforates , which can be fatal, Dr. Schwimmer says. When toxic megacolon is discovered, he says, it means the person needs surgery immediately.
One bright spot, Dr. Schwimmer says, is that toxic megacolon happens less these days because people are more aware of ulcerative colitis symptoms, and modern medications work much better to control inflammation.
A longer-term consequence of pancolitis is an increased risk of colon cancer. Still, the risk is pretty lowabout 2% for someone who has had ulcerative colitis symptoms for at least 10 years, according to an older study published in the World Journal of Gastroenterology.6 The more colon tissue you have that is inflamed, the higher your cancer risk becomes. Since pancolitis affects the whole colon, it means more opportunity for inflammation. Thats why its extremely important for people with IBD to be screened for colon cancer according to their doctors recommendation.
You May Like: Removing Colon Due To Ulcerative Colitis
Analysis Of Focus Group Data
Each focus group meeting was audiotaped and fully transcribed. Each transcript was entered into NVivo version 2.0. Two members of the study team independently reviewed each transcript with a holistic view of symptoms and themes from each of the five focus group meetings and generated a list of symptom domains and common themes discussed by participants of each focus group . These lists were compared for agreement and consensus was reached . This list served as a template for a coding scheme used to analyze each transcript. The transcripts were independently coded by symptom domain and theme by J.C.J. and A.K.W. and codes were compared for agreement.
Managing Ulcerative Colitis Flare
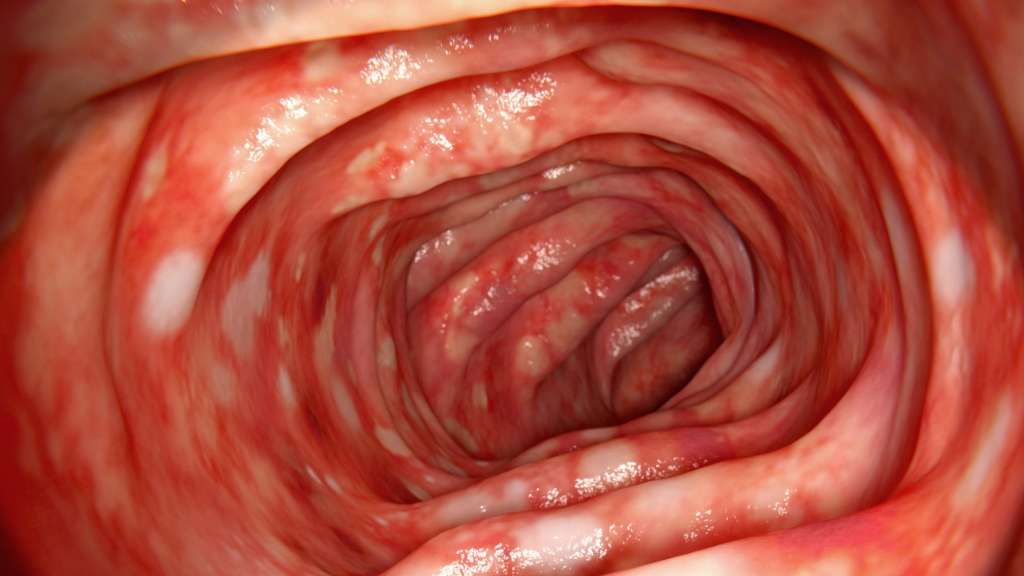
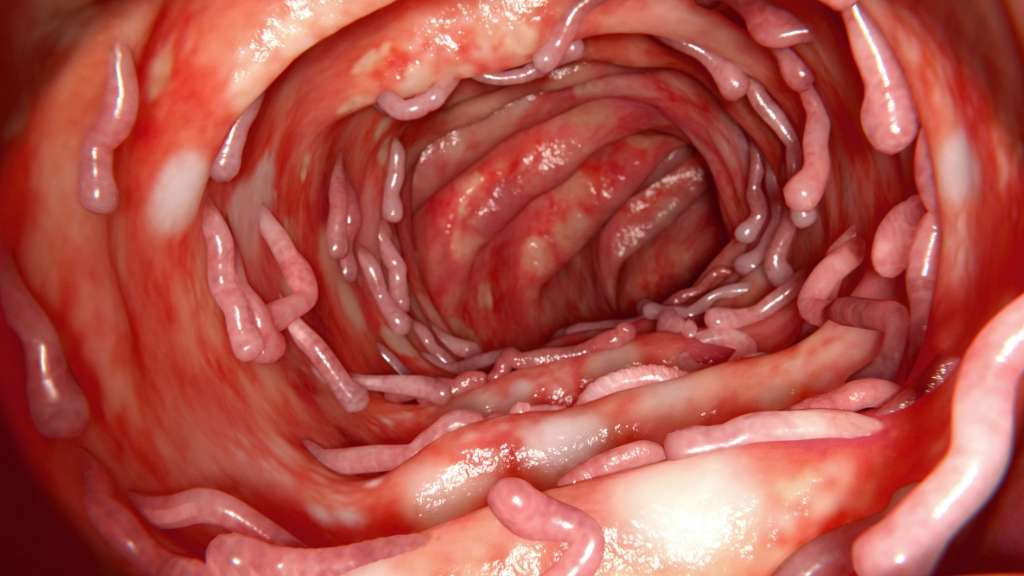
Ulcerative colitis is a form of inflammatory bowel disease that affects the mucosal lining of the large intestine and rectum, causing inflammation and ulcers in the digestive tract. People with ulcerative colitis experience periods of remission, during which symptoms subside, and flare-ups, during which symptoms return or worsen.
The symptoms of an ulcerative colitis flare may vary depending on the severity of the inflammation and where it occurs. Generally, the most common symptoms of UC flares are abdominal pain, cramping, and diarrhea . Most people with ulcerative colitis experience mild to moderate symptoms, while others may have more serious symptoms, including fever, severe abdominal cramping, and bloody stools.
Flares can be difficult to manage and may interfere with day-to-day life. Luckily, there are ways to manage these symptoms both with your doctor and at home.
You May Like: Is Ulcerative Colitis And Colitis The Same Thing
When Youre In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
When To See A Doctor
Maybe its food poisoning or a stomach bug.
I really dont want to bother the doctor.
Sound familiar? While its totally normal to want to talk yourself out of going to see your doctor, this is probably not the best approach.
Honestly, I prefer that patients tell me right away when they start having symptoms, so we can treat the flare early and often with simpler measures before it becomes more severe and more complicated or requires hospitalization, Dr. Charabaty says.
If you any ulcerative colitis symptoms flare up, call your doctor so you both can work to see whats going on and keep your symptoms from worsening. If you have severe abdominal pain and a high fever, its best to head to the emergency room, according to the Crohns and Colitis Foundation.
When you do see a doctor, this isnt a time to shy away from talking about how ulcerative colitis is affecting more than your belly, if thats the case for you.
It is really important for women with ulcerative colitis to talk about their mental health with their treating physicians and it is crucial to treat depression and anxiety as a part of a comprehensive care of IBD, Dr. Charabaty says. The mental health affects the physical health and vice versa, and both components need to be addressed to keep ulcerative colitis in remission and improve quality of life.
Read Also: I Think I Have An Ulcer What Should I Do
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Recommended Reading: What Causes Ulcers To Flare Up
What Foods Trigger Colitis
Ulcerative colitis is a chronic type of inflammation in the bowel. Today, about 750,000 people in the U.S. are living with this disease. To improve this potentially debilitating condition, colitis sufferers must closely watch their food consumption to help maintain a healthier colon and avoid triggering a disease flare-up. This article will help you understand colitis and how to avoid symptoms by changing what you eat.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Also Check: Treating Hindgut Ulcers In Horses
Eating Healthy Diet Will Surely Ease Flare
Eating healthy diet will absolutely ease flare-up of ulcerative colitis. Always confirm your diet is healthy and avoid consumption processed foods. Also, you must avoid sweet and spicy foods in your diet, as they cause irritation to your colon. Your diet ought to be composed of vegetables as a serious supply of super molecule. The vegetables ought to be recent and leafed inexperienced, as they are a decent supply of naphthoquinone. Naphthoquinone deficiency is associated to redness being severe. Additionally, avoid consumption beef however instead supply super molecule from chicken and turkey or baked fish. Beef causes stress in your colon.
How Can You Get Tested For Ulcerative Colitis
Someone can visit a clinic like the new Digestive Health Centre at OneWelbeck in London, meet with a specialist, and have tests carried out to provide a clear diagnosis.
For patients who already know that they have ulcerative colitis, it is possible to have your history reviewed and some diagnostic procedures carried out to see if any treatment options may be of benefit.
Recommended Reading: Signs And Symptoms Of Ulcerative Colitis Flare Up
Get Support For Your Ibd Today
MyCrohnsAndColitisTeam is the social network for people diagnosed with IBD and the people who love, support, and care for them. More than 142,000 members come together to ask questions, give advice, and share their experiences of life with IBD.
Have you experienced chills with Crohns disease or ulcerative colitis? Share your experience in the comments below or by posting on MyCrohnsAndColitisTeam.
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Don’t Miss: Is Soy Milk Good For Ulcerative Colitis
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
How Can I Identify Patients With Ulcerative Colitis
A combination of history, assessment of endoscopic and radiological appearances, histology, and microbiology is needed to diagnose colitis . The cardinal symptoms of ulcerative colitis are:
-
Bloody diarrhoea
-
Urgency
-
Tenesmus .
Mild distal colitis, in which rectal bleeding may be absent, can mimic irritable bowel syndrome. Colicky lower abdominal pain may occur, but severe pain is usually limited to severe colitis.
Stool cultures should be performed even in patients with a relapse of known ulcerative colitis. The presence of bloody diarrhoea for more than three weeks should alert the doctor to the possibility of inflammatory bowel disease, and endoscopy should be performed.
Read Also: How To Treat Sacral Pressure Ulcer
Also Check: What To Do When You Have An Ulcer
What Are The Treatment Options For A Flare
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines – see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
Don’t Miss: What Does Asacol Do For Ulcerative Colitis
Drink Plenty Of Water
Drinking a glass of water about half an hour before meals can help people feel fuller and eat fewer calories. People who drink water before meals may lose up to 44% more weight than people who do not, according to an older study from 2009.
This habit is also beneficial because it is crucial for people with UC to stay hydrated due to the loss of fluids from diarrhea.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: How To Heal Ulcerative Colitis With Food
How Is Fever Treated
General advice for a fever is to drink plenty of fluids. Do not bundle up with extra layers of clothing or bedding. This can cause your temperature to rise higher. Set the room to a comfortable temperature.1
Acetaminophen may be a better option than ibuprofen for treating a fever.10 There is concern that taking ibuprofen could worsen a IBD flare. Ask your health care provider what type of over-the-counter medications you should take for a fever.
Fever plus bloody diarrhea, pain, abdominal swelling, rapid heart beat, dehydration, or low urine output could be serious. These are symptoms of toxic megacolon, a rare but life-threatening complication of Crohns disease and ulcerative colitis. If you have these symptoms, seek medical care right away.
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
You May Like: Can I Donate Blood If I Have Ulcerative Colitis