What Is A Pressure Ulcer
A pressure ulcer is a break in the skin caused by unrelieved pressure. It can also be described as an area of tissue damaged or killed due to prolonged and intense contact with a hard surface, such as when someone lies down for too long without changing position.
- Prevent moist wound bed
- Provide oxygen to the pressure ulcer by keeping it exposed to air
- Treat underlying medical or surgical condition that caused the pressure ulcer
- Prevent excessive weight bearing on wounds
- Take good care of skin surrounding injured area
- Modify environment around the patient to prevent skin breakdown
What Are The Elements Of A Comprehensive Care Plan For Effective Prevention Or Pressure Injuries
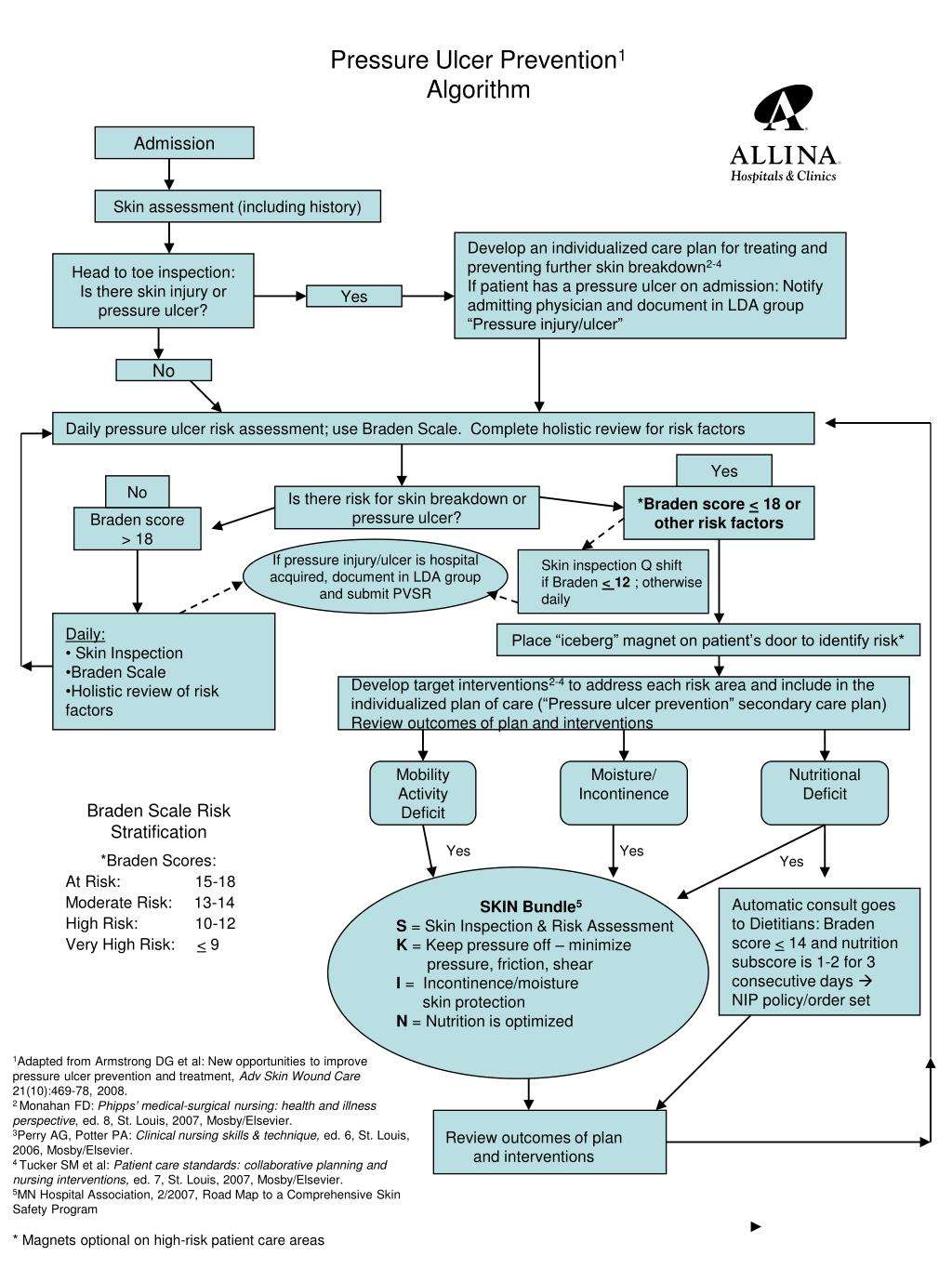
Effective prevention of pressure injuries depends on a comprehensive care plan that includes strategies and practices aimed at reducing or eliminating the risk of these injuries. Elements of such a plan may include the following:
References
National Pressure Ulcer Advisory Panel announces a change in terminology from pressure ulcer to pressure injury and updates the stages of pressure injury. National Pressure Ulcer Advisory Panel. Available at . April 13, 2016 Accessed: June 10, 2018.
NPUAP pressure injury stages. National Pressure Injury Advisory Panel. Available at . April 2016 Accessed: March 26, 2020.
Woolsey RM, McGarry JD. The cause, prevention, and treatment of pressure sores. Neurol Clin. 1991 Aug. 9:797-808. .
Abrussezze RS. Early assessment and prevention of pressure ulcers. Lee BY, ed. Chronic Ulcers of the Skin. New York: McGraw-Hill 1985. 1-9.
Schweinberger MH, Roukis TS. Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg. 2010 Jul-Aug. 49:340-7. .
Pieper B, ed. Pressure Ulcers: Prevalence, Incidence, and Implications for the Future. Washington, DC: National Pressure Ulcer Advisory Panel 2013.
All Ages: Care Planning
-
Develop and document an individualised care plan for neonates, infants, children, young people and adults who have been assessed as being at high risk of developing a pressure ulcer, taking into account:
-
the outcome of risk and skin assessment
-
the need for additional pressure relief at specific at-risk sites
-
their mobility and ability to reposition themselves
-
other comorbidities
-
patient preference.
You May Like: How Can Ulcers Be Treated
Skin Integrity Nursing Care Plans
-Provide the patient with a scheduled play, pain management, and device change.
-Upon noticing the presence of redness or changes in skin temperature, notify the charge nurse immediately. This is to prevent further breakdown and eliminate serious complications such as infection.
-Adjust bed height or reposition the patient to prevent further pressure on the area.
-Assess precautions/contraindications: Review updated physician orders, laboratory and diagnostic studies, and current medication.
-Identify and eliminate/minimize the risk of exposure: Use standard precautions as appropriate for all patients, including transmission-based precautions when indicated.
Protect exposed areas from further damage: Use protective devices such as skin barriers or glove powder to reduce friction during patient repositioning and transfers.
-Instruct patient/family of home care to include:
Daily inspection for proper wound dressing and possible signs or symptoms of infection.
Change bandages as needed to maintain the integrity of the skin edges.
Keep wound area clean and dry. Use hydrogel dressings as ordered and according to the manufacturers recommendation.
Educate on the need to provide adequate nutrition and enough fluids for hydration to the patient.
We also have care plans for Cellulitis
Get the following premium features for free after ordering a custom nursing assignment from us:
- Formatting
Monitor the patients skin daily to ensure proper hygiene.
Ethics Approval And Consent To Participate
Initially ethical clearance was obtained from Addis Ababa University, College of Health Sciences, Department of Nursing and Midwifery Research Review Ethical Committee, and Addis Ababa Regional Health Bureau Ethical Clearance Committee for four hospitals includedin the study to obtain participants in each hospitals. The sixth hospital is teaching hospital administered by Addis Ababa University. These findings were part of a research titled An assessment Nurses knowledge, attitude and practice towards pressure ulcer prevention in admitted patients in Public referral hospitals in Addis Ababa. Permissions to obtain participants secured from each hospital medical directors, matrons and head nurses for the research to be undertaken at each hospital. The anonymity of the participants was respected. The names of the participants were not mentioned to keep the confidentiality. A signed written consent was obtained from participants before participation.
Also Check: Ulcers In Small Bowel Crohn’s
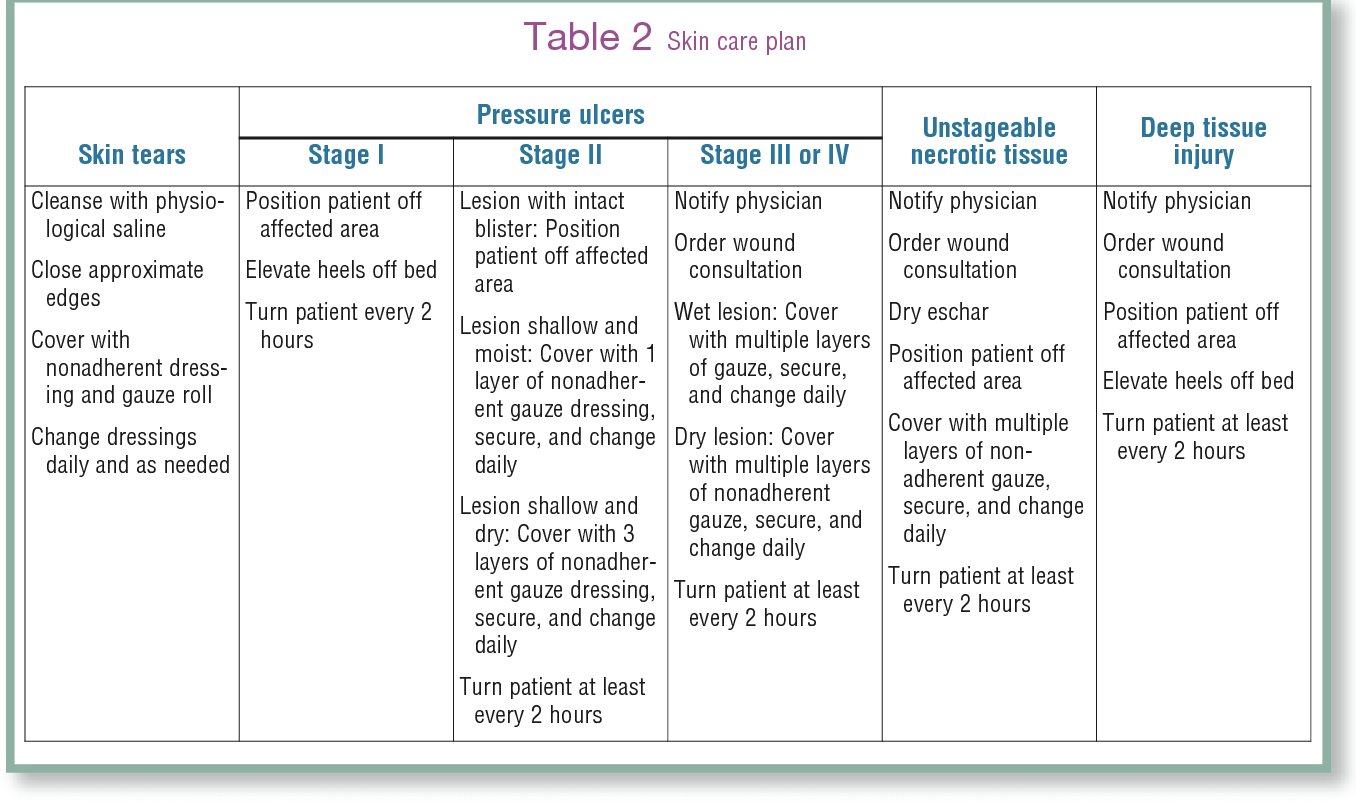
Plan Of Care Synopsis: F Intervention To Prevent Pressure Ulcers
If the physician-ordered Plan of Care includes planned clinical interventions to reduce pressure on bony prominences or other areas of skin at risk for breakdown, select Yes.
Planned interventions include teaching on frequent position changes, proper positioning to relieve pressure, careful skin assessment and hygiene, use of pressure-relieving devices such as enhanced mattresses, etc.
If the clinician completed a formal or informal assessment that indicated the patient is not at risk for pressure ulcers, select NA . If more than one pressure ulcer risk assessment was completed by the assessing clinician, all must be negative in order to select NA.
Resources Created By Dads
- Pressure Ulcer Prevention and Management Care Plan Process identifies the key components of a resident-centered care plan for preventing and managing pressure ulcers.
- Pressure Ulcer Care Plan Teaching Tool can assist facility staff in developing individualized care plans for preventing and managing pressure ulcers.
Don’t Miss: How To Check A Horse For Ulcers
Gi Bleed Nclex Review
To view this video please enable JavaScript, and consider upgrading to a web browser thatsupports HTML5 video
There are different stages of decubitus ulcers in terms of severity. Not all stages of decubitus ulcers present with open sores. The National Pressure Injury Advisory Panel has coined that the most appropriate term should be pressure injuries.
Problems on mobility, poor nutrition, among others, predispose patients in having this condition.
Signs And Symptoms Of Decubitus Ulcer
The general clinical manifestations of decubitus ulcers include:
- Unusual skin color or texture discrepancies
- Erythema or redness
- Edema or swelling in the affected area or limb
- Discharges foul in odor, can be fluid or pus-filled
- Warm or cold to touch An area of the affected region that feels different to touch than surrounding areas
- Tenderness and pain on site
Don’t Miss: Best Ulcerative Colitis Diet Book
Study Setting And Sample
The study was in Addis Ababa, the capital city of Ethiopia which contains 13 public referral hospitals . There are 34 private hospitals, 86 health centers and various NGOs and health institutions. The data in this study included nurses working from patient admission units in six randomly selected public referral hospitals . The units included were medical, surgical, orthopedics, intensive care unit, gynecology, pediatrics, dermatology, burn and oncology.
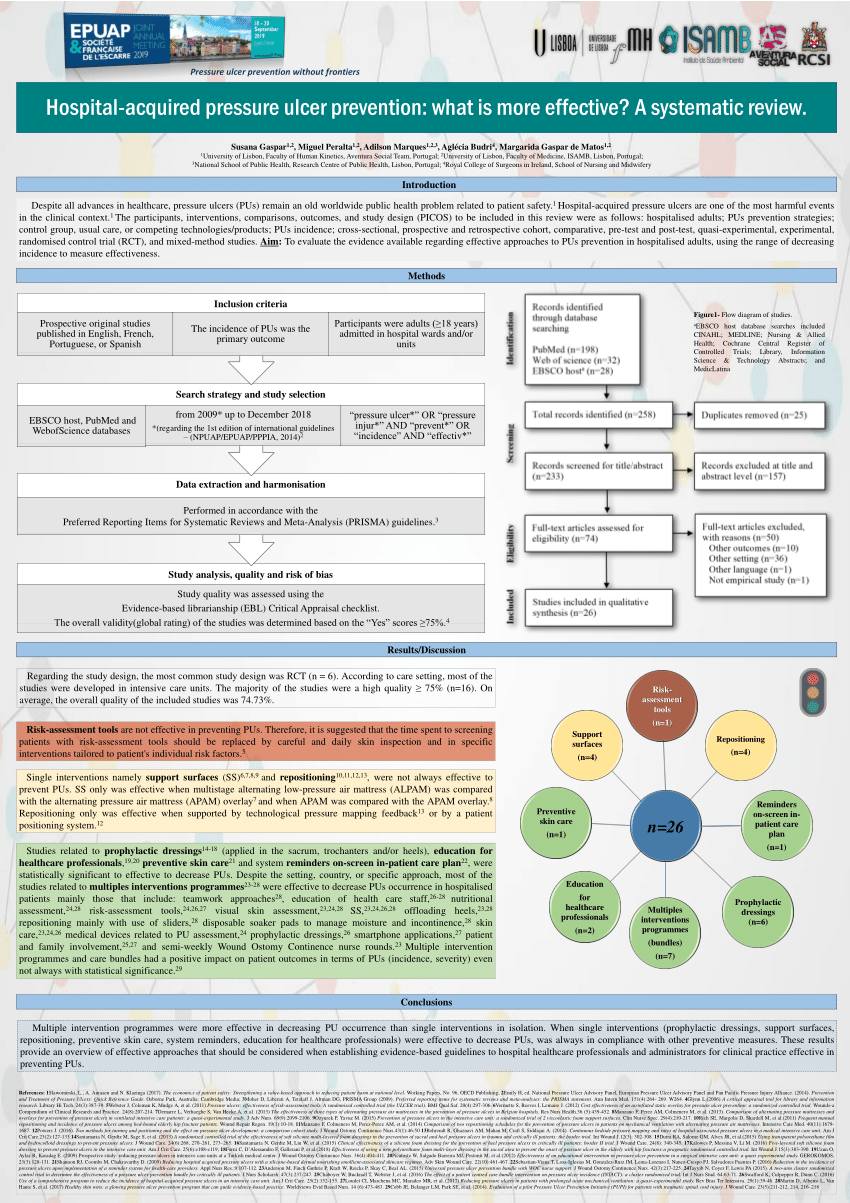
What Additional Resources Are Available To Identify Best Practices For Pressure Ulcer Prevention
A number of guidelines have been published describing best practices for pressure ulcer prevention. These guidelines can be important resources to use in improving pressure ulcer care. In addition, the International Pressure Ulcer Guideline released by the National Pressure Ulcer Advisory Panel and the European Pressure Ulcer Advisory Panel is available. A Quick Reference Guide can be downloaded from their Web site at no charge.
Resources
Clinical Practice Guideline 3: Pressure ulcers in adults: prediction and prevention. Rockville, MD: Agency for Healthcare Policy and Research May 1992. AHCPR Pub. No. 92-0047. Archived at: .
Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. J Spinal Cord Med 2001 Spring 24 Suppl 1:S40-101.
National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel . Quick Reference Guide version of the NPUAP/EPUAP International Pressure Ulcer Prevention Guidelines: Available at: and .
The following guidelines are available for a fee:
American Medical Directors Association: Pressure Ulcers in the Long-Term Care Setting. Available at: http://www.amda.com
Read Also: What Are The First Signs Of A Stomach Ulcer
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
Nursing Care Plan For Impaired Skin Integrity
Nursing care plan for impaired skin integrity : The nursing care plan template below includes the following conditions: Impaired Skin Integrity, Risk for Skin Breakdown, Altered Skin Integrity, and Risk for Pressure Ulcers.
What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing care plan?
This care plan is listed to give an example of how a Nurse may plan to treat a patient with those conditions.
Important Disclosure: Please keep in mind that these care plans are listed for Example/Educational purposes only, and some of these treatments may change over time. Do not treat a patient based on this care plan.
Care Plans are often developed in different formats. The formatting isnt always important, and care plan formatting may vary among different nursing schools or medical jobs. Some hospitals may have the information displayed in digital format, or use pre-made templates. The most important part of the care plan is the content, as that is the foundation on which you will base your care.
Read Also: Best Way To Treat Mouth Ulcers
Resources From Other Organizations
- Prevention Plus provides services and products related to the Braden Scale for Predicting Pressure Ulcer Risk and evidence-based programs for pressure ulcer prevention.
- The Bates-Jensen Wound Assessment Tool is a validated and reliable tool for conducting in-depth evaluations of wound status. The BWAT is available on this website, along with concise instructions for using the tool.
- The National Pressure Ulcer Advisory Panel is a professional organization dedicated to the preventing and managing pressure ulcers.
- The PUSH Tool 3.0 is a validated and reliable tool that is used to collect data and monitor the healing of pressure ulcers.
Sample Size And Sampling Procedure
The sample size was determined using a formula of estimating a single population proportion for cross sectional study. Since the population size is less than 10, 000 , the final sample size was estimated using correction formula. The final sample size obtained including 10% non-response rate was 252. Then, the number of participants in each selected hospitals to obtain similar proportion of participants were determined using the population proportionate sampling . It is estimated using the formula: n=/N total, where, n=Proportion of nurses participate in the study in a given public hospital, nf=Final sample size obtained using correction formula , N=is the total number of nurses in the selected public hospitals .
Also Check: Ulcerated Nodular Basal Cell Carcinoma
Nursing Diagnosis Impaired Skin Integrity Related To Pressure Ulcer
Ineffective peripheral Tissue Perfusion Pressure Ulcers occur when skin is in prolonged contact with an underlying bony prominence or other fixed objects. This can be due to improper positioning or activity restrictions. They are usually more severe than stage I and II pressure ulcers and can be dangerous if not treated properly. Pressure Ulcers are open wounds and should be cleaned regularly with mild soap, rinsed with clean water, and dried thoroughly.
Treatment For Pressure Ulcers
The ulcers are treated with methods that promote wound healing and prevent further damage, such as
-Preventing deep or prolonged contact with a hard surface. This is done by using a unique cushion called an air body or air mattress. This helps maintain position, prevent shearing and improve circulation to the wound site.
-Removing or repositioning any objects in contact with the ulcer, such as clothing or sheets.
-Lifting extremities for bedridden patients. A unique tool called the McRoberts maneuver can raise a leg while the patient is lying on their back. This will help prevent pressure from being placed on that area and allow it to heal.
-Turning/repositioning bed-bound patients every two hours if possible. If not, reposition as often as possible for the patient.
-Prompt treatment of any skin breakdown with a topical or local wound-care product that will protect the skin from further damage.
You May Like: Support Surfaces For Pressure Ulcer Prevention
Home Health Care Best Practices: M2250 Pressure Ulcer Care Plan
Posted byJoy Joan E. De Castro, RN, MSN on Jan 31, 2017
For the patient with and/or at risk for pressure ulcers, in addition to assessing M2250 Pressure Ulcer care and prevention on OASIS C home health care forms, also include these MyHomecareBiz Best Practice assessment strategies:
1. Determine the clients general condition of the skin.2. Assess the clients nutritional status, including weight, weight loss, and serum albumin levels, if indicated.3. Assess the clients awareness of the sensation of pressure.4. Assess for fecal and urinary incontinence.5. Assess patients mobility. 6. Assess for environmental moisture .7. Assess the amount of shear and friction on the clients skin.8. Assess the surface that the clients spend a majority of time on .9. Assess the skin over bony prominences .10. Perform pressure ulcer risk assessment: Braden scale, Norton scale.11. Assess the clients level of pain, especially related to dressing change and procedures.12. Assess and stage the pressure ulcers.
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Also Check: Over The Counter For Ulcers
Neonates Infants Children And Young People: Risk Assessment
-
Carry out and document an assessment of pressure ulcer risk for neonates, infants, children and young people:
-
being admitted to secondary care or tertiary care or
-
receiving NHS care in other settings if they have a risk factor, for example:
-
significantly limited mobility
-
significant loss of sensation
-
a previous or current pressure ulcer
-
nutritional deficiency
-
the inability to reposition themselves
-
significant cognitive impairment.
Demographic Characteristics Of The Nurses
A total of 252 professional nurses were invited to participate in the study, 222 fully participated in the study, for a response rate of 78.7%. Among 369 nurses 128 were males. The mean ages of participants were 29 with minimum 20 and 61 years maximum. Most participants had a bachelors degree in , while 11% were enrolled in masters of Science degree in nursing. Nurses who are counted for their experiences in more than 10 years were 20.2% while majority of them 54% have 14 years of experience in nursing profession. Sixteen nurses reported that they had received and the largest proportion of them never received any training in PU prevention, while majority of them had not previously read research articles about PU compared to 31 who had read it. A limited number of nurses had attended PU training on conference. The majority of the participants were from medical ward as shown in Table .
Table 1 Frequency distribution of nurses socio-demographic variables
Read Also: Do Stomach Ulcers Cause Nausea
What Items Should Be In Our Bundle
The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines .
Action Steps
Identify your bundle of best practices.
3.5.1 How do we customize the bundle for specific work units?
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.3.5.
Action Steps
- Identify the units that will require customization of the skin and risk assessment protocols.
- Modify the bundle, the assignment of roles, and the details of the unit to meet these special features.
Additional Information