Conditions We Treat: Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease in which the inner lining of the large intestine and rectum become inflamed. Ulcerative colitis is characterized by diarrhea, abdominal pain and blood in the stool. The disease may vary in how much of the colon is affected, and it varies in severity as well.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Advanced Approach To Managing Ulcerative Colitis
Every patient treated by the digestive health team receives the best quality care from our multidisciplinary approach to ulcerative colitis treatment. The key to improved care lies in our collaboration, communicating between specialists, so an entire team is a part of decisions for the management of each patients condition.
We offer a wide variety of leading-edge therapies to both control the disease and prevent complications. With advanced immunomodulator and biologic therapies available for ulcerative colitis, patients should expect a near normal daily life. These more advanced therapies control inflammation by decreasing your bodys immune response and target specific proteins identified with inflammation. Given as daily medications or injections, well work together to determine the best course of treatment.
State-of-the-art infusion services to treat ulcerative colitis are available at UH Specialty Clinic Infusion Center in Warrensville Heights.
Our goal is to minimize disease-related ulcerative colitis symptoms and allow people to live well with this disease that can many times disrupt life.
Don’t Miss: What Foods Not To Eat If You Have An Ulcer
Medications For Ulcerative Colitis
No medicine can cure UC. The goal of medication is to make a patients ulcerative colitis manageable. People with UC may have to take medicines indefinitely to control their condition.
Medications for treating ulcerative colitis:
- Aminosalicylates
- These medications may be used in people with mild or moderate symptoms and most people can tolerate them. They contain an active ingredient called 5-aminosalisylic acid, or 5-ASA, which helps control inflammation. Drugs in this class include balsalazide, mesalamine, olsalazine and sulfasalazine.
- Corticosteroids
- More commonly known simply as steroids, these medicines reduce the immune systems response. They are used if aminosalicylates dont seem to work. Drugs in this class include prednisone, methylprednisone, hydrocortisone and budesonide. These drugs shouldnt be used long-term.
- Immunomodulators
- These drugs reduce immune system activity as well, but may take as long as three months to work. Immunomodulators include Azasan or Imuran and Purinethol or Purixan .
- Biologics or TNF therapy
- This group includes Humira , Simponi and Remicade , medications that decrease inflammation by targeting a protein made by the immune system called tumor necrosis factor, or TNF. Side effects of these medications include higher risks for tuberculosis, fungal infections, skin cancer and psoriasis.
Doctors may also recommend antibiotics to prevent infection and other medications to treat diarrhea.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Recommended Reading: Do Stomach Ulcers Cause Nausea
Of Digestive Health Center
Leaders in IBD Treatment
Our world-class doctors are passionate about taking care of people with IBD. We provide expert IBD care in a unique, multi-specialty Digestive Health Center, with the goal of bringing about disease remission. We offer leading-edge treatment options based on the latest research, while continuing to explore new trial therapies, to help you lead a full, active life.
420 Broadway Street
Ibd Symptoms And Risks
While the exact causes of IBD are unknown, it is important to recognize the risk factors. IBD affects men and women equally and tends to run in families.
It is important to meet with an experienced IBD specialist to obtain an accurate diagnosis. IBD experts evaluate patients with chronic diarrhea and abdominal pain to identify possible IBD. They will run a series of investigations to arrive at an accurate diagnosis.
You should visit your healthcare provider and IBD specialist if you have:
- Abdominal pain or cramping
- An urgent need to have a bowel movement or the feeling that a bowel movement is incomplete
- Constipation
- Weight loss
Don’t Miss: How To Tell Stomach Ulcer
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Understanding Ulcerative Colitis Risk Factors
Several factors can contribute to your risk of ulcerative colitis, including what you can control such as diet and lifestyle and what you cannot control such as age and genetics. The most common risk factors for ulcerative colitis include:
- Age: Ulcerative colitis usually begins before age 30 or people may develop UC at any age.
- Race or ethnicity:Caucasians have the highest risk of UC although anyone of any race can get it. People of Ashkenazi Jewish descent have an even higher risk of UC.
- Genetics: People with a family history of ulcerative colitis are at higher risk of UC .
- Environmental factors: Reacting to substances within the environment such as bacteria or chemicals may trigger uncontrolled inflammation in the gastrointestinal tract.
- Diet and Lifestyle: While less common risk factors for ulcerative colitis, increased consumption of polyunsaturated fatty acids may contribute to issues with digestive health. In addition, a sedentary lifestyle or smoking are also risk factors for overall health which contribute to your gastrointestinal health.
You May Like: Best Ulcerative Colitis Diet Book
If You Need An Ulcerative Colitis Diagnosis
If you are experiencing some of the signs and symptoms of ulcerative colitis , your first appointment should be with your regular healthcare provider. Ideally, this person will already know your medical history and be able to evaluate your symptoms in context. General physicians, including internists and family physicians, are all qualified to perform a full physical exam, including a rectal exam, if necessary.
If, after a conversation and physical examination, your healthcare provider thinks your colon or intestine is a probable source of your symptoms, he or she will probably refer you to a gastroenterologist or for a colonoscopy, a medical test that allows healthcare providers to see the inside of your colon.
Diagnosing And Treating Ulcerative Colitis
There are four ways to diagnose ulcerative colitis. It is usually treated through medications or surgery.
How ulcerative colitis is diagnosed:
- A review of the patients family history of UC
- Physical exam to check for swelling, listen for sounds in the abdomen, and check for tenderness or pain in the abdomen
- Lab tests of blood and stool that check for anemia, inflammation elsewhere in the body and other markers common to UC patients
- Use of an endoscope, a long, flexible tube with a camera, to look at the colon
: National Institutes of Health
Treatment options depend on the severity of the patients ulcerative colitis. Surgery may require removing the colon and rectum in the most severe cases.
Recommended Reading: How Do You Cure Mouth Ulcers
Homeopathy Medicines For Ulcerative Colitis
The common Homeopathy medicines that our specialists have prescribed for ulcerative colitis at our clinics over the last 18 years are
SILICEA , PHOSPHORUS, COLCHICUM, TEREBENTHINA, MERCURIUS , ARSENIC, ALUMINA , SULPHUR, THUJA, AND NITRIC ACID.
Meet our specialists at any Welling Clinic or consult online to know about your custom-made Homeopathy medicines for ulcerative colitis and get started with your Homeopathy treatment for ulcerative colitis.
What Is Ulcerative Colitis
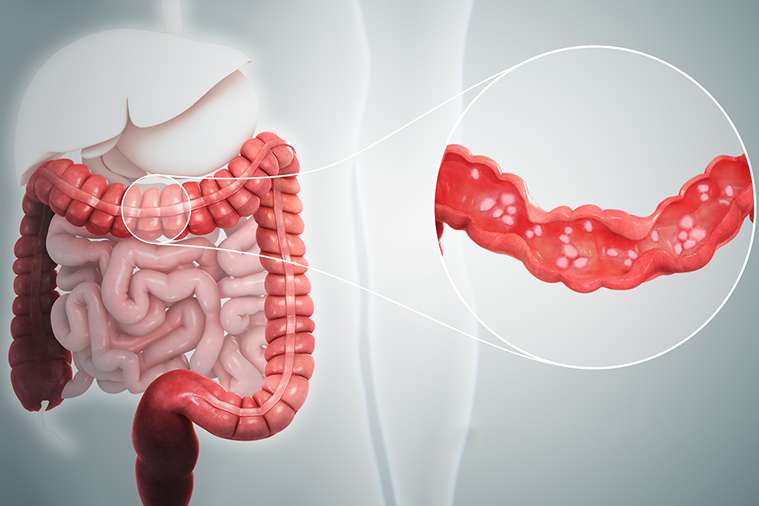
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
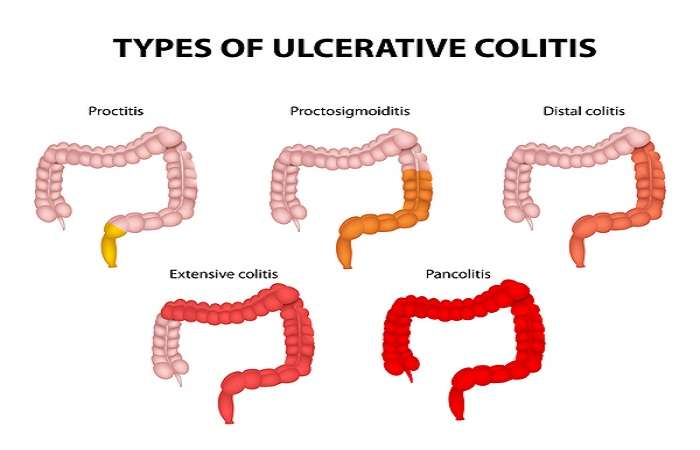
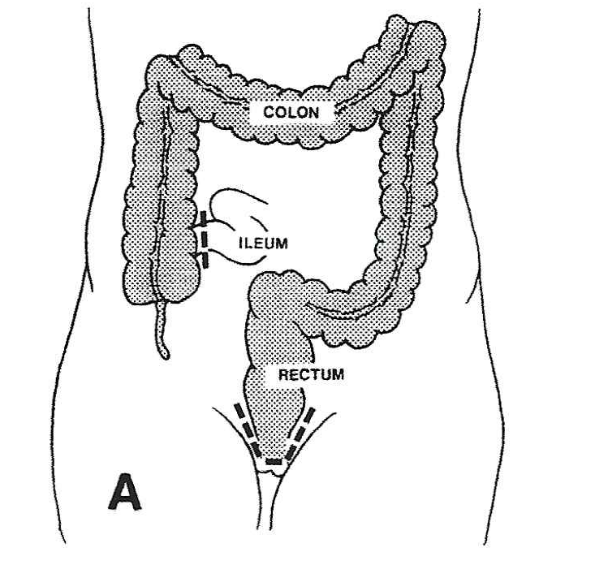
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
You May Like: How To Cure Ulcerative Proctitis
What We Offer You For Ibd Care
- Specialized expertise for all forms of IBD, including complex forms of Crohn’s disease, ulcerative, microscopic and collagenous colitis, and pouchitis. We also treat conditions that can accompany IBD and complications from longstanding disease. Go to Conditions Treated
- Advanced treatment options that may include combination treatment plans encompassing the latest medical treatments, nutritional optimization, endoscopic therapies, and minimally invasive surgeries to improve your quality of life. Go to Treatments
- Team-based approach that combines the expertise of IBD gastroenterologists, colorectal surgeons, pathologists, radiologists, pharmacists, and other specialists to tailor care to your needs. Go to Your Care Team
- Clinical trials for Crohn’s disease and ulcerative colitis from one of the strongest IBD research programs in the U.S. Go to Clinical Trials
- Comprehensive support services such as reproductive health and family planning for people with IBD, psychological support, transition from pediatric IBD care, and nutritional guidance. Go to Support Services
- Easy Access to care at our Redwood City location, where you can get comprehensive treatment and see multiple specialists during the same day to address other common conditions associated with IBD. Go to Accessing Care
Specialist Nutritionist And Dietary Care
We provide all patients with the opportunity for consultations with nutritionists with significant experience in the management of gastrointestinal illnesses. Patients are encouraged to discuss ways of maintaining and building up their nutritional status and correcting vitamin deficiencies while keeping symptoms under control. They can also work with the nutritionists to identify and eliminate potential dietary triggers of their symptoms.
You May Like: Best Treatment For Diabetic Foot Ulcer
Diagnosing Inflammatory Bowel Disease
To diagnose Crohns disease or colitis, we start with a comprehensive examination and collecting a thorough history. A number of tests are needed to confirm diagnosis. They may include:
- Colonoscopy and flexible sigmoidoscopy: Used for initial diagnosis, both use a thin, flexible tube with camera to examine different areas, including the colon, small intestine and large intestine to see any ulcers, bleeding and inflammation.
- Upper endoscopy: Uses a thin, flexible tube with camera inserted through the mouth, following the tract to the stomach and upper small intestine to look for bleeding, ulcers and inflammation.
- Capsule endoscopy: A capsule containing a camera is swallowed by the patient to take pictures along the digestive tract not easily reachable by other procedures .
- Laboratory tests: Blood work plus stool samples to check for bacteria and intestinal bleeding.
- CT interography and MR interography: Specialized radiology tests that evaluate the small intestine, an area of the gastrointestinal tract that is beyond the reach of colonoscopy and upper endoscopy, but is often where Crohns disease is present.
- Imaging tests: Collaborating with experts in Radiology for imaging and interpreting gastrointestinal abnormalities, including abdominal x-rays, barium enema, computed tomography , fistulogram and MRI.
Comprehensive Care For All Types Of Ibd
UT Southwestern Medical Centers inflammatory bowel disease team is led by gastroenterologists who have specific expertise in the diagnosis and treatment of chronic inflammatory conditions of the intestines, including Crohns disease, ulcerative colitis, and microscopic colitis.
Among the conditions we routinely help manage are:
- Crohns disease, including ileal, colonic, perianal, and upper GI
- Ulcerative colitis
- Fistulas in the GI tract
- Colonic dysplasia
- Pouch disorders/pouchitis
- Lymphocytic colitis
- Short bowel syndrome
We often collaborate with specialists in other areas of expertise, including colorectal surgery, radiology, liver disease, interventional endoscopy, pancreaticobiliary disease, dermatology, rheumatology, and motility disorders, in order to provide comprehensive care. To best treat our patients, we also hold regular monthly multidisciplinary case conferences to discuss particularly challenging cases. We also have several clinic trials in which we can enroll patients with IBD.
Don’t Miss: How To Heal Leg Ulcers Quickly
Diagnosis Of Ulcerative Colitis
The best test for diagnosis of ulcerative colitis remains sigmoidoscopy to see inner nature of the lining of the colon and the rectum.
While performing of endoscopy the physician can see the vasculature , ulceration and any out-growth like polyps.
The physician may elect to limit the extent of the exam if severe colitis is encountered to minimize the risk of perforation of the colon. Usually in serve cases it not performed to limit the spread of the disease.
Blood investigations are also performed to know the general health status
- CBC
- Stool culture, to rule out parasites and infectious causes.
- Erythrocyte sedimentation rate
- CRP
Inflammatory Bowel Disease Center
U.S. News & World Report
At NYU Langones Inflammatory Bowel Disease Center, our renowned experts provide advanced treatment and care for adults who have inflammatory bowel disease , including Crohns disease and ulcerative colitis.
Our care team offers a range of specialized services, including gastroenterology, surgery, nutrition, ostomy care, and psychosocial care in one convenient, dedicated space.
Clinical Trials
Our mission is not only to make an accurate diagnosis and offer the most advanced treatment options, but also to care for the whole person.
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
How To Treat Ulcerative Colitis
Surgery for ulcerative colitis involves removing the colon and rectum. Often a new rectum is constructed from small intestine and the patient will not require a permanent ostomy bag. This surgery is frequently done in a minimally invasive fashion, using a laparoscopic or robotic approach and small incisions to lessen discomfort and hasten recovery. The surgeons at Piedmont Colorectal Associates have extensive experience in treating ulcerative colitis and can help to decide the best approach for each patient.
Research And Clinical Trials: Advancing Care Of Crohn’s Disease And Ulcerative Colitis Through Cutting
At the Mass General Crohn’s and Colitis Center, we believe in integrating outstanding clinical care with cutting-edge research to offer answers that address the needs of our patients and advance scientific understanding of these complex diseases. We believe that every patient can significantly improve our knowledge of Crohn’s disease and ulcerative colitis, contribute understanding the factors that influence the development of these diseases, behavior of the disease and response to treatments. All of our physicians at the Crohn’s and Colitis Center are actively involved in research programs aimed at understanding the underlying cause of Crohn’s disease and ulcerative colitis, with the goal of developing more effective therapies and improve in our quality of life.
Interested patients can participate in research through enrollment in our ongoing patient registries, enroll in clinical trials of novel therapies, or participate in studies aimed at developing new treatment strategies including harnessing the dietary, lifestyle, and behavioral changes in the management of these diseases.
Don’t Miss: How To Test For Ulcerative Colitis
Treatments For Ulcerative Colitis
Although there is no cure for ulcerative colitis, effective therapies for chronic treatment and management of this condition are now available, which has drastically altered the diseases natural history. Medicines, particularly biological therapies, can help reduce symptoms significantly and even provide long-term remission.
Ulcerative colitis treatment options include:
- Combination of 5 ASA drugs for anti-inflammatory properties used for mild to moderate ulcerative colitis. 5 ASA drugs provide results in 40% to 80% of patients.
- Immune system suppressors
- Biologic therapies and other modalities
Aminosalicylates are the main treatment choice for mild to moderate ulcerative colitis. You can use topical and systemic steroids to treat ulcerative colitis flares, while immunosuppressants and biological drugs can improve moderate to severe disease.
Surgery is an option if medical therapy fails. Finally, if you have Ulcerative Colitis, you should have more colon cancer screenings because you are at a higher risk of developing colon cancer. Your gastroenterologist should formulate an effective surveillance colonoscopy schedule.
Manhattan Gastroenterologys ulcerative colitis specialists must have a broad understanding of each patients unique factors before devising the best treatment plan. Ulcerative Colitis is not an exception.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Read Also: List Of Foods Good For Ulcers
Why Welling Homeopathy Medicines For Ulcerative Colitis
- The custom-made Homeopathy medicines are effective to cure ulcerative colitis permanently,
- We have helped over 4500 patients recover from ulcerative colitis from 1o8 countries,
- If you start early, we can prevent complications of ulcerative colitis,
- Being one of the largest online and in-clinic Homeopathy practice in the world, our experience in managing ulcerative colitis patients can help you get assured results of the treatment,