Selecting The Right Dressing For Sacral Ulcer Management
A tremendous number of dressings are available for different types of wounds, and variousguidelines are available to help wound care professionals determine which type of dressing should be used in various circumstances. For example, petrolatum-impregnated dressings are nonadherent dressings that are useful in wounds with minimal exudate. Conversely, alginates and hydrofiber are moderately or highly absorbent, respectively, which makes them useful in wounds with excessive exudate production.
How To Measure A Sacral Wound
Learn about how to stage and treat this type of ulcer. The scale assesses levels of sensory perception, moisture, activity, mobility, nutrition, and friction.
Pressure Ulcer Stage Iv Pressure Ulcer Classifications
Postoperative And Rehabilitation Care
Postoperative care of patients who have undergone reconstructive surgery is of utmost significance as these ulcers have high rates of recurrence. A study done on characteristics of recurrent pressure ulcers showed that patients who underwent reconstructive surgery and developed post-operative, had an 11% to 19% chance of recurrence. Those without any postoperative complications had recurrence as high as 61%.
When medical staff shift patients from the operating table to their air-fluid beds, they must avoid excessive shearing, and stretch on skin flaps. For the first four weeks, patients are positioned flat on their support surfaces, after which they can place themselves in a semi-sitting position. The patient starts to sit for 10 minutes only after six weeks of the surgical procedure. After these sitting periods, the flap should be examined for discoloration and wound edge separation. Over two weeks, the sitting periods will increase to 2 hours in 10-minute increments. Patients will also learn to lift for 10 seconds every 10 minutes to relieve pressure. Meticulous skincare is necessary.
Recommended Reading: Snack Ideas For Ulcerative Colitis
Management Of Sacral Ulcers Varies By Ulcer Stage
It is important to properly stage pressure ulcers for several reasons, but two of the most important are for prognosis and management planning. Stage 1 and stage 2 pressure ulcers heal by regenerating tissue in the wound. Stage 3 and stage 4 pressure ulcers, on the other hand, heal through scar formation, which means the borders of the wound contract as it heals.
For Stage 1 sacral ulcers, the primary goal of therapy is to ensure adequate tissue perfusion and to protect the wound from further damage.2 This means preventing the sacrum from chronically squeezing the skin and preventing blood flow to the area. The goal of therapy for Stage 2 ulcers is to encourage tissue regeneration and protect the wound surface. For stage 3 or 4 ulcers, management efforts are focused on promoting tissue granulation and epithelialization.
Sacral Decubitus Ulcers Are A Certain Type Of Wound Located On The Lower Back At The Bottom Of The Spine

How to measure a sacral wound. Clock terms can also be used to describe the location of undermining. Use the body as a clock when documenting the length, width, and depth of a wound using the linear method. The braden risk assessment scale can be utilized to assess a patient’s risk of developing a pressure ulcer.
Get the wound depth using a cotton pledget or applicator dipped in a normal saline solution to measure the deepest part of the wound bed. Look closely at the wound and its edges, and then draw the wounds shape. Measure the wound how to measure wound size consistency is key.
Any adult who scores lower than 18 on the braden scale is high risk. For example, you might use words like jagged, red, puffy, or oozing to describe the wound.step 2, use a ruler to measure the length. Remove the applicator and hold it against the ruler to measure the depth of the wound margin based on.
This is particularly important when The total amount of tissue debrided should be listed separately from the wound measurements The six approaches for measuring wound area were simple ruler method , mathematical models , manual planimetry , digital planimetry , stereophotogrammetry and digital imaging method .
Step 1, draw the shape of the wound and write a brief description. Assessing and measuring wounds you completed a skin assessment and found a wound. In all instances of the linear method, the head is at 12:00 and the feet are at 6:00.
Archives Of Plastic Surgery
Pressure Ulcer Chart Lhsc
Also Check: What Is A Good Diet For Ulcers
Pressure Ulcer Nursing Care Plans
A pressure ulcer is a localized skin injury where tissues are compressed between bony prominences and hard surfaces such as a mattress. They are caused by pressure in combination with friction, shearing forces, and moisture. The pressure compresses small blood vessels and leads to impaired tissue perfusion. The reduction of blood flow causes tissue hypoxia leading to cellular death.
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
Don’t Miss: Artificial Sweeteners And Ulcerative Colitis
Pressure Ulcer Of Sacral Region Stage 4
- 2016201720182019202020212022Billable/Specific Code
- L89.154 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.154 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.154 – other international versions of ICD-10 L89.154 may differ.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
- Applicable To annotations, or
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- Sepsis may occur when the body overreacts to a serious infection, such as an infection stemming from a stage 4 bedsore. The immune system gets overstimulated and attacks healthy body parts. Severe cases of sepsis can lead to septic shock, which occurs when blood pressure drops due to an infection. Septic shock can be deadly as major organs may shut down.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
Don’t Miss: What To Eat If You Have Gastric Ulcer
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Also Check: What Does An Ulcerative Colitis Flare Up Feel Like
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Diagnosing A Stage 4 Bedsore
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Also Check: Chances To Win Social Security Disability With Ulcerative Colitis
Whos At Risk Of Stage 4 Bedsores
Anyone with a lower-stage bedsore is at risk of a stage 4 sore. However, some patients may be more prone to this type of injury.
At particularly high risk are those:
- With Limited MobilityMovement is the key to preventing bedsores of any stage. If an older person cannot move on their own, they may sit or lie in the same position for hours. This can cut off blood flow to their skin and cause a bedsore.
- Who Are In Understaffed Nursing HomesNursing home residents with mobility issues must rely on staff members to prevent bedsores. Sadly, some care facilities may fail to prevent bedsores due to issues like understaffing and poor training.
- Who Have Alzheimers or DementiaIf residents with mental impairments develop a bedsore, they might not be able to tell anyone due to their condition. Theyll need to have someone else find it and help them get the proper care. Residents with these conditions may also have trouble sensing pain.
- Other FactorsResidents are at higher risk of bedsores if they have blood flow or circulation problems, diabetes, or poor nutrition or if they wear a cast.
Our trusted advocates can help you and your loved one take legal action. Call us today at .
Stages Of Decubitus Ulcers
Stages of decubitus ulcers are classified from Stage I to Stage IV according to the severity of symptoms.
Stage Iâ In fair-skinned individuals, a defined skin area is characterized by persistent redness. Darker skin may come with hues of red, purple of blue. Compared to the other adjacent body area, the changes in the defined area involve skin temperature, sensation, and palpable or felt tissue consistency. When the define area is pressed, the skin does not turn to whiteâ a key indicator that decubitus ulcer has already started to occur.
Stage IIâ At this stage, the decubitus ulcer is still superficial. A blister, an abrasion, or a shallow crater or open sore has formed the surrounding area of which may appear to be irritated and red in color.
Stage IIIâ The superficial ulcer appears like a deep crater, where thick skin loss involves impairment in the skinâs underlying tissue. The depth of damage may reach the fascia, but does not pass through it.
Stage IVâ Further impairment takes place along with the fully thick skin loss. The depth of damage reaches the bone, muscle, or the supporting tendons and joint capsule. Furthermore, sinus tracts may also characterize Stage IV decubitus ulcers.
Don’t Miss: How Do You Know If You Have A Peptic Ulcer
Info For Medical Coders On How To Properly Use This Icd
- Inclusion Terms:
Inclusion Terms
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
- Healing pressure ulcer of sacral region, stage 4
- Pressure ulcer with necrosis of soft tissues through to underlying muscle, tendon, or bone, sacral region
Deterrence And Patient Education
Patients and their family members should have a clear idea that preventing recurrence requires commitment and responsibility. They should receive education on how to manage the condition in the hospital and as well as in their homes. They should be familiar with warning signs like skin discoloration, ulceration, discharge, or a foul smell from the ulcer site and body areas with decreased or no sensation.
The patient should move or turn every 2 hours it could not be done by themselves, or they should ask someone to help them. Air or water mattress should be used in their homes too. Their food intake should be adequate and should consist of a balanced and healthy diet.
Read Also: Bland Diet Recipes For Ulcers
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
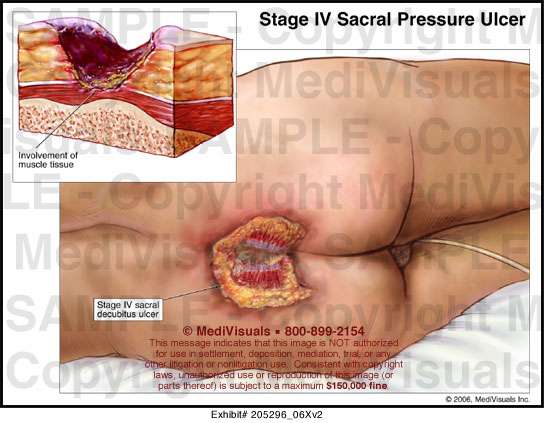
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Don’t Miss: Is Alcohol Bad For Ulcerative Colitis
The Icd Code L89 Is Used To Code Pressure Ulcer
Pressure ulcers, also known as pressure sores, bedsores and decubitus ulcers, are localized injuries to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles or the back of the cranium can be affected.
| Specialty: |