Soothe Symptoms With Salmon
Salmon is rich in omega-3 fatty-acids and eating salmon may help counterbalance the inflammation that occurs during an ulcerative colitis flare, says Torey Armul, RD, a national spokesperson for the Academy of Nutrition and Dietetics and a health coach at Rise Labs, Inc.
Salmon also has protein to provide energy, and many people can tolerate it even during a flare-up, Armul adds.
Albacore tuna, walnuts, flaxseed oil, and ground flaxseed are other good sources of omega-3s.
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.
Can Food Cause Crohn’s Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- Genetics
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Read Also: What Is Good For Mouth Ulcers
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Food Preparation And Meal Planning

While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Recommended Reading: How To Cure Gastritis And Ulcers Naturally
Toasted Potato Bread With Scrambled Eggs And Spinach
Whole-grain foods are a good source of fiber, which normally helps reduce constipation and supports overall health. The high levels of fiber in whole grains may be hard to digest during an ulcerative colitis flare.
Potato or sourdough bread is usually easier to tolerate for people with ulcerative colitis. Top with scrambled eggs for a good source of protein.
Add sautéed spinach for a healthy dose of iron.
Ulcerative Colitis Medications& Surgery
The goal of all ulcerative colitis treatment is to reduce colonic inflammation. The most effective drugs or medicines for this purpose are the salicylates, which are related to aspirin.
When aminosalicylates do not work, corticosteroids are used. A third type of anti-inflammatory drug known as immunomodulators are also used, but it may take weeks or months for these drugs to work.
The latest technology in the treatment of ulcerative colitis is the use of biologic drugs, which target the bodys immune system in order to help heal ulcerative colitis.
Biologic therapy must be given intravenously every few weeks, and involves administering antibodies that are directed at the molecules produced by the immune system that cause inflammation.
Inspired by low incidence of UC in developing countries, there are ongoing clinical studies into the possibility that the pig whipworm may be useful as ulcerative colitis treatment because some scientists theorize that worms in the colon change the immune response and consequently reduce inflammation in the process. 42% of UC patients in one study saw their symptoms improve after eating pig whipworm eggs for three months.
You May Like: How Do They Check For Ulcers
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
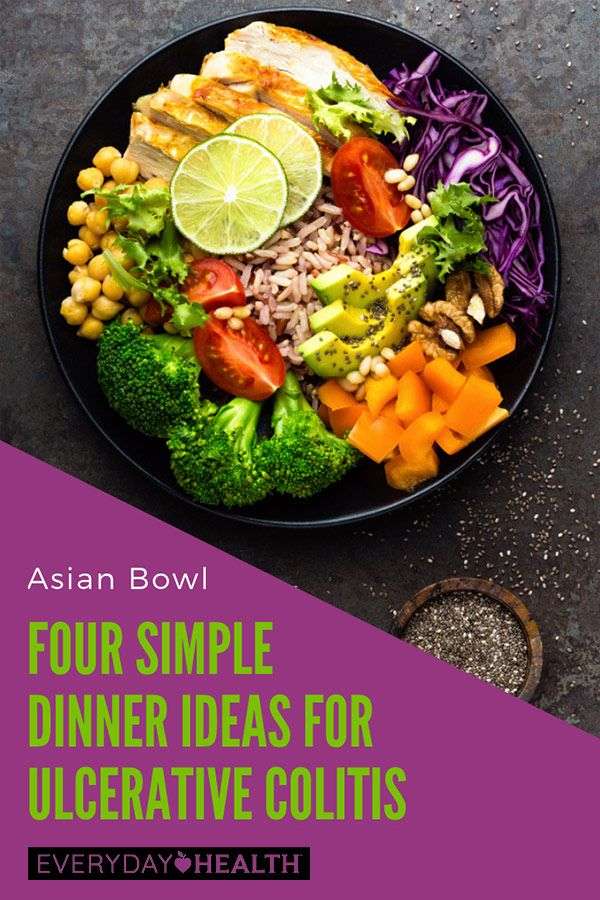
The Best Diet For Ulcerative Colitis
Most experts say that people with UC should simply try to eat a well-balanced diet whenever possible. This should include a variety of foods:
- Lean meat, fish, and poultry
- Low-fat dairy products
- Bread, cereal, and whole grains
- Fruits and vegetables
- Healthy fats such as vegetable oils
Keep a food diary to help you figure out which foods cause problems for you and whether or not you’re getting enough nutrients.
If you lose weight because of your ulcerative colitis, try to eat five or six small meals and snacks during the day instead of two or three large meals.
When you have chronic diarrhea, drink plenty of water or other fluids to stay hydrated.
A dietitian can plan a diet that meets your calorie and nutrient needs. Before you take any dietary supplements, talk to your doctor or dietitian. Find out how to make a diet plan for ulcerative colitis.
You May Like: Remicade Infusion For Ulcerative Colitis
The Ulcerative Colitis Diet Plan: Best And Worst Foods When Living With Uc
If you’re one of the nearly million of Americans living with ulcerative colitis, a type of inflammatory bowel disease, you may be looking for an ulcerative colitis diet that gives you the essential vitamins and nutrients you need but doesnt worsen the inflammation and discomfort that goes with your condition. While food isnt a cure-all for any disease, it can help you minimize your symptoms of ulcerative colitis and boost your overall health. Here is an overview of the best and worst foods to eat when youre living with ulcerative colitis.
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Recommended Reading: How To Check A Horse For Ulcers
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
- Apple sauce
- Herbal or green tea.
What Desserts Can I Eat With Ibs
The Best Low FODMAP Cakes & Cupcakes
- The Best Basic Low FODMAP Yellow Cake.
- Red Velvet Cake with Cooked Vanilla Icing.
- Chocolate Cupcakes.
- Pumpkin Cheesecake in a Gingersnap Crust.
- Flourless Chocolate Cake.
- Low FODMAP Carrot Cake with Cream Cheese Frosting.
- Cinnamon Streusel Coffee Cake.
Read Also: Best Medicine For Ulcerative Colitis
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Worst Foods For Ulcerative Colitis
When living with ulcerative colitis, you may find there are certain foods that cause your symptoms to instantly worsen. For instance, high-fiber options may be difficult to digest and cause more discomfort during a flare-up. Finding foods that are lower in fiber but still rich in other nutrients can help prevent irritation. Here are several foods you may want to avoid if you are living with UC.
Recommended Reading: What Foods Should I Eat With Ulcerative Colitis
Should Supplemental Vitamins Be Taken If So Which Ones
Again, that depends on the extent and location of the disease. As noted above, vitamin B-12 is absorbed in the lower ileum. That means that people who have ileitis or those who have undergone small bowel surgery may have a vitamin B-12 deficiency because they are unable to absorb enough of this vitamin from their diet or from oral supplements. To correct this deficiency , a monthly intramuscular injection of vitamin B-12 may be required. Folic acid deficiency is also quite common in patients who are on the drug sulfasalazine. They should take a folate tablet, 1 mg daily, as a supplement. For most people with chronic IBD, it is worthwhile to take a multivitamin preparation regularly. If you suffer from maldigestion or have undergone intestinal surgery, other vitamins-particularly vitamin D-may be required. Affecting as many as 68 percent of people, vitamin D deficiency is one of the most common nutritional deficiencies seen in association with Crohn’s disease. Vitamin D is essential for good bone formation and for the metabolism of calcium. Supplementation of this vitamin should be in the range of 800 I.U./day, especially in the non-sunny areas of the country, and particularly for those with active disease. Together with vitamins A, E, and K, vitamin D is a fat-soluble vitamin these tend to be less easily absorbed than water-soluble vitamins. Consequently, they may be absorbed better in liquid rather than pill form.
How Does Nutrition Affect Growth
In young people with IBD who had onset of their disease before puberty, growth may be retarded. Poor food intake may further contribute to poor growth. Thus, good nutritional habits and adequate caloric intake are very important. Control of the disease with drugs or, less often, surgical removal of a particularly diseased region of intestine, is most successful when appropriate dietary intake is maintained.
Also Check: What’s The Difference Between Colitis And Ulcerative Colitis
Olive Oil Coconut Oil Omega
Fat is an important component of a balanced diet. A good quality olive oil is best for sautéing over low heat and making cold dressings or sauces.
Coconut oil is worth trying, especially if you have a difficult time digesting fat. As a medium-chain triglyceride, its more easily and more completely digested without the help of bile salts than other plant oils. For that reason, it can be a good oil for people with malnutrition and malaborption problems.
Coconut is solid at room temperature, so it is versatile and can be used like butter for both sautéing over high heat and for baking.
Omega-3 fats are important because we cannot make them in our body. They are found in nuts, avocadoes, freshly ground flaxseed, and fish. Wild salmon and sardines are preferable to other fish as a source of omega-3s because of their low heavy metal content.
Artificial trans fats should be avoided altogether because it increases the risk of developing heart disease. Trans fat is used to make crackers, cookies, and other processed food because it extends the shelf life.
Nutritional Supplements May Be Needed
Your doctor may order a blood test to see if you have any nutritional deficiencies due to ulcerative colitis. According to the Crohn’s and Colitis Foundation, people who have ulcerative colitis may not be getting the necessary nutrients from a well-balanced diet alone. Therefore, your doctor may recommend vitamin and mineral supplements such as calcium, iron, folic acid, zinc and vitamins D, B12, A, E and K.
Read Also: How Do You Know If Your Horse Has Ulcers
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
You May Like: Foods That Cure Ulcerative Colitis
More Ulcerative Colitis Diet Tips
The best approach for determining ulcerative colitis foods to eat and avoid is to use a food journal. You will soon be able to identify which foods trigger symptoms and which foods seem to help. It may also help to eat smaller meals throughout the day.
Speak to your doctor or nutritionist to get helpful recommendations that will soothe your UC and provide the most vitamins and nutrients needed for optimal health.
You can also supplement your diet with calcium, folic acid, vitamin B12, and amino acids. Heal is an essential amino acid supplement that can help to calm inflammation and accelerate recovery from illness.
Ulcerative colitis does not have a cure but you can successfully manage your symptoms, support healthy digestion and immune function, and improve your quality of life by following good nutrition principles and a well-balanced diet plan.
Up to 25% off Amino
You May Like: Symptoms Of Ulcer In Female
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Which Foods Should Be Avoided
Again, there are no blanket rules or recommendations. If a particular kind of food causes digestive problems, then try to avoid it. But it’s important to distinguish between an actual allergy to one kind of food and an intolerance. Many people have food intolerances — far more than really have true food allergies. Elimination tests are better at diagnosing which foods must be avoided or modified than the standard allergy skin or blood testing. Many good books discuss the proper way to follow such an “elimination diet,” which involves keeping a food and symptom diary over several weeks.
In fact, a food diary can not only help pinpoint which foods are troublesome for you, but it can also reveal whether or not your diet is providing an adequate supply of nutrients. By reviewing your food diary, your dietitian can see if you are getting the recommended daily allowances for a person of your age, sex, and size. If not, the dietitian can suggest ways to amend your diet so that your intake of nutrients is improved. That may mean increasing the amount of food you eat, changing what you eat, or adding supplements to your diet.
You May Like: What Does An Ulcerative Colitis Flare Up Feel Like
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.