Convert E11621 To Icd
The General Equivalency Mapping crosswalk indicates an approximate mapping between the ICD-10 code E11.621 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
- – DMII oth nt st uncntrld
What Are The Symptoms Of Type 2 Diabetes
Many people with type 2 diabetes have no symptoms at all. If you do have them, the symptoms develop slowly over several years. They might be so mild that you do not notice them. The symptoms can include
- Increased thirst and urination
If you have diabetes, your blood glucose, or blood sugar, levels are too high. Over time, this can damage your nerves or blood vessels. Nerve damage from diabetes can cause you to lose feeling in your feet. You may not feel a cut, a blister or a sore. Foot injuries such as these can cause ulcers and infections. Serious cases may even lead to amputation. Damage to the blood vessels can also mean that your feet do not get enough blood and oxygen. It is harder for your foot to heal, if you do get a sore or infection.
You can help avoid foot problems. First, control your blood sugar levels. Good foot hygiene is also crucial:
- Check your feet every day
- Wash your feet every day
- Keep the skin soft and smooth
- Smooth corns and calluses gently
- If you can see, reach, and feel your feet, trim your toenails regularly. If you cannot, ask a foot doctor to trim them for you.
- Wear shoes and socks at all times
- Protect your feet from hot and cold
- Keep the blood flowing to your feet
NIH: National Institute of Diabetes and Digestive and Kidney Diseases
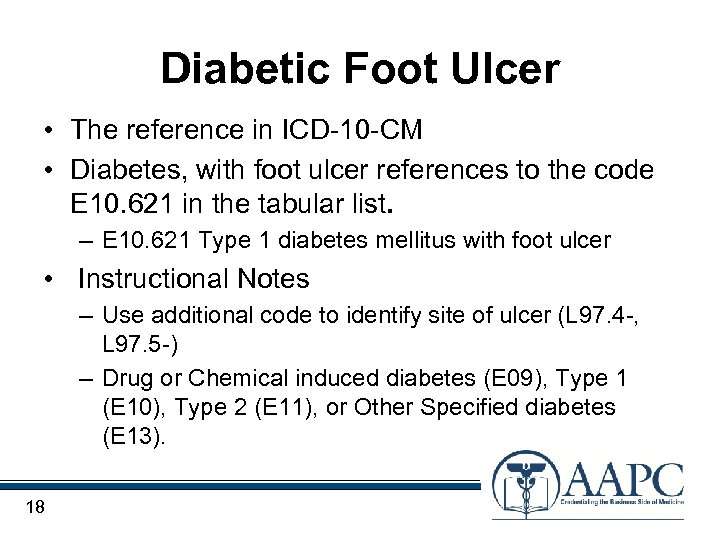
Type 2 Diabetes Mellitus With Foot Ulcer
- 2016201720182019202020212022Billable/Specific Code
- E11.621 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM E11.621 became effective on October 1, 2021.
- This is the American ICD-10-CM version of E11.621 – other international versions of ICD-10 E11.621 may differ.
“use additional code”
Read Also: Black Tarry Stools Ulcerative Colitis
Counts And Classification Of Patients With Diabetic Foot Infections
We identified 61,007 patients with one or more specific or moderately-specific codes for diabetic foot infection in inpatient records. Of these, 42,063 had specific codes that were classifiable into one of our predefined groups. Thirty-three percent of all patients had ulcer, 19.1% gangrene, 7.3% cellulitis or abscess of the foot, 6.8% osteomyelitis, 2.3% cellulitis or abscess of the toe, and 0.5% paronychia. As shown in figure , we classified the remaining 18,944 patients as having various “other” types of infection. This “other” category consisted almost entirely of patients with ICD-9-CM codes for infection of the leg but not specifically of the foot. For example, 84% of them had codes for cellulitis of the leg. They are included in our sample because infection of the foot can extend into the leg but they are not included in the evaluation of our classification system.
Statistical Methods Of The Study
Statistical data processing was performed using SPSS statistical software version 22.0. The calculation and construction of diagrams reflecting the dynamics of the studied indicators were carried out with the support of Open Office Apache 4. All digital data were processed via variation statistics using Students t-test. All studied quantitative signs of a distribution close to the normal value were presented as M ± m, where M is the arithmetic mean, and m is the standard deviation. Differences were considered statistically significant at p< 0.05, t> 2.
The receiver operating characteristic curve was used to assess the diagnostic and statistical efficiency of the proposed diabetic foot syndrome classification, considering the consequences of false decisions. The ROC curve classification of diabetic foot syndrome was used to determine the significance of the presence of diabetic foot syndrome in a patients formulated diagnosis, in which doctors can more accurately describe the diagnosis and predict the outcome of diabetic foot syndrome. In addition, ROC curves were also made using the current ICD-10 classification and compared with the proposed classification for diabetic foot syndrome.
Read Also: What Kind Of Yogurt Is Good For Stomach Ulcer
Outcomes Of Patients With Diabetic Foot Infections
Rehospitalization for foot infection
Using ICD-9-CM codes and our classification system, we determined: 1) The proportion of patients who were rehospitalized for any type of foot infection 2) The type of foot infection that was present and, 3) The number of days between admissions.
Long-term outcomes
Long-term outcomes were amputation rate, transition to long-term care, and death. We included long-term care because serious disease of the lower extremity might result in impaired ambulation and a need for nursing home care in older patients–a phenomenon that has been observed in patients who have had surgery for hip fracture. We included death because of the high frequency of co-morbid vascular disease, which is a predisposing factor for serious foot infections.
Subsequent amputations were identified by ICD-9 procedure codes from inpatient records. We also identified past amputation using the ICD-9 procedure codes along with ICD-9-CM diagnosis and CPT-4 procedure codes for post-amputation and prosthesis care we used this broader definition because it is more sensitive in identifying amputations, including those that may have occurred outside of the VA.
Deaths were identified from DEpiC, which assigns death based on an algorithm using information from the VA Beneficiary Identification and Records Locator Subsystem file, VA inpatient records, the Social Security Death Index, and Medicare records. The combination of these records has a sensitivity of 98%.
Characteristics Of The Classification Developed And Used In The Study Of Diabetic Foot Syndrome
We have developed a classification of diabetic foot syndrome that can be introduced into the ICD-10 and the ICD-11 under development.
Codes for diabetic foot syndrome adapted for the ICD-10 are proposed: Edf10.0insulin-dependent diabetes mellitus with diabetic foot syndrome and Edf11.0non-insulin-dependent diabetes mellitus with diabetic foot syndrome, where df stands for diabetic foot. The acronym df can also be used in sections E12E14 of the ICD-10 with the corresponding definitions.
In the developed classification of diabetic foot syndrome, two digits after the dot were added to the proposed codes Edf10.0 and Edf11.0: the first characterises the affected area and the second refers to the depth . Separate codes are allocated for amputations: Edf10.8amputation stump of the lower limb after non-traumatic amputation in insulin-dependent diabetes mellitus with diabetic foot syndrome, without ulcers, and Edf11.8amputation stump of the lower limb after non-traumatic amputation in non-insulin-dependent diabetes mellitus with diabetic foot syndrome, without ulcers. The letters of the English alphabet indicate the amputation level: ttoe, ffoot, llower leg and ththigh. The side of amputation and/or ulcer is designated: on the rightr and on the leftl. When a trophic defect heals, the code does not specify the depth of the lesion and its localisation.
You May Like: What To Do When You Have A Stomach Ulcer
What Causes Type 2 Diabetes
Type 2 diabetes may be caused by a combination of factors:
- Being overweight or having obesity
- Not being physically active
- Genetics and family history
Type 2 diabetes usually starts with insulin resistance. This is a condition in which your cells don’t respond normally to insulin. As a result, your body needs more insulin to help the glucose enter your cells. At first, your body makes more insulin to try to get cells to respond. But over time, your body can’t make enough insulin, and your blood glucose levels rise.
Q& a: Coding Gangrene In A Patient With A History Of Diabetes
Q: We recently had a patient with a history of diabetes admitted with gangrene of the left second toe. Can I use code L97.529 for this case?
A: Based on the limited information provided, I cannot recommend code assignment for this case but lets review a few rules related to coding and documentation that might help you.
First, if the type of diabetes is not documented by the provider, code assignment defaults diabetes mellitus type II. Ulcers of the digits of the foot are usually classified as diabetic ulcers, but if there is documentation in the medical record that would lead you to believe the ulcers are not related to the diabetes, a query may be necessary for clarification. Also, if there is any evidence in the medical record that indicates the gangrene is not related to the diabetes, query the provider.
When coding any non-pressure chronic ulcer classifiable to L97-, code first the underlying cause of the ulcer, if known, followed by the appropriate L97- code to identify the ulcer location, site, and severity. Any gangrene associated with the ulcer should also be coded first . Skin ulceration in a diabetic patient is assumed to be related to the diabetes, unless specified by the provider.
Also review Section 1.A.15 of the Official Guidelines for Coding and Reporting, which states:
The word with in the Alphabetic Index is sequenced immediately following the main term, not in alphabetical order.
You May Like: Preventing Pressure Ulcers In Nursing Homes
Type 2 Diabetes Mellitus Without Complications
Diabetes in pregnancy Diabetes mellitus diet education done Diabetes mellitus in the puerperium – baby delivered during current episode of care Diabetes mellitus type 2 Diabetes mellitus type 2 without retinopathy Diabetes type 2 Diabetes type 2 controlled with diet Diabetes type 2 on insulin Diabetes type 2, uncomplicated Diabetes type 2, without retinopathy Diabetic foot exam Diabetic foot exam done Dietary diabetic patient education Gestational diabetes mellitus Insulin treated type 2 diabetes mellitus Insulin-treated non-insulin-dependent diabetes mellitus Maturity onset diabetes mellitus in young Maturity onset diabetes of youth Maturity-onset diabetes of the young Nutrition therapy for diabetes type 2 done Nutritional therapy for diabetes mellitus type 2 Postpartum diabetes Preexisting diabetes mellitus during postpartum Preexisting diabetes postpartum Type 2 diabetes mellitus Type 2 diabetes mellitus controlled by diet Type 2 diabetes mellitus without complication Type ii diabetes mellitus without complicationContinue reading > >
Who Is At Risk For Type 2 Diabetes
You are at higher risk of developing type 2 diabetes if you
- Are over age 45. Children, teenagers, and younger adults can get type 2 diabetes, but it is more common in middle-aged and older people.
- Have prediabetes, which means that your blood sugar is higher than normal but not high enough to be called diabetes
- Had diabetes in pregnancy or gave birth to a baby weighing 9 pounds or more.
- Have a family history of diabetes
- Are overweight or have obesity
- Are Black or African American, Hispanic/Latino, American Indian, Asian American, or Pacific Islander
- Are not physically active
- Have other conditions such as high blood pressure, heart disease, stroke, polycystic ovary syndrome , or depression
- Have low HDL cholesterol and high triglycerides
- Have acanthosis nigricans – dark, thick, and velvety skin around your neck or armpits
You May Like: History Of Ulcerative Colitis Icd 10
The Study Population And Source Data
This retrospective observational study was approved by the Institutional Review Board of the Edith Nourse Rogers VA Medical Center in Bedford, Massachusetts. It was conducted in the population of diabetic patients receiving care from the Veterans Health Administration from 1998 through 2004. Our data came from the national VA Diabetes Epidemiology Cohorts , a linked, computerized research database that serves as a registry of virtually all VHA patients with diabetes. It contains patient-level data on medical visits, pharmacy and laboratory data, with diagnoses and procedures for VA and non-VA care .
Diseases Of The Skin And Subcutaneous Tissuetype 2 Excludes

Don’t Miss: Are Ulcerative Colitis And Ibs The Same
Proportions Of Patients With Co
The types and proportions of co-infections are shown in Table . By definition, patients with a given infection cannot have any co-existing infections that are more severe, but may have those that are less severe.
Table 1 Coexisting Infections in Patients hospitalized for Diabetic Foot Infections
As expected, patients with different types of infection are identified as having different types of procedures. Those with cellulitis or abscess of the foot or toe most commonly have incision and drainage, while those with osteomyelitis most commonly have excisional debridement. Patients with gangrene undergo vascular radiographic studies and have amputation more frequently than others.
The table also shows that patients with paronychia have a length of stay disproportionately long for such a mild infection. They also have a more than two-fold increase in the prevalence of alcohol addiction and psychiatric treatment compared to the other patient groups . These findings are concordant with the likelihood that paronychial infection developed while the patient was in hospital for other reasons.
Codes For Amputation Involving The Lower Extremity
Current amputations :84.11-17
Past amputations : V49.71-77 V52.1 : 27888, 28800, 28801, 28802, 27803, 28804, 28805, 27290, 27598, 27880, 27881, 27882, 27884, 27885, 27886, 27590, 27591, 27592, 27290, 27291, 27292, 27293, 27294, 27295, 27594, 27595, 27596, 26910, 28810, 28811, 28812, 28813, 28814, 28815, 28816, 28817, 28818, 28819, 28820, 28821, 28822, 28823, 28824, 28825
Recommended Reading: How Do You Heal An Ulcer
E119 Type 2 Diabetes Mellitus Without Complications
NEC Not elsewhere classifiableThis abbreviation in the Tabular List represents other specified. When a specific code is not available for a condition, the Tabular List includes an NEC entry under a code to identify the code as the other specified code.
NOS Not otherwise specifiedThis abbreviation is the equivalent of unspecified.
This note further define, or give examples of, the content of the code or category.
List of terms is included under some codes. These terms are the conditions for which that code is to be used.The terms may be synonyms of the code title, or, in the case of other specified codes, the terms are a list of the various conditions assigned to that code.The inclusion terms are not necessarily exhaustive. Additional terms found only in the may also be assigned to a code.
Certain conditions have both an underlying etiology and multiple body system manifestations due to the underlying etiology.For such conditions, the ICD-10-CM has a coding convention that requires the underlying condition be sequenced first, if applicable, followed by the manifestation.Wherever such a combination exists, there is a use additional code note at the etiology code, and a code first note at the manifestation code.These instructional notes indicate the proper sequencing order of the codes, etiology followed by manifestation.
Research Ethics And Informed Consent
This study was approved by the Danish Data Protection Agency . Permission to access information from medical records without individually informed patient consent was granted by the Danish Health and Medicine Authorities in accordance with Danish law. Since this study was non-experimental and used only existing registry data, additional ethical committee approval was not required.
Don’t Miss: Ulcer Cause Blood In Stool
Documentation Details Matter For Diabetes
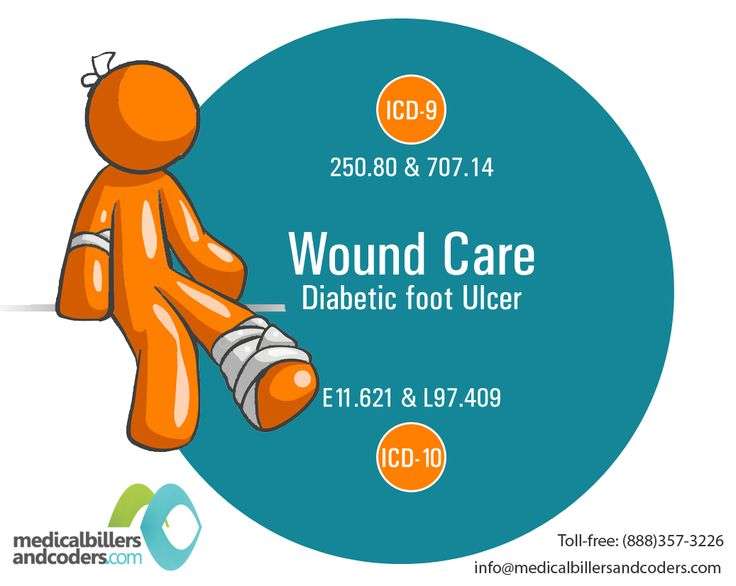
Quick, whats the ICD-9-CM code for diabetes? I bet you knew it was 250.00.
Whats the ICD-10-CM equivalent? Does ICD-10-CM even have an equivalent, since 250.00 is very vague?
Yes, we do have a default code in ICD-10-CM for those times the physician just doesnt document anything more than diabetesits E11.9. Just like 250.00, E11.9 doesnt really tell us much.
ICD-10-CM includes a greater number of codes for diabetes than ICD-9-CM . Many of the ICD-10-CM diabetes codes are combination codes that include information about the patients diabetes as well as any complications or manifestations. Obviously, E11.9 doesnt include a lot of detail.
ICD-10-CM divides diabetes into five categories, up from the two we currently have in ICD-9-CM:
- E08, diabetes mellitus due to underlying condition
- E09, drug- or chemical-induced diabetes mellitus
- E10, type 1 diabetes mellitus
- E11, type 2 diabetes mellitus
- E13, other specified diabetes mellitus
Im not sure why ICD-10-CM skips category E12. Maybe they are leaving it for possible code expansion.
ICD-10-CM diabetes codes include subcategories for:
- Ketoacidosis
- Neurological complications
- Circulatory complications
If Erin has poorly controlled type 2 diabetes, you would report E11.65 .
Suppose Erin also had a diabetic foot ulcer. We would also code E11.621 .
That gives us code L97.412 .
– See more at:
-
Neurological complications
-
Circulatory complications
What Is Type 2 Diabetes
Type 2 diabetes is a disease in which your blood glucose, or blood sugar, levels are too high. Glucose is your main source of energy. It comes from the foods you eat. A hormone called insulin helps the glucose get into your cells to give them energy. If you have diabetes, your body doesn’t make enough insulin or doesn’t use insulin well. The glucose then stays in your blood and not enough goes into your cells.
Over time, having too much glucose in your blood can cause health problems. But you can take steps to manage your diabetes and try to prevent these health problems.
Don’t Miss: How Do You Get Ulcers In Your Stomach
The Painful Dpn Validation Cohort The Non
Next, we restricted the painful DPN population, the non-painful DPN population and the diabetic foot ulcer population to those with a diagnosis in the Central Denmark Region between January 1, 2009 and July 10, 2016 . Patients who had been seen at any department of neurology/neurophysiology, mixed internal medicine, endocrinology, dermatology, vascular surgery, plastic surgery, or orthopedic surgery, at one university hospital and four regional hospitals were randomly listed in each population and the 60 first-listed individuals in each population constituted the painful DPN validation cohort, the non-painful DPN validation cohort, and the diabetic foot ulcer validation cohort, respectively.
Quality Payment Program Measures
When code E11.621 is part of the patient’s diagnoses the following Quality Measures apply and affect reimbursement. The objective of Medicare’s Quality Measures is to improve patient care by making it more: effective, safe, efficient, patient-centered and equitable.
| Quality Measure | ||
|---|---|---|
| Percentage of patients 18-75 years of age with diabetes who had hemoglobin A1c > 9.0% during the measurement period. | Effective Clinical Care | |
| Diabetes: Eye Exam | Percentage of patients 18-75 years of age with diabetes and an active diagnosis of retinopathy overlapping the measurement period who had a retinal or dilated eye exam by an eye care professional during the measurement period or diabetics with no diagnosis of retinopathy overlapping the measurement period who had a retinal or dilated eye exam by an eye care professional during the measurement period or in the 12 months prior to the measurement period. | Effective Clinical Care |
Read Also: Children’s Mouth Ulcers Treatment