To Treat Or Not To Treat
Because Crohns is usually painful and is associated with complications including bowel perforation, anemia and malnutrition, patients are usually treated with medications to calm down the immune system and reduce the inflammation. These are powerful drugs that suppress the immune system. They are very effective at controlling the pain and destruction but can leave a patient open to infection. Because of that, its less clear how to treat patients with asymptomatic disease. For those with no pain and no signs of inflammation, watchful waiting is a common strategy.
The same type of medications are used to treat the arthritis associated with inflammatory bowel disease. The physician wasnt sure if it made sense for him to use an immune-suppressing medicine while seeing sick patients. His rheumatologist, seeing him put the pad on his seat before gently lowering himself onto the chair, was much less uncertain. She had put many people on these medications, she told him some of them doctors. Most did fine. He agreed to start taking it. The effect was immediate and amazing. His pain a regular visitor for nearly a decade is gone. Even at the end of the day, his walk to and from his car is painless. He still uses the pad at times those bones are still a little tender. But the rest of him feels great.
Diagnosing Back Pain In Ulcerative Colitis
Diagnosing back pain as a symptom of ulcerative colitis can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their UC. Whats more, back pain may develop years before UC does, making it more challenging to note the connection between the two.
If your doctor suspects that your UC has led to axial arthritis or ankylosing spondylitis, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also commonly used to diagnose axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. An MRI scan can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Living With Uc: Diet Changes
Diet doesnt cause ulcerative colitis, but some foods may make your symptoms worse. Common culprits include dairy, fatty foods, and too much fiber, which can trigger diarrhea. You may find it helps to keep a journal of what you eat and any symptoms you have. Look for links and try avoiding suspected triggers. If you lose a lot of weight, you may need to work with a dietitian to come up with a high-calorie diet.
Recommended Reading: Diet For Gerd And Ulcers
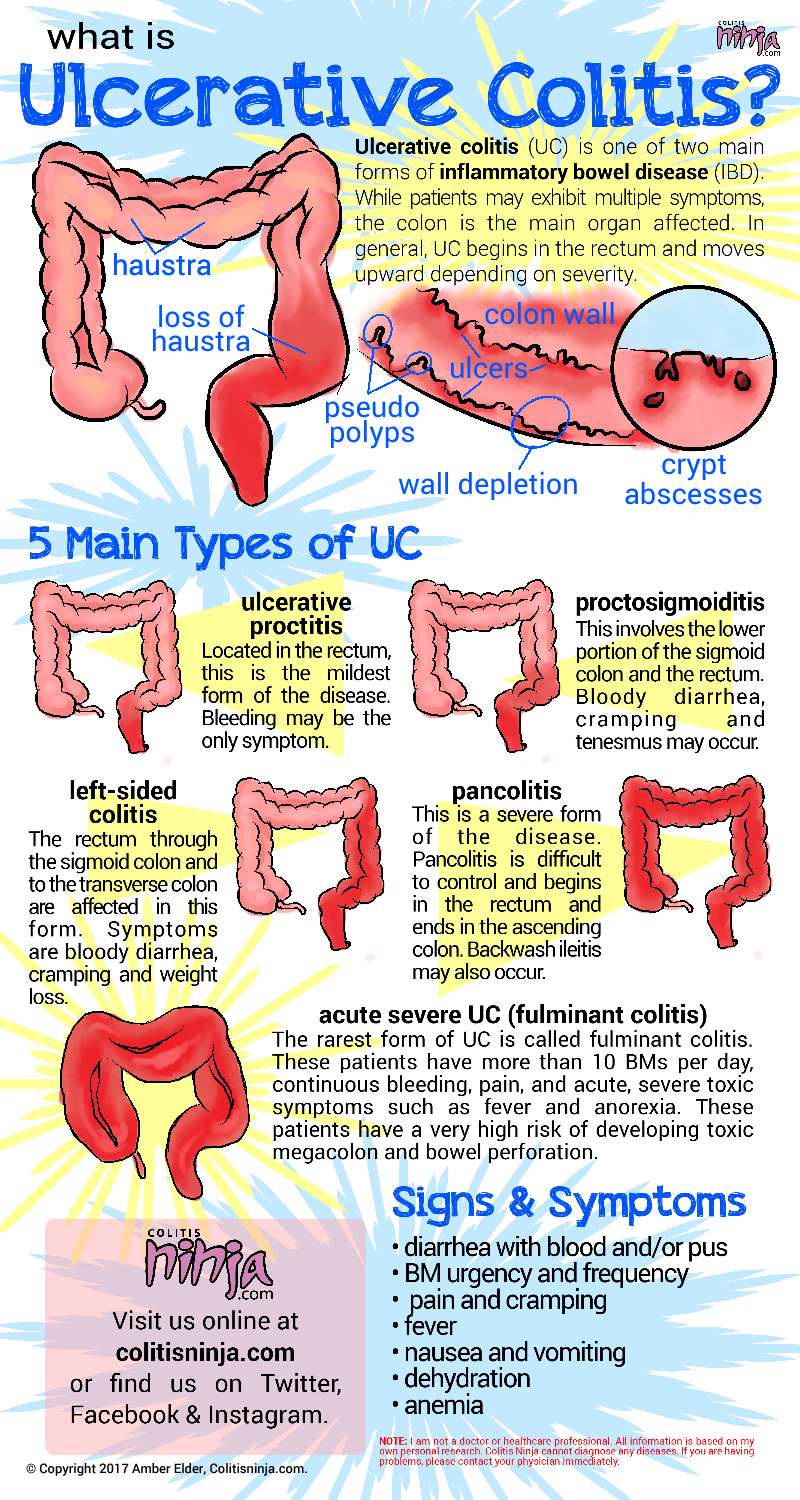
What Is Ulcerative Colitis
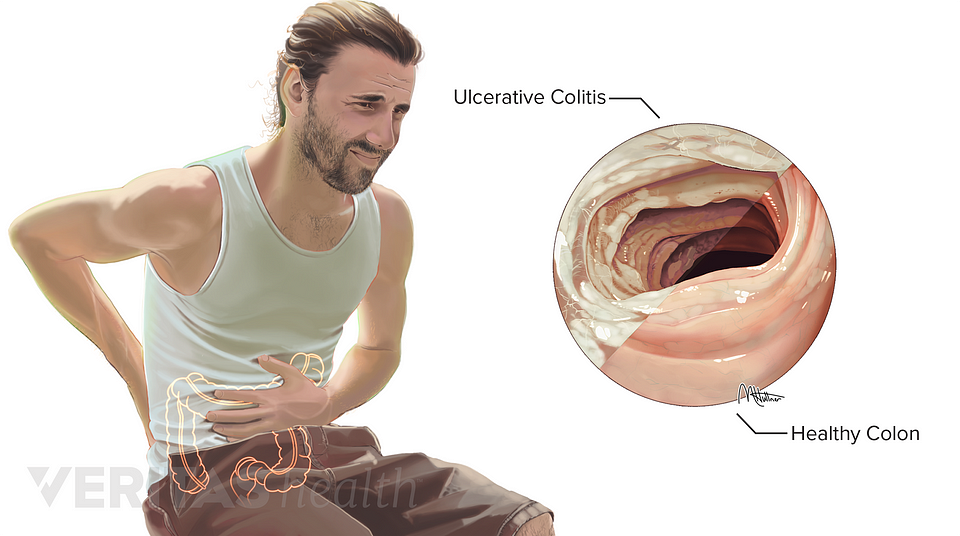
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
A Hidden Underlying Disease
Crohns disease is an autoimmune disorder in which antibodies, the bodys chief defense against infection, mistakenly attack the digestive tract as if it were a foreign invader. Although it can affect the G.I. tract anywhere, it is most frequently found in the terminal ileum. Most patients with Crohns will have pain and diarrhea but not all. In studies of patients with known Crohns disease, one in six will have no symptoms at all.
The biopsy results came back consistent with Crohns. So did blood tests designed to help diagnose inflammatory bowel disease. But it wasnt the diseased bowel that was giving the man the pain in his buttocks. It was an associated disorder, a type of arthritis known as sacroiliitis an inflammation of the joint between the pelvic girdle and the sacrum, the triangular bone that forms the connection between the hips. Although the reason this happens is not well understood, it appears that some of the immune cells misdirected to attack the gut can also attack the joints. Up to 39 percent of patients with an inflammatory bowel disease develop arthritis in some form. And up to 20 percent will develop the arthritis before getting the bowel disease. In this patients case, its hard to know which came first, because the bowel disease was discovered almost by accident.
Recommended Reading: What Causes Ulcers On The Feet
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
Lying Lateral Leg Lifts
Lie on your side and also use a towel or flat pillow to fill the void in between your stomach as well as the floor can assist also. Do this exercise with your back to a wall and also place your lower foot flat versus the wall if you can. Lower Left Back Pain Ulcerative Colitis
Maintain a small ahead tilt of the hips and also use your hand to quit you from rocking forwards. Inhale, and, as you take a breath out, raise your uppermost leg. Guarantee you do not twist your foot to direct upwards.
Don’t Miss: Doctors Specializing In Ulcerative Colitis
Herbal And Alternative Treatments
Cannabis research increasingly points to benefits for a range of chronic health conditions, but there is minimal evidence specific to ulcerative colitis at this time. Studies so far suggest the potential of cannabis to improve the quality of life for people with UC, likely due to its anti-inflammatory and antioxidant effects. More investigation is needed before recommendations can be made.
Other studies show that, compared to placebo, the treatments of aloe vera gel, wheatgrass juice, andrographis paniculata extract, and topical Xilei-san may all help alleviate UC symptoms. Before experimenting with any alternative treatments, you should always consult with your health care provider.
Ulcerative Colitis: How Do You Tell It Apart From Crohns Disease
The symptoms of ulcerative colitis are similar to another form of inflammatory bowel disease called Crohns. The difference is that UC happens only in your large intestine. Crohns can occur in various places throughout your digestive tract, so you may get symptoms anywhere from the anus to the mouth. Irritable bowel syndrome is another disorder known for long-term belly pain and diarrhea, but it doesnt cause inflammation or sores in the intestines.
Don’t Miss: What Is Moderate Ulcerative Colitis
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Ial Crunches Lower Left Back Pain Ulcerative Colitis
Some workouts can exacerbate back agony and also needs to be prevented when you have severe low pain in the back. Partial crunches can help enhance your back as well as tummy muscles. Lie with knees curved and also feet flat on the floor. Cross arms over your chest or put hands behind your neck.
Tighten abdominal muscle and elevate your shoulders off the flooring. Take a breath out as you raise your shoulders. Do not lead with your joints or utilize arms to pull your neck off the flooring. Hold for an instant, then slowly lower back down. Repeat 8 to 12 times.
Proper kind avoids too much stress and anxiety on your low back. Your feet, tailbone, and also lower back must continue to be in call with the floor covering whatsoever times.
Also Check: Ulcers In Small Bowel Crohn’s
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
Recommended Reading: Do Ulcers Cause Weight Loss
Colitis And Sacroiliac Pain
What is the relationship between colitis and sacroiliac pain? Doctors have been busy studying the increasing evidence showing a definite link between certain types of sacroiliac joint pain and various lower bowel issues, like irritable bowel syndrome and ulcerative colitis.
There can be many possible reasons for sacroiliac joint pain and most people with SIJ symptoms will not develop colitis. However, scientists have seen enough proof that some sacroiliac symptomology can be an early manifestation of colitis and other autoimmune disorders of the lower bowel.
This short discussion takes a look at what we know about the link between colitis and sacroiliac joint pain. We will explore several scenarios commonly seen by doctors who treat both disorders.
Also Check: How To Check A Horse For Ulcers
Lower Back Pain With Ulcerative Colitis
Lower back pain and its relationship to inflammatory bowel disease has been talked about fairly often in our community. While there is no one reason for experiencing lower back pain , you are not alone if you experience this type of pain along with your Crohns disease or ulcerative colitis.
Before I continue, I want to reiterate that I am not a medical professional and if you are having this type of pain, I do highly suggest you bring it up to your doctor. There is often a reason for this pain that may require medical attention so I dont suggest waiting, if possible.
Recommended Reading: Best Treatment For Diabetic Foot Ulcer
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
Is This Pain Normal
Having said that, lower back pain is common among IBD patients so believe me, you are not abnormal. Your GI has likely had many patients with this symptom.
You will do whatever necessary to figure out the root cause and you will be okay. I am not trying to mitigate the pain, frustration, confusion, and mental angst that goes along with this unspecified symptom. I just want you to know you are not alone.
I know so many of us feel as though our bodies are so complex that no one understands us. I feel that way so often and it is scary. Really scary.
I get it.
Recommended Reading: How To Prevent Skin Ulcers
Diagnostic Tests/lab Tests/lab Values
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
Can Ulcerative Colitis Cause Nausea
People may experience mild to severe nausea as a symptom of ulcerative colitis. Changing dietary and eating habits can help manage nausea. There are also medications doctors can recommend to ease feelings of nausea. Alternative therapies, such as medical cannabis, may also help.
In some cases, severe nausea may cause vomiting or loss of appetite, which may lead to malnourishment, fatigue, and weight loss.
In this article, we will look at the link between ulcerative colitis and nausea. We will also list different types of treatment that might help a person manage nausea and other related symptoms.
Ulcerative colitis can cause nausea. People may also experience vomiting, fatigue, loss of appetite, and weight loss. Symptoms can vary between people and can depend on the severity and location of inflammation in the body.
According to the National Institute of Diabetes and Digestive and Kidney Diseases , people are more likely to experience nausea and vomiting if they have severe ulcerative colitis or if the condition involves more of the large intestine.
However, a stricture may also cause nausea, along with vomiting and constipation. A stricture happens when scar tissue builds up and narrows the intestine, causing a blockage.
Also Check: Crohn’s Versus Ulcerative Colitis Pathology
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.