Research And Statistics: How Many People Have Ulcerative Colitis
People of European descent have a higher risk of developing ulcerative colitis than do those of African or Hispanic descent.
People of European Jewish descent have an especially high risk.
Ulcerative colitis tends to run in families, affecting men and women equally overall. But older men are more likely to develop it than older women, according to the Crohns and Colitis Foundation.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Also Check: Stomach Ulcer And Chest Pain
Rapid Remission & Response At Week 8
In two pivotal UC trials, patients treated with HUMIRA achieved rapid remission* at Week 8.
ULTRA 1: Remission for Total Population at Week 8 All Patients Were Bionaïve1
18.5%
P< 0.05
ULTRA 2: Remission for Total Population at Week 8 Patients Were Bionaïve and Bioexperienced1
16.5%
Limitation of Use: The effectiveness of HUMIRA has not been established in patients who have lost response to or were intolerant to TNF blockers.1
ULTRA 1 Study Design Intro: 8-week, randomized, double-blind, placebo-controlled study in 390anti-TNF-naïve adult patients with inadequate response to concurrent or prior immunosuppressant therapy and evaluated 3 treatment arms. Primary endpoint: percentage of patients achieving clinical remission at Week 8.1,2
ULTRA 2 Study Design Intro: 52-week, randomized, doubleblind, placebo-controlled study in 518 adult patients with inadequate response to concurrent or prior immunosuppressant therapy, as well as patients who lost response or were intolerant to anti-TNF agents.§ Two treatment arms were evaluated. Co-primary endpoints: percentage of patients achieving clinical remission at Weeks 8 and 52.1,3
TNF=tumor necrosis factor
Are There Any Special Dietary Requirements For Persons With Ulcerative Colitis
Although it seems plausible that a specialized diet might benefit patients with ulcerative colitis, there is actually no evidence to support treatment with dietary modification. Despite extensive research, no diet has been found to slow progression, treat, or cure the disease. It is recommended that patients stay on a balanced, healthy diet rich in fruits, vegetables, grains, lean meats, beans, fish, eggs, nuts. Patients should also try to limit foods with saturated fatshigh cholesterol. During flare-ups, patients should continue to eat as tolerated. The Crohn’s and Colitis Foundation of America recommends a bland diet with soft food during a flare including hot cereals, boiled eggs, mashed potatoes, steamed vegetables, canned or cooked vegetables to minimize discomfort.
Read Also: How To Cure Tongue Ulcer
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Experimenting To Find Out What Can Or Cannot Work For Me
Ive had IBD for five years now and Im slowly learning that I need to adapt and work with my body each day rather than oppose blanket rules. So if youre reading this article, Id encourage you towork with your body too and slowly experiment to see what you can tolerate.
Of course, chronic illness or not, alcohol daily is not great for any of us. But its important that we also try to live our lives and not beat ourselves up about our decisions and indulging occasionally
Of course, I should add as a final note, working with yourself is great but working with your doctor is just as important. With some of the medications we take, we must make sure no alcohol passes our lips at all. And, if we are in a flare, than any kind of alcohol is likely to make it worse.
Id love to hear about your experiences with IBD and drinking.
Have you managed to find a solution that works for you or have you just given it up altogether? Is it just me who finds some types of alcohol can impact me much more than others? And finally, does anyone else just really miss wine? Do let me know below!
Read Also: History Of Ulcerative Colitis Icd 10
Key Points About Ulcerative Colitis In Children
-
Ulcerative colitis is an inflammatory bowel disease. In this condition, the inner lining of your childs large intestine and rectum gets inflamed.
-
This inflammation causes diarrhea or frequent emptying of the colon. Your child may also have stomach pain and diarrhea.
-
Treatment may include avoiding foods that cause symptoms, taking medicine, and having surgery.
-
Children with this condition need long-term care. Your child may have times when symptoms go away. But symptoms usually come back.
Data Hunter Series: Uc Efficacy
Dr. Casey Chapman hosts three UC experts to discuss clinical trial data and additional analyses in bionaïve and bioexperienced UC patients.
Did you enjoy this video? See Data Hunter Dr. Casey Chapman talk with fellow experts about UC safety
Weeks 2, 4, 6,& 8
Remission* for Total Population at Weeks 2, 4, 6, & 8 per Partial Mayo Score All Patients Were Bionaïve2,4
- HUMIRA 160 mg/80 mg/40 mg EOW
- Control
Clinical remission per partial Mayo score over time in the ITT-A3 population .
Statistical Considerations: Post-hoc analyses are not powered or tested to demonstrate a statistically significant difference in treatment effect no statistical inferences can be made due to the exploratory nature of the analysis.
Post-hoc Analysis Methodology: The post-hoc analysis is of the intention-to-treat study population of patients treated with HUMIRA EOW or placebo who achieved clinical remission per partial Mayo score at Week 8. Patients with missing data were classified as not achieving clinical response or clinical remission.
EOW=every other week ITT-A3=intention-to-treat-Amendment 3
*Clinical remission was defined as a total Mayo score of 2 with no subscore > 1.Clinical response is defined as a decrease in total Mayo score of 3 points from baseline and a decrease in total Mayo score of 30% from baseline and a decrease in the rectal bleeding score of 1 or an absolute rectal bleeding score of 0 or 1.
Response* at Week 8 per Full Mayo Score3,
Don’t Miss: Diabetic Foot Ulcer Treatment Guidelines
You Need An Adjustment Of Your Meds
Antibiotics for an infection outside of your gut could aggravate UC symptoms. Let your doctor know if you start to experience diarrhea after starting antibiotics, since a switch in the type of drug might be needed.
Your doctor may also suggest taking an antidiarrheal medication or a probiotic, which may help reduce diarrhea.
What Is The Life Expectancy With Ulcerative Colitis Topic Guide
Read Also: L Glutamine Ulcerative Colitis Dosage
Golimumab Versus Infliximab Versus Adalimumab Versus Vedolizumab
Because of lack of direct comparative studies between the various biological agents in the treatment of ulcerative colitis with moderate to severe activity, a meta-analysis indirectly compared these agents . Five RCTs were included to assess the efficacy of golimumab , infliximab , and adalimumab in the treatment of moderate to severe active UC in adult patients without prior anti-TNF therapy. The outcomes evaluated included clinical response, clinical remission, mucosal healing after induction therapy , maintenance therapy , as well as clinical response and sustained remission 2121. Thorlund K, Druyts E, Toor K, Mills EJ. Comparative efficacy of golimumab, infliximab, and adalimumab for moderately to severely active ulcerative colitis: a network meta-analysis accounting for differences in trial designs. Expert Rev Gastroenterol Hepatol 2015 9:693-700. PMID: 25763862.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Recommended Reading: How To Eat With A Stomach Ulcer
Practical Implications For Clinicians And Patients And Goals For Future Trials Of Uc Therapies
In this review of clinical trials assessing advanced therapies for the treatment of moderate to severe UC, we noted several important aspects of trial design that should be accounted for when evaluating trials, including: differences in disease characteristics of the trial populations exposure to previous UC therapies and permitted concomitant therapies progression of patients between induction and maintenance phases of therapy and the endpoints used to determine efficacy. Although patients and clinicians often focus on absolute rates of response, our overview suggests that failing to account for these differences may be misleading. Accordingly when evaluating efficacy outcomes across trials, placebo-adjusted response rates, numbers needed to treat, and/or risk ratios may allow for more meaningful efficacy comparisons than comparing absolute efficacy responses. Though network meta-analyses comparing therapies for moderate to severe UC have been conducted, limitations of such comparisons have highlighted the need for randomised comparative efficacy trials.,
Are There Positive Effects Of Drinking Alcohol
To complicate matters further, while drinking alcohol clearly has some very negative effects on health, and on the GI tract, in particular, there are potential positive effects. In addition to the psychological and social benefits of the occasional drink at parties, moderate amounts of alcohol may have some health benefits. Studies have indicated that moderate drinking may have a positive effect on the coronary system and help prevent coronary artery disease.
Don’t Miss: How To Stop Ulcers From Hurting
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Don’t Miss: How To Know You Have A Ulcer
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
What Is Ulcerative Colitis In Children
Ulcerative colitis is an inflammatory bowel disease . In this condition, the inner lining of your childs large intestine and rectum gets inflamed. This inflammation often starts in the rectum and lower intestine. Then it spreads to the whole colon.
This causes diarrhea or frequent emptying of the colon. As cells on the surface of the lining of the colon die and fall off, open sores form. This causes pus, mucus, and bleeding.
Don’t Miss: Can You Eat Oatmeal With Ulcerative Colitis
Newly Identified Protein May Help Diagnose Ulcerative Colitis
An international research collaboration has discovered a potential new diagnostic marker for ulcerative colitis in a trans-ethnic analysis of Japanese and white patients. The finding could lead to the development of non-invasive, diagnostic blood test to both identify the disease and to determine progression in patients, according to the researchers.
They published their findings on December 27, 2021, in Clinical Gastroenterology and Hepatology.
More than five million worldwide suffer from inflammatory bowel disease, a catch-all descriptor for a class of disorders that includes ulcerative colitis and Crohn’s disease. Both diseases cause significant pain, diarrhea and bleeding, the result of inflammation and lesions along the large intestine. Despite the prevalence of IBD, diagnosis currently requires extensive, invasive testing, including colonoscopies, endoscopic ultrasounds and more. Symptoms can be managed, but not cured, and the cause is unknown.
“We found that patients with inflammatory bowel disease, especially ulcerative colitis, have high levels of antibodies programmed to target endothelial protein C receptors,” said first author Yoichi Kakuta, associate professor, Division of Gastroenterology at Tohoku University Hospital.
Next, the researchers plan to clarify the mechanism underpinning how the antibody is involved with the development of ulcerative colitis, with the goal of developing a diagnostic blood test and treatment options.
How Are Ulcerative Colitis And Crohn’s Disease Similar
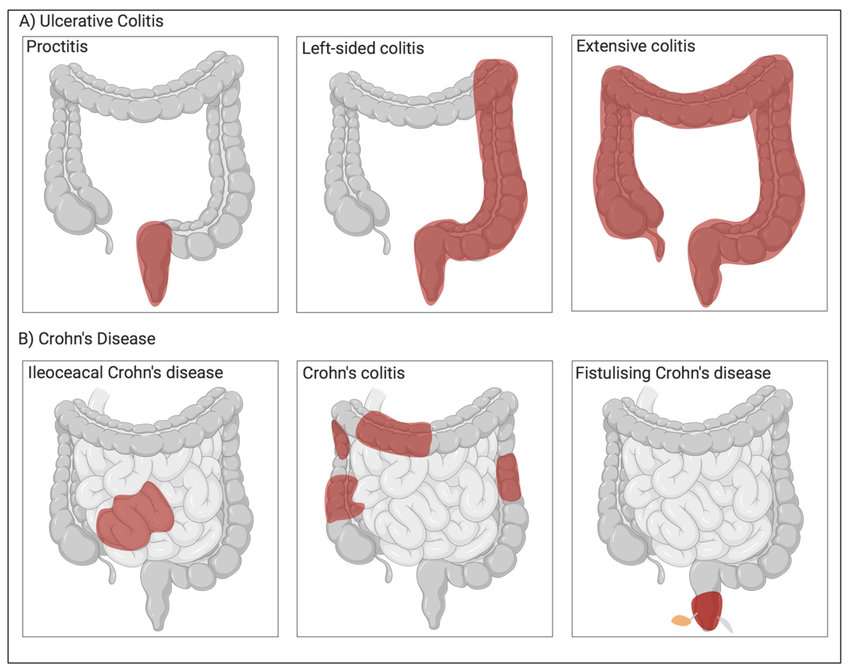
- Both diseases often develop in teenagers and young adults although the disease can occur at any age
- Ulcerative colitis and Crohn’s disease affect men and women equally
- The symptoms of ulcerative colitis and Crohn’s disease are very similar
-
The causes of both UC and Crohn’s disease are not known and both diseases have similar types of contributing factors such as environmental, genetic and an inappropriate response by the body’s immune system
Also Check: Is Milk Good For Ulcers