Rotem Sigall Boneh Rd
Rotem Sigall Boneh, RD, is a clinical and research dietitian with 8 years of experience in research in the field of dietary therapy and IBD. She graduated with honors and earned her Nutritional Science degree at the Hebrew University Jerusalem and is currently completing her Master’s Degree in Epidemiology and Preventive Medicine at Tel Aviv University, investigating the role of the Mediterranean Diet in pediatric IBD. She specializes in nutrition therapy and nutrition management for patients with IBD and is the lead dietitian in the Crohn’s Disease Exclusion Diet trials. She is the founder and former chair of D-ECCO, the dietitian committee of the European Crohn’s and Colitis organization. She actively participated in position papers and published several articles in the field of diet and IBD. She was the head of the research unit at the Pediatric Gastroenterology and Nutrition unit at the Wolfson Medical Center and was the project manager of several randomized control trials. Currently, she is a researcher and the Principal Investigator of the DIETOMICS-CD trial.
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Foods To Eat With Ulcerative Colitis
My long-term nutrition goal for my clients with ulcerative colitis is always to move towards an anti-inflammatory diet where they eat as many whole plant foods as possible. It is thought that a more Mediterranean or anti-inflammatory diet pattern contributes to an healthier community of gut bacteria, a stronger gut barrier and a better immune balance between tolerance and inflammation. In one clinical trial, a plant-based diet improved relapse rates in ulcerative colitis. Other lab research suggests that a Mediterranean-style diet decreases risk of colitis. However, because of the nature of inflammation and irritation, it can often take very slow and sustained change over time to increase intake of plant-based foods comfortably.
- Fruits and Vegetables
Fruits and vegetables have been associated with a decreased risk of ulcerative colitis. They are high in anti-inflammatory phytochemicals and fibre, which is critical for production of short chain fatty acids by our gut bacteria that help to ease inflammation and support gut barrier function.
- Omega 3 rich seeds
We all need omega 3 rich foods in our daily diet ulcerative colitis is no exception. Data suggests that increased intake of omega 3 rich foods decreases risk of ulcerative colitis but clinical trials on fish oils have not offered conclusive benefits to disease outcomes.
- Calcium- and magnesium-rich foods
- High Fibre Foods, as tolerated
- Turmeric
- Psyllium
You May Like: Does Smoking Cause Ulcers After Gastric Bypass
Comprehensive Care In One Location
Our newly designed, state-of-the-art center offers the comfort and convenience of receiving all of your care in one dedicated space. You can see your gastroenterologist or surgeon, receive an infusion, or participate in one-on-one counseling or a support group at a single location. Our spacious and private infusion bays can accommodate visitors and are equipped with warmed blankets and televisions. In addition, a quiet room is available for meditation.
In addition to our East 33rd Street location, our experts provide care at other locations in Manhattanincluding the Joan H. Tisch Center for Womens Health, NYU Langone Ambulatory Care West Side, the Preston Robert Tisch Center for Mens Healthand on Long Island at NYU Langone Nassau Gastroenterology Associates.
What To Eat During An Ulcerative Colitis Flare Up

When youre in a flare, the most important thing to do is follow your doctors advice and avoid high fibre, irritating foods. For my clients who are already plant-based, this can take some work to lessen fibre while maintaining your nutrient intake. You may need doctor-supervised bowel rest, where nutrition is provided via other means. Or, you may need a low residue diet until the flare subsides.
However, you may also be advised to simply eat whatever you can if this is the case, I find is that so often, the foods chosen are not very healthy and may further the inflammatory response. So here, I recommend juicing small amounts of fruits and vegetables, and enjoying a lot of blended foods like smoothies, blended soups and easy to digest foods like noodles, nut butters, plant-based yogurts and rice.
Also Check: Can Diverticulitis Cause Ulcerative Colitis
Diet And Inflammatory Bowel Disease
by Stephanie Fade / Dietitian Blog Posts
Diet and Inflammatory Bowel Disease. The two most important things Ive learnt.
For world IBD day here are the 2 most important things I have learnt from science and from over 20 years experience as a dietitian about diet and Inflammatory Bowel Disease or IBD.
How Can Our Dietitian Help
- Dietary assessment and supplementation recommendations
- Low residue diet plans if required during the active stage of the disease
- Longer term symptom management which involves identification of trigger foods and this may involve a short term Low FODMAP diet
- Longer term eating habits with focus on anti-inflammatory foods and nurturing gut microbiome diversity to support gut health
Also Check: Ulcerative Colitis And Lactose Intolerance
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
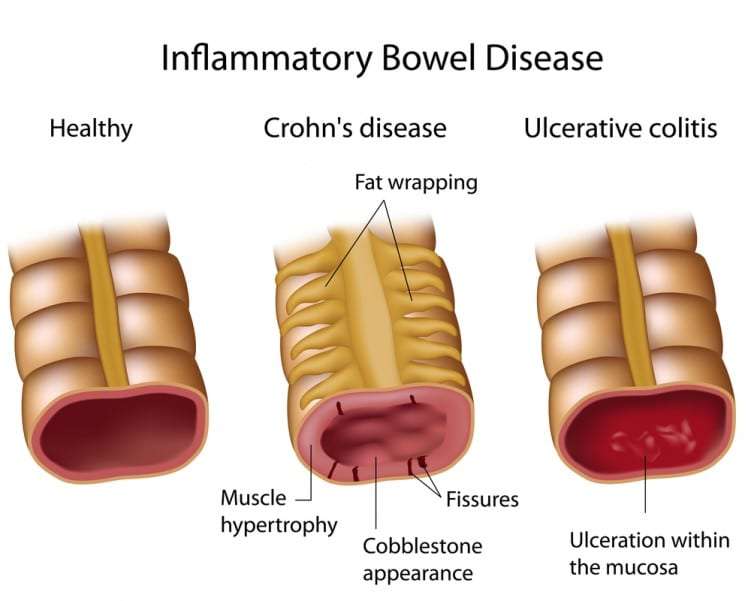
Causes Of Ulcerative Colitis
While ulcerative colitis usually begins between the ages of 15 and 30, many people over the age of 50 can also develop the disease. Thought to be an autoimmune disease, the cause of ulcerative colitis is unknown, yet there is a tendency for patients with ulcerative colitis to have a close family relative with the same disease. Stress and other environmental factors may aggravate symptoms of ulcerative colitis, they are not the cause of the disease.
Read Also: Wound Vac For Pressure Ulcers
Ibd Research And Clinical Trials
The University of Michigan Inflammatory Bowel Disease Center is nationally recognized for clinical and laboratory research. The majority of our referrals are patients who have already tried the treatment options available for IBD and are looking for the very newest therapies they cant get anywhere else. We have multiple open clinical trials investigating new therapies and diagnostics for Crohns disease and ulcerative colitis for those who qualify. Learn more at IBD Clinical Trials and Research.
Director Of Internal Operations
Alli has a Bachelor of Science in Business Administration with a concentration in Entrepreneurship from Marist College. Alli is our operational and office manager. Alli has been with CrohnColitisLifestyle since 2016 starting as an intern. Alli is committed to providing an excellent experience to our clients through their time with us on the administrative side of their program. While attending Marist College Alli received many awards in multiple business plan competitions for her work re-designing the Ostomy bag and has a true passion for helping those with Crohns and Colitis.
Also Check: Different Types Of Ulcerative Colitis
How Is Ulcerative Colitis Treated
There are several approaches Dr. Aybar can use to treat your childs ulcerative colitis. Medications called aminosalicylates can help to reduce inflammation, and corticosteroids help prevent your childs immune system from attacking their colon.
Other medications called immunomodulators or TNF-alpha blocking agents also help by decreasing inflammatory reactions.
Its also important that your child eats a nutritious, well-balanced diet that contains all the nutrients they need, but excludes any food that could irritate the colon. Dr. Aybar is an expert in pediatric nutrition, and he can design an appropriate diet plan for your child.
Most children who have ulcerative colitis respond well to these treatments. However, a few children dont improve and may even deteriorate. If this is the case, surgery to remove the affected section of the colon could be the best option.
If your child has symptoms of ulcerative colitis, call Annapolis Pediatric Gastroenterology and Nutrition today, or book an appointment online.
Get Great Nutritional Support From A Registered Dietitian
If you are looking for a registered dietitian to help guide and support your efforts we suggest you work with one who has experience in the low FODMAP diet. Weve invited RDNs who have Low FODMAP related services available to offer their information here. Check back often as this list is updated monthly.
Please note that this is an informational service only and is not a promotion nor recommendation for an individual provider. We encourage you to request references from any professional medical provider you engage with.
Read Also: What Are The Symptoms Of An Ulcer In Your Stomach
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
How We Can Help: Meet Our Specialist Dietitians
Dr. Bridgette Wilson
Dr. Wilson is a gut specialist clinical and research dietitian with a wealth of clinical dietetic experience both in the NHS and private healthcare. Her award-winning PhD research on the Low FODMAP diet and Prebiotics in Irritable Bowel Syndrome and Ulcerative Colitis has given her a great depth of knowledge to help you attain good symptom control.
Sophie Medlin
Sophie has expertise in gastrointestinal and colorectal health, including specialist knowledge and skills in the management of medical conditions such as irritable bowel syndrome , colorectal dysfunction, diverticular disease and polycystic ovarian syndrome. Sophie has over 10 years experience working with the IBD community.
Pooja Dhir
Pooja Dhir is a registered specialist dietitian who has worked as a senior manager in the NHS, specialising in upper gastrointestinal and surgery. She has worked in acute hospitals, both inpatients and outpatients and has written articles for the leading medical nutrition CN magazine and is published in the Journal of Human Nutrition and Dietetics.
What to expect from your Crohns Disease, Ulcerative Colitis & Inflammatory Bowel Disease consultation
Typically, this will involve three sessions, for example:
Session 1: Assessment and dietary modifications
Session 2: Assessment of progress and reintroduction of foods to establish tolerance
Session 3: Long term nutritional management and healthy eating
Pricing
You May Like: How To Cure Gastritis And Ulcers Naturally
Why Is It Important
Malnutrition is a common problem for people with Inflammatory Bowel Disease , especially those with Crohns Disease. This is due to reduced food intake, increased nutrient requirements and increased gastrointestinal loss of nutrients, among other causes.
Thats why nutritional treatment and support are so important for patients with IBD. They are required to avoid iron deficiency, prevent osteoporosis and promote optimal growth and development for children.
In certain situations, such as for people with strictures or before an operation, there may be a need for specific dietary advice or supplementation. Enteral nutrition as primary or additional therapy can also be used to induce remission for those with active Crohns. It is often the treatment of choice for children as it avoids the use of steroids, which can affect growth.
When people have good levels of nutrition, clinical outcomes are better so its important to use validated tools to screen and support people. Its harder to pick up nutritional risk in children, but we know there is an impact on growth for 15-40% of children with IBD, so this should be monitored especially carefully. Iron deficiency is particularly common in children with IBD, along with other deficiencies including folic acid, zinc, magnesium, calcium, vitamins A, B12, D, E and K.
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
You May Like: Snack Ideas For Ulcerative Colitis
What Foods Should You Eat With Ulcerative Colitis
If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to:
In terms of specific food recommendations, go with these:
| Food Type |
|---|
Registered Dietitians Help Patients Eat Well With Ibd
Feb 26, 2020 | Sinai Health
Whether were meeting friends for a cup of coffee, celebrating a birthday with cake or seeking comfort from chicken soup, food is more than just sustenance. But for the more than 270,000 Canadians living with inflammatory bowel disease , food can also be a source of discomfort, pain and anxiety.
Mount Sinais Zane Cohen Centre for Digestive Diseases provides specialized care and surgical treatments for patients living with IBD. Julie Cepo and Jennifer Ball are Registered Dietitians who consult on patients nutritional needs including those who are hospitalized and need nutrition through intravenous fluids or a feeding tube, patients returning to eating as they prepare to go home from the hospital, and after theyve returned to the outpatient setting.
We asked Julie and Jennifer to answer some frequently asked questions about the role of diet for patients living with IBD and how a dietitian can help.
How does the relationship with food change for people living with IBD?
People living with IBD often experience symptom flare ups followed by periods of remission where they have little to no symptoms. Eating certain foods can be associated with worsening of symptoms during flare ups. This makes it hard to trust that foods may be better tolerated when the disease is in remission. A Registered Dietitian can work with patients to help them rebuild confidence and heal their relationship with food.
What role does nutrition play in managing IBD?
Also Check: What To Avoid With An Ulcer
What To Know Before Working With An Rd For Your Ibd
If youre used to in-person appointments, a virtual visit will feel very similar, says Binder-McAsey. Rather than driving to their office, though, youll talk to the RD face-to-face over a computer or smartphone.
Before you get started, here are a few things to consider.
- The dietitians location Virtual care can allow you to access healthcare located far away, but you may want to start your search locally, since some dietitians may not be able to treat out-of-state people. If you do find an RD who works out of your state, Binder-McAsey recommends reaching out to ask if they can work with you.
- Your insurance policy Ask the RD which insurance plans they take, if any. This information may also be available on their website.
- The care platform Before the pandemic, providers had to use a HIPAA-compliant platform to assure their services were secure, but that rule changed during the pandemic. Now, providers are allowed to use a variety of communication apps in an effort to expand the availability of medical services, according to the U.S. Department of Health & Human Services, including FaceTime, Facebook Messenger, Google Hangouts, Zoom, and Skype. Ask the dietitian which platform they use, and think about whether youre comfortable using it.
Research And Public Speaking
In addition to her role at Gut Nutrition, Catherine is a research fellow at University of Otago Christchurch and is an affiliate researcher at Kings College London. Her research primarily focuses on food and nutrition for people with Crohns and ulcerative colitis. Read her IBD research publications.
Catherine is an experienced public speaker. She has spoken at conferences in Europe, Australia and New Zealand and to organisations including Crohns and Colitis UK
A talk on whole food treatment for inflammation bowel disease and the Crohns disease exclusion diet. Canterbury branch of Crohns and Colitis NZ support group meeting.
Read Also: What Foods Should I Avoid With A Stomach Ulcer