What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Risk Of Bias In Included Studies
Risk of bias for all included studies is summarised in . In order to represent ‘very high’ risk of bias, we have used two columns so very high risk of bias occurs when the cell is red in the final column .
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
We judged only one of the 51 studies to be at low risk of bias and ten to have unclear risk of bias . We judged 14 studies to be at very high risk of bias, that is, to have high risk of bias for two or more domains . We assessed the rest of the studies at high risk of bias. We grouped the low and unclear categories together.
*Studies marked with an asterisk were not included in the individual network.
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
-
Applies controlled, localised negative pressure to help uniformly draw wounds closed.
-
Helps remove interstitial fluid allowing tissue decompression.
-
Helps remove infectious materials and quantifies exudates loss.
-
Provides a closed, moist wound healing environment
-
Promotes flap and graft survival.
-
Both hospital and domiciliary use.
-
Reduces hospital/dressings/nursing cost .
You May Like: Ulcerative Colitis Is It Deadly
Stages Of Decubitus Ulcers
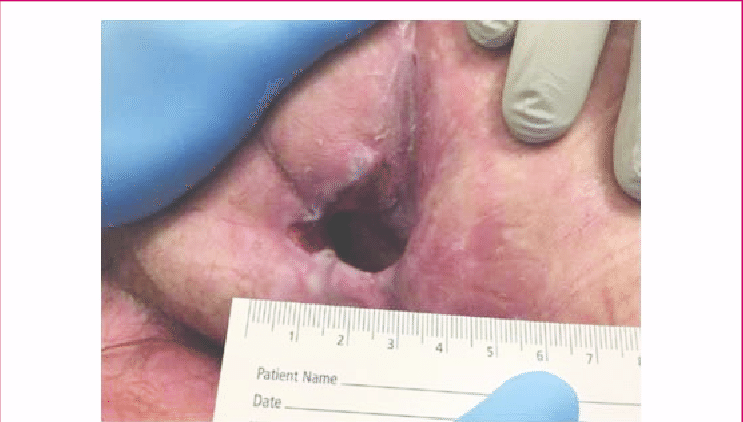
The National Pressure Ulcer Advisory Panel has developed a series of four stages of a decubitus ulcer to aid in diagnosis and treatment.Stage I: The skin is discolored but not broken. Light-complexioned people may have red marks. Dark complexioned people may have a discoloration that is blue or purple. In some people, the discoloration is white.Stage II: Skin breaks open and the ulcer is shallow with a reddish or pinkish wound bed. There may be tissue death around the wound, or a fluid-filled blister.Stage III: Ulcer on the skin is deeper, affecting the fat layer and looking like a crater. Pus may be in the wound.Stage IV: Ulcer moves to deeper layers of muscle or bone. A dark material called “eschar” may be inside the ulcer.Unstageable: An ulcer that is yellow or green. It might have a brown scab covering it, or be soft and look pus filled. A dry and stable ulcer surface is the body’s natural protection and should be allowed to continue healing. However, if extensive tissue damage is evident, the covering might need to be removed for treatment.
Histopathology Of Exposed Bone In Sacral Pressure Ulcers

Contrary to the perception that exposed bone by definition must contain osteomyelitis, several case series in which bone biopsies were conducted described histological evidence of osteomyelitis in a minority of such patients. For example, Türk et al examined histologic autopsy specimens of 28 patients with advanced-grade pressure ulcers, specifically those with visible bone . Based on the histopathologic findings, 4 distinct groups were identified. Group 1 had full thickness soft tissue disease but no inflammation of the bone, with the cortical layer of the sacrum intact. Group 2 had bone cortex involvement with increased osteoclast activity and reactive new bone formation. Group 3 had fibrotic/remodelling bony involvement without osteomyelitis changes, in the presence of suppurative soft tissue disease. Group 4 was subdivided into 6 patients with chronic osteomyelitis restricted to the superficial and subcortical aspects of the sacrum without involvement of the medullary cavity of bone, and 7 patients who had mild small confined foci of acute superimposed on chronic osteomyelitis changes without suppurative inflammation or wide destruction of bone. The highlight of these findings was that in more than half of cases osteomyelitis was not detectable histologically, whereas in cases with osteomyelitis, disease was generally more focal and superficial .
Don’t Miss: What Can I Do For Ulcers In My Stomach
Who Is At Risk Of A Pressure Ulcer
People immobile due to illness or injury are at greatest risk of getting a pressure ulcer.
- They may be unable to change position without assistance eg, see Skin complications of paraplegia and tetraplegia.
- They may have nerve damage from injury or illness, such as spina bifida, diabetes or stroke, and are unable to sense pain or the signals that normally make people move.
- Older people are at greater risk because their skin is thinner and more fragile.
- A pressure ulcer may develop underneath a plaster of Paris or fibreglass plaster .
When Sacral Ulcers Require Surgery
If you catch sacral ulcers early, then improving a persons diet and keeping them active while cleaning the wounds can reverse the damage. Once a person starts to show symptoms of Stage Three development, most medical professionals recommend surgery as the most effective curative.
To remove the dead skin that results from untreated sacral pressure, medical professionals will use the methods most appropriate for the patients situation. These methods can include:
- Biological treatment
Also Check: Can You Donate Blood If You Have Ulcerative Colitis
Deterrence And Patient Education
Patients and their family members should have a clear idea that preventing recurrence requires commitment and responsibility. They should receive education on how to manage the condition in the hospital and as well as in their homes. They should be familiar with warning signs like skin discoloration, ulceration, discharge, or a foul smell from the ulcer site and body areas with decreased or no sensation.
The patient should move or turn every 2 hours it could not be done by themselves, or they should ask someone to help them. Air or water mattress should be used in their homes too. Their food intake should be adequate and should consist of a balanced and healthy diet.
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the ‘control’ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
Don’t Miss: Pepto Bismol And Ulcerative Colitis
Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
-
absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
-
achieve freedom from particulate contaminants or toxic chemicals left in the wound
-
provide thermal insulation, in order to maintain the optimum temperature for healing
-
allow permeability to water, but not bacteria
-
optimise the pH of the wound
-
minimise wound infection and avoid excessive slough
-
avoid wound trauma on dressing removal
-
accommodate the need for frequent dressing changes
-
provide pain relief and
-
be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Recommended Reading: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
-
the proportion of wounds healed
-
time to complete healing .
You May Like: Exercising A Horse With Ulcers
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
How The Intervention Might Work
Animal experiments conducted over 40 years ago suggested that acute wounds heal more quickly when their surfaces are kept moist rather than left to dry and scab . A moist environment is thought to provide optimal conditions for the cells involved in the healing process, as well as allowing autolytic debridement , which is thought to be an important part of the healing pathway .
The desire to maintain a moist wound environment is a key driver for the use of wound dressings and related topical agents. Whilst a moist environment at the wound site has been shown to aid the rate of epithelialisation in superficial wounds, excess moisture at the wound site can cause maceration of the surrounding skin , and it has also been suggested that dressings that permit fluid to accumulate might predispose wounds to infection . Wound treatments vary in their level of absorbency, so that a very wet wound can be treated with an absorbent dressing to draw excess moisture away and avoid skin damage, whilst a drier wound can be treated with a more occlusive dressing or a hydrogel to maintain a moist environment.
Some dressings are now also formulated with an ‘active’ ingredient .
Recommended Reading: What Foods Should I Eat With Ulcerative Colitis
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
-
Ovid MEDILINE
-
Ovid MEDLINE
-
Ovid Embase
-
EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
-
ClinicalTrials.gov
-
WHO International Clinical Trials Registry Platform
-
EU Clinical Trials Register .
Searching other resources
You May Like: Compression For Venous Leg Ulcers
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.